Abstract
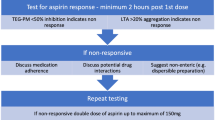
Transcatheter pulmonary valve replacement (TPVR) is a staple in the pediatric cardiac catheterization lab. Despite the ubiquitous use of this procedure, guidelines for antithrombosis post pulmonary valve replacement are non-existent. A survey was sent out via email to the members of the Congenital Cardiovascular Interventional Study Consortium (CCISC) and the Pediatric and Adult Interventional Cardiac Symposium (PICS-AICS). Responses were received from 109 cardiologists who perform this procedure. Following TPVR 76.5% of respondents use only Aspirin, while the remainder prescribe a second antithrombotic agent at discharge. The majority (78%) of respondents do not educate patients about avoiding enteric formulations of aspirin, and another 86% do not educate patients about the need to avoid proton pump inhibitors (PPI). In addition, 67% do not advise against concomitant use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). Lastly, the survey showed a wide discrepancy in prescribed dose with 56% choosing to always prescribe 70–100 mg regardless of weight, 28% choosing to do weight-based dosing, and 7.5% choosing 325 mg regardless of weight. In a survey sent out to pediatric cardiac interventionalists worldwide, a significant discrepancy was noted in antithrombotic regimens used following TPVR. We hypothesize that these discrepancies may contribute to early valve failure and suggest the need for further study and the development of unified antithrombosis guidelines following TPVR.






Similar content being viewed by others
References
Georgiev S, Ewert P, Tanase D, Hess J, Hager A, Cleuziou J, Meierhofer C, Eicken A (2019) A low residual pressure gradient yields excellent long-term outcome after percutaneous pulmonary valve implantation. JACC Cardiovasc Interv 12:1594–1603
Haas NA, Carere RG, Kretschmar O, Horlick E, Rodes-Cabau J, de Wolf D, Gewillig M, Mullen M, Lehner A, Deutsch C, Bramlage P, Ewert P (2018) Early outcomes of percutaneous pulmonary valve implantation using the Edwards SAPIEN XT transcatheter heart valve system. Int J Cardiol 250:86–91
Kenny D, Hijazi ZM, Kar S, Rhodes J, Mullen M, Makkar R, Shirali G, Fogel M, Fahey J, Heitschmidt MG, Cain C (2011) Percutaneous implantation of the Edwards SAPIEN transcatheter heart valve for conduit failure in the pulmonary position: early phase 1 results from an international multicenter clinical trial. J Am Coll Cardiol 58:2248–2256
Ghawi H, Kenny D, Hijazi ZM (2012) Transcatheter pulmonary valve replacement. Cardiol Ther 1:5
Cabalka AK, Hellenbrand WE, Eicken A, Kreutzer J, Gray RG, Bergersen L, Berger F, Armstrong AK, Cheatham JP, Zahn EM, McElhinney DB (2017) Relationships among conduit type, pre-stenting, and outcomes in patients undergoing transcatheter pulmonary valve replacement in the prospective North American and European Melody Valve Trials. JACC Cardiovasc Interv 10:1746–1759
Malekzadeh-Milania S, Ladouceura M, Patel M, Boughenoua FM, Iserin L, Bonne D, Boudjemline Y (2015) Incidence and predictors of Melody® valve endocarditis: a prospective study. Arch Cardiovasc Dis 108:97–106
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C (2020) 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. https://doi.org/10.1161/CIR.0000000000000923
Cipollone F, Patrignani P, Greco A, Rosaria Panara M, Padovano R, Cuccurullo F, Patrono C, Rebuzzi AG, Liuzzo G, Quaranta G, Maseri A (1997) Differential suppression of thromboxane biosynthesis by indobufen and aspirin in patients with unstable angina. Circulation 96:1109–1116
Antman EMAD, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr (2004) ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction. Circulation 110:588–636
Eikelboom JW, Hirsh J, Spencer FA, Baglin TP, Weitz JI (2012) Antiplatelet drugs: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e89S-e119S
Wurtz M, Grove EL, Kristensen SD, Hvas AM (2010) The antiplatelet effect of aspirin is reduced by proton pump inhibitors in patients with coronary artery disease. Heart 96:368–371
Warner TD, Nylander S, Whatling C (2011) Anti-platelet therapy: cyclo-oxygenase inhibition and the use of aspirin with particular regard to dual anti-platelet therapy. Br J Clin Pharmacol 72:619–633
Campbell CL, Steinhubl SR (2005) Variability in response to aspirin—do we understand the clinical relevance. J Thromb Hemost 3:5
Mehta SR, Tanguay JF, Eikelboom JW, Jolly SS, Joyner CD, Granger CB, Faxon DP, Rupprecht HJ, Budaj A, Avezum A, Widimsky P, Steg PG, Bassand JP, Montalescot G, Macaya C, Pasquale GD, Niemela K, Ajani AE, White HD, Chrolavicius S, Gao P, Fox KAA, YusuF S (2010) Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomised factorial trial. The Lancet 376:10
Rosseel L, De Backer O, Sondergaard L (2019) Clinical valve thrombosis and subclinical leaflet thrombosis following transcatheter aortic valve replacement: is there a need for a patient-tailored antithrombotic therapy? Front Cardiovasc Med 6:44
Gurbel PA, Bliden KP, DiChiara J, Newcomer J, Weng W, Neerchal NK, Gesheff T, Chaganti SK, Etherington A, Tantry US (2007) Evaluation of dose-related effects of aspirin on platelet function: results from the Aspirin-Induced Platelet Effect (ASPECT) study. Circulation 115:3156–3164
Dawson J, Quinn T, Rafferty M, Higgins P, Ray G, Lees KR, Walters MR (2011) Aspirin resistance and compliance with therapy. Cardiovasc Ther 29:301–307
Shantsila E, Lip GY (2008) “Aspirin resistance” or treatment non-compliance: which is to blame for cardiovascular complications? J Transl Med 6:47
Schwartz KA, Schwartz DE, Barber K, Reeves M, De Franco AC (2008) Non-compliance is the predominant cause of aspirin resistance in chronic coronary arterial disease patients. J Transl Med 6:46
Funding
No funding was required for this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work.
Corresponding author
Ethics declarations
Conflict of interest
Evan Zahn is a proctor, a consultant and a former site Principle Investigator for Medtronic. Evan Zahn is a proctor, a consultant, and a national Principle Investigator for Edwards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shibbani, K., Garg, R., Zahn, E.M. et al. Aspirin Use and Transcatheter Pulmonary Valve Replacement, the Need for Consistency. Pediatr Cardiol 42, 1640–1646 (2021). https://doi.org/10.1007/s00246-021-02652-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02652-8