Abstract
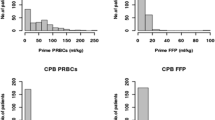
A restrictive blood transfusion strategy has emerged in adult cardiac surgery. However, the feasibility in children is poorly investigated. 352 consecutive patients undergoing open-heart surgery were retrospectively reviewed, excluding patients requiring extracorporeal membrane oxygenation. Patient demographics, perioperative blood product usage, and clinical outcome parameters were investigated. Variables predicting the need for blood products were delineated. Of the 352 study patients, 148 patients (42%) underwent bloodless surgery and 204 (58%) were transfused. Of the 204 transfused patients, 170 (83.4%) patients received one blood transfusion and 34 (16.6%) received two or more blood transfusions. Patient’s weight and preoperative hematocrit (Hct) were statistically significant in predicting the need for blood priming the CPB circuit (AUC 0.99, p < 0.001, sensitivity 96.6%, specificity 95.2%). A body weight of 8.5 kg carried a sensitivity of 100% and specificity of 94.5% (p < 0.001) for a blood prime. Among patients with a weight less than 8.5 kg (n = 171), only 27 patients (15.8%, p < 0.001) required additional transfusion of PRBCs. Factors impacting the need for a blood transfusion during CPB included redo surgery [odds ratio (OR) 4.61, p = 0.001] and the highest lactate level on CPB (OR 1.65, p = 0.006). Redo surgery had the highest impact (OR 7.27, p = 0.012) for requiring a postoperative PRBC transfusion. A restrictive transfusion strategy can be safely implemented in pediatric cardiac surgery. The majority of children with a BW > 8.5 kg required no blood products and those with a BW ≤ 8.5 kg required only 1 unit of blood, to prime the cardiopulmonary bypass circuit.


Similar content being viewed by others
Abbreviations
- ACC:
-
Aortic cross-clamp
- BW:
-
Body weight
- CPB:
-
Cardiopulmonary bypass
- ECMO:
-
Extracorporeal membrane oxygenation
- Hb:
-
Hemoglobin
- Hct:
-
Hematocrit
- MUF:
-
Modified ultrafiltration
- NIRS:
-
Near infrared spectroscopy
- PD Hct:
-
Post-dilution hematocrit
- POD:
-
Postoperative day
- PRBC:
-
Packed red blood cells
- RACHS-1:
-
Risk Adjustment in Congenital Heart Surgery
- SCUF:
-
Slow continuous ultrafiltration
- SpO2 :
-
Systemic oxygen saturation
References
Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD (2007) Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation 116(22):2544–2552
Kipps AK, Wypij D, Thiagarajan RR, Bacha EA, Newburger JW (2011) Blood transfusion is associated with prolonged duration of mechanical ventilation in infants undergoing reparative cardiac surgery. Pediatr Crit Care Med 12(1):52–56
Banbury MK, Brizzio ME, Rajeswaran J, Lytle BW, Blackstone EH (2006) Transfusion increases the risk of postoperative infection after cardiovascular surgery. J Am Coll Surg 202(1):131–138
Kneyber MC, Grotenhuis F, Berger RF, Ebels TW, Burgerhof JG, Albers MJ (2013) Transfusion of leukocyte-depleted RBCs is independently associated with increased morbidity after pediatric cardiac surgery. Pediatr Crit Care Med 14(3):298–305
Gauvin F, Robillard P, Hume H et al (2012) Transfusion-related acute lung injury in the Canadian paediatric population. Paediatr Child Health 17(5):235–239
Salpeter SR, Buckley JS, Chatterjee S (2014) Impact of more restrictive blood transfusion strategies on clinical outcomes: a meta-analysis and systematic review. Am J Med 127(2):124–131
Carson JL, Terrin ML, Noveck H et al (2011) Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 365(26):2453–2462
Lacroix J, Hebert PC, Hutchison JS et al (2007) Transfusion strategies for patients in pediatric intensive care units. N Engl J Med 356(16):1609–1619
Marik PE, Corwin HL (2008) Efficacy of red blood cell transfusion in the critically ill: a systematic review of the literature. Crit Care Med 36(9):2667–2674
Hebert PC, Wells G, Blajchman MA et al (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion requirements in critical care investigators, Canadian critical care trials group. N Engl J Med 340(6):409–417
Song HK, von Heymann C, Jespersen CM et al (2014) Safe application of a restrictive transfusion protocol in moderate-risk patients undergoing cardiac operations. Ann Thorac Surg 97(5):1630–1635
Shehata N, Burns LA, Nathan H et al (2012) A randomized controlled pilot study of adherence to transfusion strategies in cardiac surgery. Transfusion 52(1):91–99
Hajjar LA, Vincent JL, Galas FR et al (2010) Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA 304(14):1559–1567
Carson JL, Duff A, Poses RM et al (1996) Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 348(9034):1055–1060
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI (2002) Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 123(1):110–118
Hebert PC, Wells G, Tweeddale M et al (1997) Does transfusion practice affect mortality in critically ill patients? Transfusion Requirements in Critical Care (TRICC) investigators and the Canadian critical care trials group. Am J Respir Crit Care Med 155(5):1618–1623
Iyengar A, Scipione CN, Sheth P et al (2013) Association of complications with blood transfusions in pediatric cardiac surgery patients. Ann Thorac Surg 96(3):910–916
Redlin M, Kukucka M, Boettcher W et al (2013) Blood transfusion determines postoperative morbidity in pediatric cardiac surgery applying a comprehensive blood-sparing approach. J Thorac Cardiovasc Surg 146(3):537–542
Szekely A, Cserep Z, Sapi E et al (2009) Risks and predictors of blood transfusion in pediatric patients undergoing open heart operations. Ann Thorac Surg 87(1):187–197
de Gast-Bakker DH, de Wilde RB, Hazekamp MG et al (2013) Safety and effects of two red blood cell transfusion strategies in pediatric cardiac surgery patients: a randomized controlled trial. Intensive Care Med 39(11):2011–2019
Cholette JM, Rubenstein JS, Alfieris GM, Powers KS, Eaton M, Lerner NB (2011) Children with single-ventricle physiology do not benefit from higher hemoglobin levels post cavopulmonary connection: results of a prospective, randomized, controlled trial of a restrictive versus liberal red-cell transfusion strategy. Pediatr Crit Care Med 12(1):39–45
Pagano D, Milojevic M, Meesters MI et al (2018) 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery. Eur J Cardiothorac Surg 53(1):79–111
Karkouti K, O’farrell R, Yau TM, Beattie WS (2006) Prediction of massive blood transfusion in cardiac surgery. Can J Anaesth 53(8):781–794
Carter RC, Jacobson JL, Burden MJ et al (2010) Iron deficiency anemia and cognitive function in infancy. Pediatrics 126(2):e427–e434
Hurtado EK, Claussen AH, Scott KG (1999) Early childhood anemia and mild or moderate mental retardation. Am J Clin Nutr 69(1):115–119
Jonas RA, Wypij D, Roth SJ et al (2003) The influence of hemodilution on outcome after hypothermic cardiopulmonary bypass: results of a randomized trial in infants. J Thorac Cardiovasc Surg 126(6):1765–1774
Newburger JW, Jonas RA, Soul J et al (2008) Randomized trial of hematocrit 25% versus 35% during hypothermic cardiopulmonary bypass in infant heart surgery. J Thorac Cardiovasc Surg 135(2):347–354
Funding
No Funding was providing for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kato, H., Chasovskyi, K. & Gandhi, S.K. Are Blood Products Routinely Required in Pediatric Heart Surgery?. Pediatr Cardiol 41, 932–938 (2020). https://doi.org/10.1007/s00246-020-02338-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02338-7