Abstract
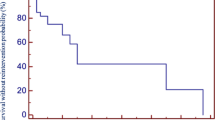
The Fontan operation and its modifications are currently the standard palliation in patients with single ventricle physiology. The advantages of extracardiac conduit Fontan operation (ECF) have previously been described. We evaluated the outcome of patients who underwent ECF operation at our center since the year 2000 to assess morbidity, mortality and New York Heart Association (NYHA) functional class in the current era. Medical records of 97 patients who underwent ECF operation from November 2000 till October 2013 were reviewed to determine the diagnosis, age at surgery, surgical technique, postoperative complications, NYHA class at last follow-up, echocardiographic parameters, and most recent Holter monitor results. The median age at surgery was 3.4 years with 4 total deaths until last follow-up (hospital mortality was 1 %, and mortality after hospital discharge was 3 %). Seventy-eight of the 97 patients (80 %) underwent fenestrated Fontan surgery. Median duration of follow-up was 3.9 years (IQR 0.2–12.2 years). At the latest follow-up, 62 patients (67 %) were determined to be in NYHA class I, 25 patients (27 %) in NYHA class II, and 6 (6 %) patients in NYHA class III, and the median oxygen saturation was 92 % (IQR 86–96). There were 15 patients with history of preoperative arrhythmias and 6 of them required pacemaker placement at the time of surgery. One patient developed ectopic atrial tachycardia, and 1 patient had clinical thromboembolism on follow-up. Systolic function of the single ventricle by transthoracic echocardiogram at the latest follow-up was described as normal in 77 patients (83 %), fair in 15 patients (16 %), and poor in 1 patient (1 %). The results of our study show that patients who undergo extracardiac conduit Fontan operation in the modern era may have significantly less morbidity and mortality when compared to earlier years.



Similar content being viewed by others
References
Fontan F, Baudet E (1971) Surgical repair of tricuspid atresia. Thorax 26:240–248
Puga FJ, Chiavarelli M, Hagler DJ (1987) Modifications of the Fontan operation applicable to patients with left atrioventricular valve atresia or single atrioventricular valve. Circulation 76:III53–III60
de Leval MR, Kilner P, Gewillig M, Bull C (1988) Total cavopulmonary connection: a logical alternative to atriopulmonary connection for complex Fontan operations. Experimental studies and early clinical experience. J Thoracic Cardiovasc Surg 96:682–695
Pizarro C, de Leval MR (1998) Surgical variations and flow dynamics in cavopulmonary connections: a historical review. Pediatr Card Surg Annu Semin Thorac Cardiovasc Surg 1:53–59
Azakie A, McCrindle BW, Van Arsdell G, Benson LN, Coles J, Hamilton R, Freedom RM, Williams WG (2001) Extracardiac conduit versus lateral tunnel cavopulmonary connections at a single institution: impact on outcomes. J Thorac Cardiovasc Surg 122:1219–1228
Lee JR, Kwak JG, Kim KC, Min SK, Kim WH, Kim YJ, Rho JR (2007) Comparison of lateral tunnel and extracardiac conduit Fontan procedure. Interact CardioVasc Thorac Surg 6:328–330
Brown JW, Ruzmetov M, Deschner BW, Rodefeld MD, Turrentine MW (2010) Lateral tunnel Fontan in the current era: is it still a good option? Ann Thorac Surg 89:556–563
Kim SJ, Kim WH, Lim HG, Lee JY (2008) Outcome of 200 patients after an extracardiac Fontan procedure. J Thorac Cardiovasc Surg 136:108–116
Hirsch JC, Goldberg C, Bove EL, Salehian S, Lee T, Ohye RG, Devaney EJ (2008) Fontan operation in the current era: a 15-year single institution experience. Ann Surg 248:402–410
Lamberti JJ, Spicer RL, Waldman JD, Grehl TM, Thomson D, George L, Kirkpatrick SE, Mathewson JW (1990) The bidirectional cavopulmonary shunt. J Thorac Cardiovasc Surg 100:22–29
Bridges ND, Jonas RA, Mayer JE, Flanagan MF, Keane JF, Castaneda AR (1990) Bidirectional cavopulmonary anastomosis as interim palliation for high-risk Fontan candidates: early results. Circulation 82(5):IV170–176
Bove EL (1998) Current status of staged reconstruction for hypoplastic left heart syndrome. Pediatr Cardiol 19:308–315
Bove EL, Ohye RG, Devaney EJ (2004) Hypoplastic left heart syndrome: conventional surgical management. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 7:3–10
Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C (2002) Fenestration improves clinical outcome of the Fontan procedure: a prospective, randomized study. Circulation 105:207–212
Gentles TL, Mayer JE Jr, Gauvreau K, Newburger JW, Lock JE, Kupferschmid JP et al (1997) Fontan operation in five hundred consecutive patients: factors influencing early and late outcome. J Thorac Cardiovasc Surg 114(3):376–391
Chowdhury UK, Airan B, Kothari SS, Talwar S, Saxena A, Singh R et al (2005) Specific issues after extracardiac Fontan operation: ventricular function, growth potential, arrhythmia, and thromboembolism. Ann Thorac Surg 80:665–672
Mitchell ME, Ittenback RF, Gaynor W, Wernovsky G, Nicolson S, Spray TL (2006) Intermediate outcomes after the Fontan procedure in the current era. J Thorac Cardiovasc Surg 131:172–180
Tweddell JS, Nersesian M, Mussatto KA, Nugent M, Simpson P, Mitchell ME et al (2009) Fontan palliation in the modern era: factors impacting mortality and morbidity. Ann Thorac Surg 88:1291–1299
Giannico S, Hammad F, Amodeo A, Michielon G, Drago F, Turchetta A et al (2006) Clinical outcome of 193 extracardiac Fontan patients: the first 15 years. J Am Coll Cardiol 47:2065–2073
Marcelletti CF, Iorio FS, Abella RF (1999) Late results of extracardiac Fontan repair. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2:131–142
Nakano T, Kado H, Ishikawa S, Shiokawa Y, Ushinohama H, Sagawa K et al (2004) Midterm surgical results of total cavopulmonary connection: clinical advantages of the extracardiac conduit method. J Thorac Cardiovasc Surg 127:730–737
Nakano T, Kado H, Tachibana T, Hinokiyama K, Shiose A, Kajimoto M, Ando Y (2007) Excellent midterm outcome of extracardiac conduit total cavopulmonary connection: results of 126 cases. Ann Thorac Surg 84:1619–1626
Rogers LS, Glatz AC, Ravishankar C, Spray TL, Nicolson SC, Rychik J, Rush CH, Gaynor JW, Goldberg DJ (2012) 18 years of the Fontan operation at a single institution: results from 771 consecutive patients. J Am Coll Cardiol 11:1018–1025
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
Rights and permissions
About this article
Cite this article
Raj, S., Rosenkranz, E., Sears, B. et al. Intermediate-Term Results After Extracardiac Conduit Fontan Palliation in Children and Young Adults with Single Ventricle Physiology—A Single-center Experience. Pediatr Cardiol 37, 1111–1118 (2016). https://doi.org/10.1007/s00246-016-1402-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1402-y