Abstract
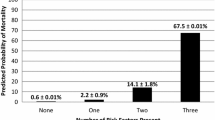
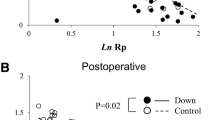
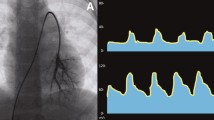
This study aimed to investigate risk factors for poor outcomes in infants with isolated atrial septal defect (ASD) and pulmonary hypertension who had unexpectedly fatal course. We retrospectively reviewed 22 infants with isolated ASD and pulmonary hypertension, and analyzed the relationship between clinical outcomes and pulmonary hemodynamic parameters including pulmonary arterial resistance (Rp) and compliance (Cp) based on cardiac catheterization among them. Age and weight at cardiac catheterization were 5 (1–11) months and 4.9 (3.1–9.2) kg, respectively. There were 17 individuals with Down syndrome. Pulmonary hemodynamic parameters were shown as follows: the ratio of pulmonary to systemic blood flow: 2.0 (0.6–3.8), mean pulmonary arterial pressure: 41 (20–60) mmHg, the ratio of pulmonary to systemic mean pressure (Pp/Ps): 0.67 (0.46–1.13), Rp: 4.11 (0.68–15.80) Wood units m2, and Cp: 1.80 (0.63–6.16) mL/mmHg m2. There were 4 deaths during the follow-up period of 40 (7–241) months. Univariable logistic regression analysis revealed that Pp/Ps (odds ratio [OR]: 18,500, 95% confidential interval [CI] 1.48–230,659,690, P = 0.041) and Cp (OR: 0.03, 95% CI 0.001–0.73, P = 0.031) were significantly related to death. A Pp/Ps cutoff value more than 0.94 and a Cp cutoff value less than 0.97 mL/mmHg m2 yielded as the predictors of death with sensitivity of 98% and 94%, specificity of 75% and 75%, respectively. Decreased Cp is a previously unrecognized predictor for poor outcome in infants with isolated ASD and pulmonary hypertension.
Similar content being viewed by others
Availability of Data and Materials
All data will be offered if applicable.
Code Availability
Statistical analysis was performed using the Analysis TollPak In the Microsoft Office Excel™ add-in software.
References
Geggel RL (2017) Clinical detection of hemodynamically significant isolated secundum atrial septal defect. J Pediatr 190:261–264.e1. https://doi.org/10.1016/j.jpeds.2017.07.037
Lammers A, Hager A, Eicken A, Lange R, Hauser M, Hess J (2005) Need for closure of secundum atrial septal defect in infancy. J Thoracic Cardiovasc Surg 129(6):1353–1357. https://doi.org/10.1016/j.jtcvs.2004.10.007
Tanghöj G, Liuba P, Sjöberg G, Rydberg A, Naumburg E (2019) Adverse events within 1 year after surgical and percutaneous closure of atrial septal defects in preterm children. Cardiol Young 29(5):626–636. https://doi.org/10.1017/S1047951119000350
Charisopoulou D, Bini RM, Riley G, Janagarajan K, Moledina S, Marek J (2020) Repair of isolated atrial septal defect in infants less than 12 months improves symptoms of chronic lung disease or shunt-related pulmonary hypertension. Cardiol Young. https://doi.org/10.1017/S1047951120000463
Lee JS, Cha SG, Kim GB, Lee SY, Song MK, Kwon HW, Bae EJ, Kwak JG, Kim WH, Lee JR (2019) Reversibility of pulmonary hypertension following surgical atrial septal defect closure in children with down syndrome. J Cardiovasc Imag 27(4):247–253. https://doi.org/10.4250/jcvi.2019.27.e33
Saji T (2014) Clinical characteristics of pulmonary arterial hypertension associated with Down syndrome. Pediatr Int 56(3):297–303. https://doi.org/10.1111/ped.12349
Takatsuki S, Nakayama T, Ikehara S, Matsuura H, Ivy DD, Saji T (2017) Pulmonary arterial capacitance index is a strong predictor for adverse outcome in children with idiopathic and heritable pulmonary arterial hypertension. J Pediatr 180:75–79.e2. https://doi.org/10.1016/j.jpeds.2016.10.003
Muneuchi J, Nagatomo Y, Watanabe M, Joo K, Onzuka T, Ochiai Y, Joo K (2016) Relationship between pulmonary arterial resistance and compliance among patients with pulmonary arterial hypertension and congenital heart disease. J Thoracic Cardiovasc Surg 152(2):507–513. https://doi.org/10.1016/j.jtcvs.2016.03.080
Okada S, Muneuchi J, Nagatomo Y, Watanabe M, Iida C, Shirouzu H, Matsuoka R, Joo K (2017) Pulmonary arterial resistance and compliance in preterm infants. Int J Cardiol 244:265–270. https://doi.org/10.1016/j.ijcard.2017.06.056
Cheng XL, Liu ZH, Gu Q, Ni XH, Luo Q, Zhao ZH, He JG, Xiong CM (2017) Prognostic value of pulmonary artery compliance in patients with pulmonary arterial hypertension associated with adult congenital heart disease. Int Heart J 58(5):731–738. https://doi.org/10.1536/ihj.16-449
Tonelli AR, Alnuaimat H, Mubarak K (2010) Pulmonary vasodilator testing and use of calcium channel blockers in pulmonary arterial hypertension. Respir Med 104(4):481–496. https://doi.org/10.1016/j.rmed.2009.11.015
Goetschmann S, Dibernardo S, Steinmann H, Pavlovic M, Sekarski N, Pfammatter JP (2008) Frequency of severe pulmonary hypertension complicating “isolated” atrial septal defect in infancy. Am J Cardiol 102(3):340–342. https://doi.org/10.1016/j.amjcard.2008.03.061
Pellegrini P, Rossi A, Pasotti M, Raineri C, Cicoira M, Bonapace S, Dini FL, Temporelli PL, Vassanelli C, Vanderpool R, Naeije R, Ghio S (2014) Prognostic relevance of pulmonary arterial compliance in patients with chronic heart failure. Chest 145(5):1064–1070. https://doi.org/10.1378/chest.13-1510
de Perrot M, McRae K, Shargall Y, Thenganatt J, Moric J, Mak S, Granton JT (2011) Early postoperative pulmonary vascular compliance predicts outcome after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension. Chest 140(1):34–41. https://doi.org/10.1378/chest.10-1263
Iwaya Y, Muneuchi J, Inoue Y, Watanabe M, Okada S, Ochiai Y (2019) Relationship Between Pulmonary Arterial Resistance and Compliance in Patients with Down Syndrome. Pediatr Cardiol 40(4):841–847. https://doi.org/10.1007/s00246-019-02080-9
Schwarz MA, Caldwell L, Cafasso D, Zheng H (2009) Emerging pulmonary vasculature lacks fate specification. Am J Physiol Lung Cell Mol Physiol 296(1):L71–L81. https://doi.org/10.1152/ajplung.90452.2008
Parera MC, van Dooren M, van Kempen M, de Krijger R, Grosveld F, Tibboel D, Rottier R (2005) Distal angiogenesis: a new concept for lung vascular morphogenesis. Am J Physiol Lung Cell Mol Physiol 288(1):L141–L149. https://doi.org/10.1152/ajplung.00148.2004
Armulik A, Abramsson A, Betsholtz C (2005) Endothelial/pericyte interactions. Circul Res 97(6):512–523. https://doi.org/10.1161/01.RES.0000182903.16652.d7
Peng T, Tian Y, Boogerd CJ, Lu MM, Kadzik RS, Stewart KM, Evans SM, Morrisey EE (2013) Coordination of heart and lung co-development by a multipotent cardiopulmonary progenitor. Nature 500(7464):589–592. https://doi.org/10.1038/nature12358
Lévy M, Maurey C, Dinh-Xuan AT, Vouhé P, Israël-Biet D (2005) Developmental expression of vasoactive and growth factors in human lung. Role in pulmonary vascular resistance adaptation at birth. Pediatr Res 57(5 Pt 2):21R–25R. https://doi.org/10.1203/01.PDR.0000159575.58834.8D
Muneuchi J, Ochiai Y, Masaki N, Okada S, Iida C, Sugitani Y, Ando Y, Watanabe M (2019) Pulmonary arterial compliance is a useful predictor of pulmonary vascular disease in congenital heart disease. Heart Vessels 34(3):470–476. https://doi.org/10.1007/s00380-018-1263-9
Funding
This work received no specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
The authors’ contributions are as the follows; YI: writing original draft, investigation, J M: conceptualization, methodology, editing, MW: conceptualization, data curation, YS; data curation, YO; critical review.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to declare.
Ethical Standards
This work does not involve any human/animal experimentation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iwaya, Y., Muneuchi, J., Watanabe, M. et al. Decreased Pulmonary Arterial Compliance is a Predictor for Poor Outcomes in Infants with Isolated Atrial Septal Defect and Pulmonary Hypertension. Pediatr Cardiol 41, 1408–1413 (2020). https://doi.org/10.1007/s00246-020-02400-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02400-4