Abstract
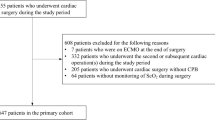
Optimizing oxygen delivery to the brain is one of the main goals in children with congenital heart defects after surgery. It has been shown that cerebral oxygen saturation (cSO2) is depressed within the first day after neonatal cardiopulmonary bypass surgery. However, peri-operative cerebral oxygen metabolism has not yet been assessed in previous studies. The aim of this study was to describe the peri-operative changes in cerebral oxygen metabolism in neonates with congenital heart defects following cardiopulmonary bypass surgery. Prospective observational cohort study. PICU of a tertiary referral center. Fourteen neonates with hypoplastic left heart syndrome (HLHS) undergoing Norwood procedure and 14 neonates with transposition of great arteries (TGA) undergoing arterial switch operation (ASO) were enrolled. Pediatric heart surgery. We measured non-invasively regional cSO2 and microperfusion (rcFlow) using tissue spectrometry and laser Doppler flowmetry before and after surgery. Cerebral fractional tissue oxygen extraction (cFTOE), the arterio–cerebral difference in oxygen content (acDO2) and approximated cerebral metabolic rate of oxygen (aCMRO2) were calculated. According to the postsurgical hemodynamics, arterial saturation (aSO2) normalized immediately after surgery in the TGA group, whereas HLHS patients still were cyanotic. cSO2 significantly increased in TGA group over 48 h after ASO (p = 0.004) and was significantly higher compared to HLHS group after Norwood procedure. cFTOE as a risk marker for brain injury was elevated before surgery (TGA group 0.37 ± 0.10, HLHS group 0.42 ± 0.12) and showed a slight decrease after ASO (p = 0.35) but significantly decreased in patients after Norwood procedure (p = 0.02). Preo-peratively, acDO2 was significantly higher in patients with HLHS compared to patients with TGA (7.7 ± 2.5 vs. 5.2 ± 1.6 ml/dl, p = 0.005), but normalized in the posto-perative course. Before surgery, the aCMRO2 was slightly higher in the HLHS group (5.1 ± 1.5 vs. 3.9 ± 2.5 AU, p = 0.14), but significantly decreased after Norwood procedure (− 1.6 AU, p = 0.009). There was no difference in rcFlow between both groups and between the points in time prior and after surgery. Neonates undergoing cardiac surgery suffer from peri-operative changes in hemodynamics and cerebral hypoxemic stress. The cerebral oxygen metabolism seems to be more affected in cyanotic children with functionally univentricular hearts compared to post-operative acyanotic patients. Additional stress factors must be avoided to achieve the best possible neurological outcome.


Similar content being viewed by others
References
Hoffman GM, Stuth EA, Jaquiss RD et al (2004) Changes in cerebral and somatic oxygenation during stage 1 palliation of hypoplastic left heart syndrome using continuous regional cerebral perfusion. J Thorac Cardiovasc Surg 127(1):223–233
Uebing A, Furck AK, Hansen JH et al (2011) Perioperative cerebral and somatic oxygenation in neonates with hypoplastic left heart syndrome or transposition of the great arteries. J Thorac Cardiovasc Surg 142(3):523–530
Toet MC, Flinterman A, Laar I et al (2005) Cerebral oxygen saturation and electrical brain activity before, during, and up to 36 hours after arterial switch procedure in neonates without pre-existing brain damage: its relationship to neurodevelopmental outcome. Exp Brain Res 165(3):343–350
Phelps HM, Mahle WT, Kim D et al (2009) Postoperative cerebral oxygenation in hypoplastic left heart syndrome after the Norwood procedure. Ann Thorac Surg 87(5):1490–1494
Klein KU, Fukui K, Schramm P et al (2011) Human cerebral microcirculation and oxygen saturation during propofol-induced reduction of bispectral index. Br J Anaesth 107(5):735–741
Klein KU, Schramm P, Glaser M et al (2010) Intraoperative monitoring of cerebral microcirculation and oxygenation-a feasibility study using a novel photo-spectrometric laser-Doppler flowmetry. J Neurosurg Anesthesiol 22(1):38–45
Neunhoeffer F, Sandner K, Wiest M et al (2017) Non-invasive assessment of cerebral oxygen metabolism following surgery of congenital heart disease. Interact Cardiovasc Thorac Surg 25(1):96–102
Neunhoeffer F, Warmann SW, Hofbeck M et al (2017) Elevated intrathoracic CO2 pressure during thoracoscopic surgery decreases regional cerebral oxygen saturation in neonates and infants-a pilot study. Paediatr Anaesth 27(7):752–759
Neunhoeffer F, Wiest M, Sandner K et al (2016) Non-invasive measurement of renal perfusion and oxygen metabolism to predict postoperative acute kidney injury in neonates and infants after cardiopulmonary bypass surgery. Br J Anaesth 117(5):623–634
Balegar KK, Stark MJ, Briggs N et al (2014) Early cerebral oxygen extraction and the risk of death or sonographic brain injury in very preterm infants. J Pediatr 164(3):475–480
Kissack CM, Garr R, Wardle SP et al (2004) Cerebral fractional oxygen extraction in very low birth weight infants is high when there is low left ventricular output and hypocarbia but is unaffected by hypotension. Pediatr Res 55(3):400–405
Lemmers PM, Toet M, van Schelven LJ et al (2006) Cerebral oxygenation and cerebral oxygen extraction in the preterm infant: the impact of respiratory distress syndrome. Exp Brain Res 173(3):458–467
Jain V, Buckley EM, Licht DJ et al (2014) Cerebral oxygen metabolism in neonates with congenital heart disease quantified by MRI and optics. J Cereb Blood Flow Metab 34(3):380–388
Vestergaard MB, Lindberg U, Aachmann-Andersen NJ et al (2016) Acute hypoxia increases the cerebral metabolic rate—a magnetic resonance imaging study. J Cereb Blood Flow Metab 36(6):1046–1058
Xu F, Liu P, Pascual JM et al (2012) Effect of hypoxia and hyperoxia on cerebral blood flow, blood oxygenation, and oxidative metabolism. J Cereb Blood Flow Metab 32(10):1909–1918
Gaies MG, Gurney JG, Yen AH et al (2010) Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11(2):234–238
Rajan V, Varghese B, van Leeuwen TG et al (2009) Review of methodological developments in laser Doppler flowmetry. Lasers Med Sci 24(2):269–283
ter Horst HJ, Verhagen EA, Keating P et al (2011) The relationship between electrocerebral activity and cerebral fractional tissue oxygen extraction in preterm infants. Pediatr Res 70(4):384–388
Votava-Smith JK, Statile CJ, Taylor MD et al (2017) Impaired cerebral autoregulation in preoperative newborn infants with congenital heart disease. J Thorac Cardiovasc Surg 154(3):1038–1044
Licht DJ, Wang J, Silvestre DW et al (2004) Preoperative cerebral blood flow is diminished in neonates with severe congenital heart defects. J Thorac Cardiovasc Surg 128(6):841–849
Dehaes M, Cheng HH, Buckley EM et al (2015) Perioperative cerebral hemodynamics and oxygen metabolism in neonates with single-ventricle physiology. Biomed Opt Express 6(12):4749–4767
Funding
This study was funded by the foundation Stiftung KinderHerz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All author declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants/parents included in the study.
Rights and permissions
About this article
Cite this article
Neunhoeffer, F., Hofbeck, M., Schlensak, C. et al. Perioperative Cerebral Oxygenation Metabolism in Neonates with Hypoplastic Left Heart Syndrome or Transposition of the Great Arteries. Pediatr Cardiol 39, 1681–1687 (2018). https://doi.org/10.1007/s00246-018-1952-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1952-2