Abstract
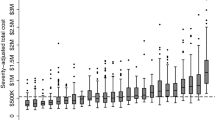
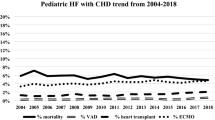
Rehospitalization following pediatric heart transplantation is common. However, existing data remain somewhat limited. Using a novel linkage between administrative and clinical databases, pediatric heart transplant (HT) recipients from 29 centers who survived to discharge were retrospectively reviewed to determine the frequency, timing of, and indication for all-cause rehospitalizations in the year following transplant discharge. Of 2870 pediatric HT recipients, 1835 (63.9%) were rehospitalized in the first year post-discharge (5429 total readmissions). Rehospitalization rates varied significantly across centers (46% to 100%) and were inversely correlated to center transplant volume (r2 0.25, p < 0.01). The median number of rehospitalizations per patient was 2 (IQR 1–4) and the median time to first rehospitalization was 29 days (IQR 9–99 days). Independent risk factors for rehospitalization included younger age at HT (HR 0.99, 95% CI 0.97–0.99), congenital heart disease (HR 1.2, 95% CI 1.1–1.4), listing status 1B at transplant (HR 1.3, 95% CI 1.1–1.5), and post-transplant complications including rejection prior to discharge (HR 1.5 95% CI 1.3–1.8) and chylothorax (HR 1.3, 95% CI 1.0–1.6). Cardiac diagnoses were the most common indication for rehospitalization (n = 1600, 29.5%), followed by infection (n = 1367, 25.2%). These findings may serve to guide the development of interventions aimed at reducing post-HT hospitalizations.




Similar content being viewed by others
References:
Rossano JW, Cherikh WS, Chambers DC, Goldfarb S, Hayes D Jr, Khush KK, Kucheryavaya AY, Toll AE, Levvey BJ, Meiser B, Stehlik J (2018) The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: twenty-first pediatric heart transplantation report-2018; Focus theme: Multiorgan Transplantation. J Heart Lung Transpl 37:1184–1195
McAdams-Demarco MA, Grams ME, Hall EC, Coresh J, Segev DL (2012) Early hospital readmission after kidney transplantation: patient and center-level associations. Am J Transpl 12:3283–3288
Pereira AA, Bhattacharya R, Carithers R, Reyes J, Perkins J (2012) Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transpl 18:1037–1045
Donovan MP, Drusin RE, Edwards NM, Lietz K (2002) Analysis of trends in hospital readmissions and postoperative complications in heart transplant recipients: single center study. Transpl Proc 34:1853–1854
Boubaker K, Harzallah A, Ounissi M, Becha M, Guergueh T, Hedri H, Kaaroud H, Abderrahim E, Ben Abdellah T, Kheder A (2011) Rehospitalization after kidney transplantation during the first year: length, causes and relationship with long-term patient and graft survival. Transpl Proc 43:1742–1746
Jalowiec A, Grady KL, White-Williams C (2008) Predictors of rehospitalization time during the first year after heart transplant. Heart Lung 37:344–355
Dharnidharka VR, Stablein DM, Harmon WE (2004) Post-transplant infections now exceed acute rejection as cause for hospitalization: a report of the NAPRTCS1. Am J Transpl 4:384–389
Tsao CI, Chou NK, Chi NH, Yu HY, Chen YS, Wang CH, Ko WJ, Chen SC, Wang SS (2010) Unplanned readmission within 1 year after heart transplantation in Taiwan. Transpl Proc 42:946–947
Hollander SA, McElhinney DB, Almond CS, McDonald N, Chen S, Kaufman BD, Bernstein D, Rosenthal DN (2017) Rehospitalization after pediatric heart transplantation: incidence, indications, and outcomes. Pediatr Transpl 21:e12857
Mahle WT, Mason KL, Dipchand AI, Richmond M, Feingold B, Canter CE, Hsu DT, Singh TP, Shaddy RE, Armstrong BD, Zeevi A, Ikle DN, Diop H, Odim J, Webber SA (2019) Hospital readmission following pediatric heart transplantation. Pediatr Transpl. https://doi.org/10.1111/petr.13561:e13561
Godown J, Thurm C, Dodd DA, Soslow JH, Feingold B, Smith AH, Mettler BA, Thompson B, Hall M (2017) A unique linkage of administrative and clinical registry databases to expand analytic possibilities in pediatric heart transplantation research. Am Heart J 194:9–15
Healthcare Cost and Utilization Project (H-CUP) Clinical classification software. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed 26 June 2019
Dharnidharka VR, Stablein DM, Harmon WE (2004) Post-transplant infections now exceed acute rejection as cause for hospitalization: a report of the NAPRTCS. Am J Transpl 4:384–389
Menachem JN, Lindenfeld J, Schlendorf K, Shah AS, Bichell DP, Book W, Brinkley DM, Danter M, Frischhertz B, Keebler M, Kogon B, Mettler B, Rossano J, Sacks SB, Young T, Wigger M, Zalawadiya S (2018) Center volume and post-transplant survival among adults with congenital heart disease. J Heart Lung Transpl 37:1351–1360
Rana A, Fraser CD, Scully BB, Heinle JS, McKenzie ED, Dreyer WJ, Kueht M, Liu H, Brewer ED, Rosengart TK, O'Mahony CA, Goss JA (2017) Inferior outcomes on the waiting list in low-volume pediatric heart transplant centers. Am J Transpl 17:1515–1524
Kogon BE, Oster ME, Wallace A, Chiswell K, Hill KD, Cox ML, Jacobs JP, Pasquali S, Karamlou T, Jacobs ML (2019) Readmission after pediatric cardiothoracic surgery: an analysis of the Society of Thoracic Surgeons Database. Ann Thorac Surg 107:1816–1823
Magnetta DA, Godown J, West S, Zinn M, Rose-Felker K, Miller S, Feingold B (2019) Impact of the 2016 revision of US pediatric heart allocation policy on waitlist characteristics and outcomes. Am J Transpl. https://doi.org/10.1111/ajt.15567
Funding
This project was supported through internal funding from the Katherine Dodd Faculty Scholar Program at Vanderbilt University (JG). Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health T32HL105334 (NL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No authors have conflict of interest to declare in relation to the material presented.
Disclosures
The data reported here have been supplied by the Hennepin Healthcare Research Institute as the contractor for the SRTR. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
246_2020_2326_MOESM3_ESM.eps
Supplementary file3 (EPS 114 kb). Supplemental Fig. 1 Correlation between center rehospitalization rate and median length of stay for the transplant admission across 29 pediatric transplant centers
Rights and permissions
About this article
Cite this article
Lambert, A.N., Weiner, J.G., Hall, M. et al. Rehospitalization Following Pediatric Heart Transplantation: Incidence, Indications, and Risk Factors. Pediatr Cardiol 41, 584–590 (2020). https://doi.org/10.1007/s00246-020-02326-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02326-x