Abstract
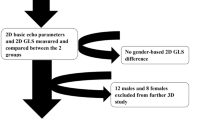
Accurate assessment of LV systolic function remains a challenge, especially in the pediatric population. Myocardial strain measurement by 2D speckle tracking echocardiography (2DSTE) is a relatively new modality for assessment of regional and global myocardial wall motion. This study aims to establish the normative value among various pediatric age groups at a large pediatric tertiary care institution and to describe the challenges encountered in establishing such strain data. Transthoracic echocardiograms were acquired in 121 healthy children (age 0–21 years) and were retrospectively analyzed. The global longitudinal strain (GLS) was obtained by 2D speckle tracking using Philips Epiq7® and QLAB post processing software. The normative value for left ventricular GLS (%) obtained in our study was − 20.8 ± 2.3 (< 1 year); − 21.4 ± 2.2 (1–4 years); − 19.6 ± 2.4 (5–9 years); − 19.4 ± 2.6 (10–14 years); − 18.9 ± 3.0 (15–21 years). There was a statistically significant difference in GLS between the different age groups. The BMI (kg/m2) of assessed subjects were 14.6 ± 2.3 (< 1 year); 16.3 ± 1.5 (1–4 years); 16.7 ± 2.3 (5–9 years); 21.3 ± 4.6 (10–14 years); 23.9 ± 5.9 (15–21 years). There was no significant difference in GLS by gender or by BMI found in our study. We present our experience with establishment of normative values of 2DSTE in our pediatric echocardiography lab. This study shows that age is the major determinant of variation in peak GLS in healthy subjects, emphasizing the importance of establishment of normative data among various age groups in pediatrics.

Reproduced with permission from Ref. [1]





Similar content being viewed by others
References
Sengupta PP et al (2007) Left ventricular form and function revisited: applied translational science to cardiovascular ultrasound imaging. J Am Soc Echocardiogr 20(5):539–551
Lang RM et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
Marcus KA et al (2011) Reference values for myocardial two-dimensional strain echocardiography in a healthy pediatric and young adult cohort. J Am Soc Echocardiogr 24(6):625–636
Korinek J et al (2005) Two-dimensional strain–a Doppler-independent ultrasound method for quantitation of regional deformation: validation in vitro and in vivo. J Am Soc Echocardiogr 18(12):1247–1253
Hu HM et al (2018) Detection of subclinical anthracyclines' cardiotoxicity in children with solid tumor. Chin Med J (Engl) 131(12):1450–1456
Jashari H et al (2015) Normal ranges of left ventricular strain in children: a meta-analysis. Cardiovasc Ultrasound 13:37
Levy PT et al (2016) Reference ranges of left ventricular strain measures by two-dimensional speckle-tracking echocardiography in children: a systematic review and meta-analysis. J Am Soc Echocardiogr 29(3):209.e6–225.e6
Lai WW et al (2006) Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr 19(12):1413–1430
Bussadori C et al (2009) A new 2D-based method for myocardial velocity strain and strain rate quantification in a normal adult and paediatric population: assessment of reference values. Cardiovasc Ultrasound 7:8
Klitsie LM et al (2013) Longitudinal follow-up of ventricular performance in healthy neonates. Early Hum Dev 89(12):993–997
Takayasu H et al (2011) Left ventricular torsion and strain in patients with repaired tetralogy of Fallot assessed by speckle tracking imaging. Echocardiography 28(7):720–729
Kibar AE et al (2015) Effect of obesity on left ventricular longitudinal myocardial strain by speckle tracking echocardiography in children and adolescents. Balkan Med J 32(1):56–63
Takigiku K et al (2012) Normal range of left ventricular 2-dimensional strain: Japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J 76(11):2623–2632
Poterucha JT et al (2012) Changes in left ventricular longitudinal strain with anthracycline chemotherapy in adolescents precede subsequent decreased left ventricular ejection fraction. J Am Soc Echocardiogr 25(7):733–740
Manalo R et al (2019) Does myocardial strain remain abnormal long after normalization of ejection fraction in patients with acute myocarditis? Echocardiography 36(3):609–612
Zhang X et al (2015) Speckle tracking echocardiography: clinical applications in cardiac resynchronization therapy. Int J Clin Exp Med 8(5):6668–6676
Li J-Y et al (2019) Assessment of right ventricular strain in children with repaired tetralogy of Fallot using speckle tracking imaging. Chin Med J 132(6):744–748. https://doi.org/10.1097/CM9.0000000000000126
Ng ACT et al (2018) Left ventricular global longitudinal strain is predictive of all-cause mortality independent of aortic stenosis severity and ejection fraction. Eur Heart J Cardiovasc Imaging 19(8):859–867. https://doi.org/10.1093/ehjci/jex189
Tower-Rader et al (2018) Prognostic value of global longitudinal strain in hypertrophic cardiomyopathy: a systematic review of existing literature. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2018.07.016
Funding
No funding was secured for this case report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Garg, A., Manalo, R., Gorla, S.R. et al. Establishment of Myocardial Strain Measurement Data in Pediatric Patients Without Structural Heart Disease: A Single Center Study. Pediatr Cardiol 41, 892–898 (2020). https://doi.org/10.1007/s00246-020-02328-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02328-9