Abstract
We evaluated the effects of different respiratory assist modes on cerebral blood flow (CBF) and arterial oxygenation in single-ventricle patients after bidirectional superior cavopulmonary anastomosis (BCPA). We hypothesized that preserved auto-regulation of respiration during neurally adjusted ventilatory assist (NAVA) may have potential advantages for CBF and pulmonary blood flow regulation after the BCPA procedure. We enrolled 23 patients scheduled for BCPA, who underwent pressure-controlled ventilation (PCV), pressure support ventilation (PSV), and NAVA at two assist levels for all modes in a randomized order. PCV targeting large V T (15 mL × kg−1) resulted in lower CBF and oxygenation compared to targeting low V T (10 mL × kg−1). During PSV and NAVA, ventilation assist levels were titrated to reduce EAdi from baseline by 75 % (high assist) and 50 % (low assist). High assist levels during PSV (PSVhigh) were associated with lower PaCO2, PaO2, and O2SAT, lower CBF, and higher pulsatility index compared with those during NAVAhigh. There were no differences in parameters when using low assist levels, except for slightly greater oxygenation in the NAVAlow group. Modifying assist levels during NAVA did not influence hemodynamics, cerebral perfusion, or gas exchange. Targeting the larger V T during PCV resulted in hyperventilation, did not improve oxygenation, and was accompanied by reduced CBF. Similarly, high assist levels during PSV led to mild hyperventilation, resulting in reduced CBF. NAVA’s results were independent of the assist level chosen, causing normalized PaCO2, improved oxygenation, and better CBF than did any other mode, with the exception of PSV at low assist levels.
Similar content being viewed by others
Introduction
In the staged surgical reconstruction of a single functional ventricle resulting in a total cavopulmonary connection (modified Fontan operation), the intermediate stage is a bidirectional superior cavopulmonary anastomosis (BCPA). The intervention is aimed at increasing effective pulmonary blood flow (PBF) [1–3]. This operation routes blood flow from the superior vena cava directly into the pulmonary arteries, whereas blood flow from the inferior vena cava and coronary veins enters the single ventricle directly.
After BCPA, PBF is derived only from the upper body venous return, which, in the infant, largely reflects cerebral blood flow (CBF). Under these circumstances, the cerebral and pulmonary auto-regulatory mechanisms are in direct competition with each other, and the net result on organ perfusion will be different from that in individuals with normal ventricle physiology [2–4]. A unique consequence of BCPA [2, 3] circulation is that systemic arterial oxygenation is the weighted average of deoxygenated blood coming from the inferior vena cava and oxygenated blood from the pulmonary veins. CBF and its auto-regulation may have important clinical implications for the postoperative management and early and late neurodevelopmental outcomes after BCPA [5–8]. Hypercapnia with acidosis increases CBF [9–12] and reduces PBF by increasing pulmonary vascular resistance (PVR) in normal circulation, after cardiopulmonary bypass (CPB), and during anesthesia [13–15]. A unique aspect of PBF physiology after BCPA is the interaction of two highly autonomically regulated vascular beds—cerebral and pulmonary circulation—that have opposite responses to changes in CO2 and acid–base status.
Neurally adjusted ventilatory assist (NAVA) delivers ventilation in proportion to neural inspiratory effort, thus taking advantage of the respiratory control feedback loop [16–18]. Electrical activity of the diaphragm (EAdi) is a measure of the patient’s neural drive, auto-regulated by the patient’s neuroventilatory coupling. During NAVA, the EAdi signal determines both timing and amplitude of the ventilatory assist, resulting in a proportional respiratory assist determined by an operator-set proportionality factor (NAVA level).
Therefore, we hypothesized that preserved auto-regulation of respiration during NAVA may have potential advantages for CBF and PBF regulation after the BCPA procedure and that this would result in an optimal balance between adequate pulmonary perfusion and CBF post-BCPA. Hence, this report concentrates on middle cerebral artery blood flow (MCABF) and gas exchange effects induced by different levels of ventilator assist during pressure-controlled ventilation (PCV), pressure support ventilation (PSV), and NAVA.
Materials and Methods
Patients
The study protocol was approved by the research and ethics review board at Shanghai Children’s Medical Center, China. Informed and signed consent were obtained from the parents of all patients. Twenty-three patients with a median age of 10.0 months (range 4–39 months) and a median weight of 7.5 kg (range 5–11.5 kg) scheduled for BCPA were enrolled preoperatively. The demographic, diagnostic, and surgical characteristics analyzed are described in Table 1.
Surgical Procedures and Postoperative Strategy
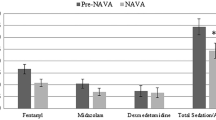
All patients were intubated with a cuffed endotracheal tube (Mallinckrodt Medical, Westmeath, Ireland). General anesthesia was maintained with inhaled sevoflurane, intravenous fentanyl, and pancuronium bromide. CPB with modified ultrafiltration was performed for 56–120 min (median 98 min) without aortic cross-clamping in 22 patients (Table 1) as the routine strategy in our institution, while another patient underwent the BCPA procedure without CPB. All patients were weaned from CPB when the transesophageal temperature reached 35 °C and hemodynamic stability was achieved. On return to the cardiac intensive care unit, patients were mechanically ventilated with a Servo-i ventilator (Maquet Critical Care, Solna, Sweden) capable of delivering PCV, PSV, and NAVA. The FiO2 was 0.40–0.60 in all patients. The aim of mechanical ventilation was to maintain PaCO2 at 40 mmHg and PaO2 ≥40 mmHg. Rectal temperature was maintained at 36–37.5 °C using a cooling or warming blanket. The patients received infusions of propofol (2 mg/kg/h) for the duration of the study. Hemoglobin concentration was maintained at or above 120 g/L. Dopamine (5 mcg/kg/min) and milrinone (0.5 mcg/kg/min) were infused to maintain hemodynamic stability. Superior vena cava pressure was monitored and maintained between 10–20 mmHg by infusion of 5 % albumin (5 mL/kg) before the start of the study. After stabilization, the insertion and correct positioning of the EAdi catheter were assured by means of a specific function in the ventilator (“EAdi catheter positioning”). Inotropes, vasodilators, PEEP, and FiO2 were not adjusted after study initiation.
Measurements
Patient Monitoring
All patients underwent continuous invasive monitoring of systemic arterial and superior vena cava pressure, which was considered central venous pressure (CVP). Heart rate (HR), arterial blood pressure (BP), respiratory rate (RR), airway pressure [such as positive inspiratory pressure (PIP) and mean airway pressure (MAP)], tidal volumes (V T) delivered by the ventilator, and rectal temperature were monitored continuously. Before the beginning of the study, the endotracheal tube cuff was checked and inflated to eliminate gas leaks. EAdi and respiratory variables were monitored from the Servo-i ventilator.
Arterial Blood Gases (ABGs)
Arterial blood samples were obtained from the peripheral arterial catheter and analyzed for PaCO2, PaO2, SaO2, and pH using a blood gas analyzer (ABL 850, Radiometer Copenhagen, Copenhagen, Denmark).
Transcranial Doppler (TCD)
The flow velocity through the middle cerebral artery (MCA) was measured with a 2-MHz pulse-wave ultrasound transducer (EMS-9UA), fixed above the zygomatic arch with a soft rubber holder (Delica Electronics Co., Ltd. Shenzhen, China). The transducer interrogated the portion of the MCA near its junction to the ipsilateral anterior cerebral artery.
Study Protocol
The study protocol was started within 2 h of discontinuation of CPB and as soon as a cardiorespiratory steady state was achieved. The protocol consisted of two periods, which were defined as control ventilation and assist ventilation. FiO2 was fixed at 0.4 for all patients after study initiation. PEEP, routinely set at 3–4 cmH2O, was maintained constant throughout the study period. During the first period of the study, all subjects were ventilated with PCV titrated to achieve a tidal volume (V T) of 10 mL/kg (PCVlow) or 15 mL/kg (PCVhigh) at the same respiratory frequency for 30 min with a close monitor of ventilator pressure and hemodynamic in a random order before awake from anesthesia. If hemodynamic instability of patient or the peak inspiratory pressure was more than 20 cmH2O, he will be withdrawn from the study immediately. When the first period was finished and signs of EAdi recovery were registered, the second study period was initiated. EAdi level after 2 min of continuous positive airway pressure was considered EAdibase. After establishing EAdibase, administration of two levels of PSV and NAVA was initiated, following a predefined computer-generated random sequence, defined as levellow and levelhigh. Respiratory assist was delivered to achieve a reduction in peak EAdi by 50 % of EAdibase (PSVlow) and (NAVAlow). During levelhigh, respiratory assist was administered to achieve a reduction in peak EAdi by 75 % of EAdibase (PSVhigh) and (NAVAhigh). Each patient underwent four 30-min trials during the second period. The last 5 min of each trial was recorded and stored on a dedicated personal computer for data analysis. The systolic peak velocity (V s) and the end diastolic velocity (V d) of MCABF measured by TCD were recorded during the last 2 min of each trial. The mean velocity (V m) of MCABF was calculated as “V m = (V s − V d)/3 + V d.” The pulsatility index (PI) was calculated as “PI = (V s − V d)/V m.” At the end of each test period, an arterial blood sample was collected for blood gas analysis.
Data Analysis
Data are expressed as mean ± standard deviation using SAS 9.2 statistical software (SAS Institute, Cary, NC). PCVlow and PCVhigh from the first period and data from the four registrations in the second period were compared using a repeated-measures ANOVA. The comparison of different levels of assistance within each mode (PSVlow vs. PSVhigh and NAVAlow vs. NAVAhigh) and equivalent levels of assistance (PSVlow vs. NAVAlow and PSVhigh vs. NAVAhigh) was assessed by the least significant difference (LSD) methods post hoc test. A p value of <0.05 was considered significant.
Results
Twenty-three patients were enrolled in this study; two patients did not complete the study and were not included in the data analysis. Both excluded patients, marked in Table 1, did not complete the study protocol due to failure to obtain a consistent EAdi signal. Ultrasound examination revealed bilateral diaphragmatic paralysis in both subjects.
PCV with Low and High Tidal Volume Targets
In the first study period, PCVlow versus PCVhigh, patients were hyperventilated during the PCVhigh but not during the PCVlow period, with pH values of 7.47 ± 0.05 versus 7.42 ± 0.05 (P < 0.001), and PaCO2 values of 33.5 ± 5.5 versus 39.3 ± 7.2 mmHg (P < 0.001), respectively. Resulting ventilator pressure and oxygenation data for both groups are given in Table 2. The PCVhigh group had higher CVP compared to the PCVlow group (16 ± 4 vs. 15 ± 4 mmHg; P = 0.001). MCABF velocity values were lower in the PCVhigh group compared to the PCVlow group (V s, 96.6 ± 28.3 vs. 101.8 ± 24.9 m s−1; P = 0.029; V m, 50.1 ± 16.5 vs. 53.8 ± 16.3 m s−1; P = 0.042; and V d, 26.7 ± 9.7 vs. 32.2 ± 11.3 m s−1; P < 0.001). PI was higher during PCVhigh than during PCVlow (1.5 ± 0.2 vs. 1.3 ± 0.3, P < 0.001) (Table 2).
PSV Versus NAVA
Among the four groups on a ventilatory assist mode, either PSV or NAVA at low or high levels of assist resulted in several differences in ventilation parameters (e.g., airway pressures and V T), blood gases, and cerebral blood flow (see Table 3). Post hoc analysis showed the following main differences between various combinations of ventilator modes and assist levels:
-
1.
PSVhigh versus PSVlow and NAVAhigh versus NAVAlow, respectively
The four episodes of assisted ventilation ventilator parameters are given in Table 3. For the two assist levels during PSV, we observed a lower EAdipeak (4.1 ± 2.3 vs. 7.0 ± 3.9; P < 0.001) during PSVhigh when compared to PSVlow. pH values were higher (7.45 ± 0.06 vs. 7.41 ± 0.03; P = 0.002), PaCO2 was lower (34.5 ± 6.6 vs. 39.9 ± 6.8 mmHg, P < 0.001), and PaO2 was lower (43.7 ± 8.58 vs. 45.7 ± 8.9 mmHg; P = 0.013) during PSVhigh when compared to PSVlow. MCABF velocities were significantly lower (P = 0.03) during PSVhigh compared to PSVlow. Detailed MCABF velocity results are given in Table 3.
During NAVA, there were no differences in RR, V T, PIP, and MAP between NAVAhigh and NAVAlow. There was a lower EAdipeak (4.1 ± 2.1 vs. 6.7 ± 3.6 μV; P < 0.001) but no difference in EAdimin (0.5 ± 0.4 vs. 0.5 ± 0.4 μV, P = 0.780) in NAVAlow compared to NAVAhigh. No difference in arterial blood gas between the two assist levels could be observed. Also, there was no difference in MCABF velocities between the two NAVA assist levels (Table 3).
-
2.
PSVhigh versus NAVAhigh and PSVlow versus NAVAlow, respectively
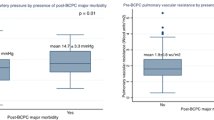
Comparing the breathing patterns and resulting ventilator pressures at similar assist levels during PSV and NAVA, respectively, there were no differences between PSVlow and NAVAlow, whereas there were differences between PSVhigh and NAVAhigh. V T, PIP, and MAP were significantly higher during PSVhigh than during NAVAhigh (Table 3). Comparing the arterial blood gases between the two modes (NAVA and PSV) at the same level of assist, SaO2 (81.9 ± 8.6 vs. 79.6 ± 10.3 %; P < 0.01) was higher and PaCO2 (37.6 ± 6.4 vs. 39.9 ± 6.8 mmHg; P < 0.01) was lower during NAVAlow than during PSVlow. At the higher level of assist, a lower pH (7.42 ± 0.03 vs. 7.45 ± 0.06; P < 0.01), a higher PaCO2 (38.1 ± 6.0 vs. 34.5 ± 6.6 mmHg; P < 0.01), and a higher SaO2 (82.0 ± 7.5 vs. 79.0 ± 9.1 %; P < 0.01) were observed during NAVAhigh compared to PSVhigh. The PI of MCABF was lower in NAVA than in PSV at both assist levels [1.1 ± 0.3 vs. 1.2 ± 0.3 at the lower assist level (P < 0.01) and 1.2 ± 0.3 vs. 1.3 ± 0.4 at the high assist level (P < 0.01)]. V d, but not V s or V m, of MCABF (35.2 ± 13.1 vs. 34.7 ± 12.8 m/s; P < 0.01) was higher during NAVAhigh than during PSVhigh.
Discussion
In patients with a BCPA for single-ventricle physiology, venous return from the brain as well as from the upper extremities is directed into the lungs via the superior vena cava, whereas venous return from the inferior vena cava drains into the right atrium and via the single functional ventricle directly into the arterial circulation. In consequence, systemic arterial oxygenation is the weighted average of the deoxygenated blood coming from the inferior vena cava and the oxygenated blood from the pulmonary veins.
Hypoxemia in the early postoperative period is therefore often considered to be a consequence of transiently elevated PVR that occurs after CPB, which may limit the age at which BCPA can be performed safely. Conventionally, postoperative hypoxemia is refractory to conventional treatment aimed at decreasing PVR, especially in young infants. Hyperventilation and inhaled nitric oxide have been shown ineffective and do not improve oxygenation in the absence of an intrapulmonary shunt [15, 19].
The determinants of systemic oxygenation after the BCPA are multifactorial and depend upon PBF, CBF, cardiac output, and intrapulmonary shunting [20–22]. A unique aspect of the physiology of PBF after BCPA is the interaction of two highly autonomically regulated vascular beds—the cerebral and the pulmonary circulation—that have opposite responses to changes in CO2 and acid–base status [23–25]. It has been reported that hyperventilation to achieve lower PVR impairs oxygenation, while hypoventilation improves oxygenation in patients after BCPA [12, 14, 15, 20, 21]. Li et al. [12] reported that moderate hypercapnia with respiratory acidosis improved arterial oxygenation and reduced oxygen consumption and arterial lactate levels, thus improving overall oxygen transport in children after BCPA. Fogel et al. [13] reported that PaCO2 had a major influence on CBF and PBF distribution, whereas changes in PO2 had only a minor impact. They concluded that increased CO2 tension in patients after BCPA results in increased blood flow to the brain and lungs, improved PaO2, increased cerebral O2 transport, and increased cardiac index, which accounted for the increased CBF. Hoskote et al. [14] demonstrated that increasing PaCO2 from 35 to 55 mmHg improved systemic oxygenation, systemic blood flow, CBF, and PBF. It also decreased systemic vascular resistance without increasing PVR after BCPA. The improvement in oxygenation with hypercapnic acidosis suggests that an increase in cerebral and systemic blood flow overrides the vasoconstrictive effect of hypercapnic acidosis on PVR after BCPA [12–14, 20, 21]. In the first period of our study, we confirmed that hyperventilation due to an excessively high V T did not improve the systemic oxygenation in BCPA circulation; instead, it tended to accentuate hypoxemia. PVR, which depends on the balance in the vascular tone of its two components: the alveolar vessels and the extra-alveolar or parenchymal vessels, is directly affected by changes in lung volume. When the lung is inflated above functional residual capacity, PVR is elevated because the alveolar vessels become compressed as a result of alveolar distension. Meanwhile, the blood flow from the SVC returning to the lung is reduced because of the elevated intrathoracic pressure as a result of high ventilation pressure. These help to explain the effect of lower saturation when the patients after BCPA were hyperventilated, although the cardiovascular effects of mechanical ventilation are complex. The decrease in MCA flow velocity is a major issue as it decreased PBF and the delivery of oxygenated blood into the systemic circulation.
However, most of the methods to increase PBF described above, with the exception of hypoventilation, relied on extrinsically administered CO2, which is not practical for clinical use. Hypercapnia with respiratory acidosis will stimulate the respiratory centers, often resulting in deep sedation or paralysis to inhibit spontaneous inspiratory efforts in these strategies. This would work against the aim of early extubation after BCPA. NAVA, a new method to ventilate patients where auto-regulation of the patient’s neuroventilatory efforts determines ventilation, seems much closer to normal physiology and may be ideal for patients after BCPA.
In the second part of our study, we demonstrated that NAVA with a high support level avoided hyperventilation, in contrast to the high level of PSV. All other settings, except PSVhigh, maintained PaCO2 within the normal range. As a result, there was a tendency toward decreased V d and increased PI of the MCABF during PSVhigh, while this phenomenon did not occur during NAVA, even when a high level of assist was applied. These potential advantages are probably linked to the basic concept of NAVA, which delivers respiratory assist throughout inspiration in proportion to the EAdi signal, reflecting the patient’s neural respiratory drive. Hence, ventilator function and cycling are controlled by the patient’s respiratory drive and rhythm. By optimizing the respiratory control feedback loop, NAVA has the potential to enhance patient–ventilator interaction, ensuring synchrony and minimizing the risk of over-assistance. Sinderby [26] reported that in healthy subjects, NAVA can safely and efficiently unload the respiratory muscles during a maximal inspiratory maneuver, without failing to cycle-off ventilatory assist and without causing excessive lung distention, even when a high level of support was administered. Colombo et al. [27] showed that, in contrast to PSV, NAVA resulted in auto-regulation of the respiratory efforts at different assist levels, avoiding over-assistance and patient–ventilator asynchrony. Terzi et al. [28] reported that, compared to PSV, NAVA in patients with acute respiratory distress syndrome holds promise for limiting the risk of over-assistance, preventing patient–ventilator asynchrony and improving overall patient–ventilator interaction.
In the second period of our study, we confirmed our hypothesis that ventilating patients after BCPA with an auto-regulated ventilation mode, NAVA, avoids over-assistance and hyperventilation and achieves better oxygenation by CBF auto-regulation. We also found that the correlation between PaCO2 and MCABF was not exactly linear, especially when comparing PSVlow and NAVAlow. This finding indicates that lung perfusion is not the only reason for improved oxygenation in patients after BCPA. The variable breathing pattern and assistance of sighs seen during NAVA, which are proportional to the patients’ supported effort, may improve ventilation/perfusion matching and are probably another important effect. EAdimin in NAVA was significantly lower than that in PSV, indicating that end expiratory lung volume was more easily maintained during NAVA.
Our results suggest that NAVA could be the preferred ventilation strategy for patients after the BCPA procedure for single-ventricle physiology. In the past decades, there are some studies that mentioned the cardiovascular effects with different ventilatory techniques [29]. Walsh et al. [30] reported that ventilation with airway pressure release ventilation, when the spontaneous inspiratory effort transmitted to the pleural space results in a consequence of decreased intrapleural pressure, improves lung perfusion compared with pressure control ventilation in children after tetralogy of Fallot repair and cavopulmonary shunt operations. In some cases with high risk of pulmonary venous obstruction before BCPA procedure, such as the patients with single-ventricle physiology combined with total anomalous pulmonary venous connection or obvious systemic atrioventricular valve insufficiency, positive pressure ventilation should be helpful for them to keep functional residual capacity. Moreover, the patients after BCPA procedure with systemic ventricular dysfunction or acute lung injury may not be extubated rapidly postoperatively.
Limitations of the Study
We did not distinguish between the effects of hypercarbia and intrathoracic pressure on CBF and PBF. These two factors are difficult to separate and represent the combined influence of the factors of oxygenation in BCPA circulation. Time considerations did not allow this project to separate the differences related to hypercarbia and intrathoracic pressure, and our results are not objective. We only compared NAVA and PSV in our study, without involving other ventilation strategies. And 30 min of ventilation might be limited in patients with other interfering factors to reach steady state. Further research needs to be done in the future. Some authors reported that CBF was influenced by a high concentration of sedatives [31, 32]. However, the dose of propofol maintained in our study was small and identical in all patients. Thus, the influence of sedatives on MCABF velocity in our study was probably limited.
Conclusion
In the early postoperative period of BCPA in patients with single-ventricle physiology, large V Ts, leading to a slightly increased pH and lower PaCO2, will result in lower CBF and higher resistance of the cerebral vascular bed during controlled mechanical ventilation. Allowing for spontaneous ventilation should therefore be beneficial in BCPA circulation. However, over-assistance can also occur during PSV, whereas during NAVA, with its closed loop concept on the ventilatory drive, this does not occur independently of the assist level. Therefore, NAVA does allow for better oxygenation in BCPA circulation and, through lower cerebral vascular resistance, improved CBF. This suggests that NAVA may play an important role in the postoperative care of patients with single-ventricle physiology.
References
Glenn WW (1984) Superior vena cava-pulmonary artery anastomosis. Ann Thorac Surg 37:9–11
Seliem MA, Baffa JM, Vetter JM, Chen SL, Chin AJ, Norwood WI Jr (1993) Changes in right ventricular geometry and heart rate early after hemi-Fontan procedure. Ann Thorac Surg 55:1508–1512
Fogel MA, Weinberg PM, Chin AJ, Fellows KE, Hoffman EA (1996) Late ventricular geometry and performance changes of functional single ventricle throughout staged Fontan reconstruction assessed by magnetic resonance imaging. J Am Coll Cardiol 28:212–221
Hopkins RA, Armstrong BE, Serwer GA, Peterson RJ, Oldham HN Jr (1985) Physiological rationale for a bidirectional cavopulmonary shunt a versatile complement to the Fontan principle. J Thorac Cardiovasc Surg 90:391–398
Tideman E, Marsál K, Ley D (2007) Cognitive function in young adults following intrauterine growth restriction with abnormal fetal aortic blood flow. Ultrasound Obstet Gynecol 29:614–618
Rosenbaum JL, Almli CR, Yundt KD, Altman DI, Powers WJ (1997) Higher neonatal cerebral blood flow correlates with worse childhood neurologic outcome. Neurology 49:1035–1041
Chang L, Anderson T, Migneco OA, Boone K, Mehringer CM, Villanueva-Meyer J, Berman N, Mena I (1993) Cerebral abnormalities in myotonic dystrophy. Cerebral blood flow, magnetic resonance imaging, and neuropsychological tests. Arch Neurol 50:917–923
Koide H, Kobayashi S, Kitani M, Tsunematsu T, Nakazawa Y (1994) Improvement of cerebral blood flow and cognitive function following pacemaker implantation in patients with bradycardia. Gerontology 40:279–285
Li J, Hoskote A, Hickey C, Stephens D, Bohn D, Holtby H, Van Arsdell G, Redington AN, Adatia I (2005) Effect of carbon dioxide on systemic oxygenation, oxygen consumption, and blood lactate levels after bidirectional superior cavopulmonary anastomosis. Crit Care Med 33:984–989
Fogel MA, Durning S, Wernovsky G, Pollock AN, Gaynor JW, Nicolson S (2004) Brain versus lung: hierarchy of feedback loops in single-ventricle patients with superior cavopulmonary connection. Circulation 110((11 Suppl 1)):II147–II152
Hoskote A, Li J, Hickey C, Erickson S, Van Arsdell G, Stephens D, Holtby H, Bohn D, Adatia I (2004) The effects of carbon dioxide on oxygenation and systemic, cerebral, and pulmonary vascular hemodynamics after the bidirectional superior cavopulmonary anastomosis. J Am Coll Cardiol 44:1501–1509
Bradley SM, Simsic JM, Mulvihill DM (1998) Hyperventilation impairs oxygenation after bidirectional superior cavopulmonary connection. Circulation 98(19 Suppl):II372–II376; discussion, II376–II377
Chang AC, Zucker HA, Hickey PR, Wessel DL (1995) Pulmonary vascular resistance in infants after cardiac surgery: role of carbon dioxide and hydrogen ion. Crit Care Med 23:568–574
Karsli C, Luginbuehl I, Farrar M, Bissonnette B (2003) Cerebrovascular carbon dioxide reactivity in children anaesthetized with propofol. Paediatr Anaesth 13:26–31
McNeill BR, Murkin JM, Farrar JK, Gelb AW (1990) Autoregulation and the CO2 responsiveness of cerebral blood flow after cardiopulmonary bypass. Can J Anaesth 37:313–317
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindström L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Piquilloud L, Vignaux L, Bialais E, Roeseler J, Sottiaux T, Laterre PF, Jolliet P, Tassaux D (2011) Neurally adjusted ventilatory assist improves patient-ventilator interaction. Intensive Care Med 37:263–271
Grasselli G, Beck J, Mirabella L, Pesenti A, Slutsky AS, Sinderby C (2012) Assessment of patient-ventilator breath contribution during neurally adjusted ventilatory assist. Intensive Care Med 38:1224–1232
Adatia I, Atz AM, Wessel DL (2005) Inhaled nitric oxide does not improve systemic oxygenation after the bidirectional superior cavopulmonary anastomosis. J Thorac Cardiovasc Surg 129:217–219
Aeba R, Katogi T, Kashima I, Omoto T, Kawada S, Omae K (2000) Factors influencing arterial oxygenation after bidirectional cavopulmonary shunt without additional sources of pulmonary blood flow. J Thorac Cardiovasc Surg 120:589–595
Bradley SM, Simsic JM, Mulvihill DM (2003) Hypoventilation improves oxygenation after bidirectional superior cavopulmonary connection. J Thorac Cardiovasc Surg 126:1033–1039
Salim MA, Case CL, Sade RM, Watson DC, Alpert BS, DiSessa TG (1995) Pulmonary/systemic flow ratio in children after cavopulmonary anastomosis. J Am Coll Cardiol 25:735–738
Kety SS, Schmidt CR (1946) The effects of active and passive hyperventilation on cerebral blood flow, cerebral oxygen consumption, cardiac output, and blood pressure of normal young men. J Clin Invest 25:107–119
Lakshminrusimha S, Steinhorn RH, Wedgwood S, Savorgnan F, Nair J, Mathew B, Gugino SF, Russell JA, Swartz DD (2011) Pulmonary hemodynamics and vascular reactivity in asphyxiated term lambs resuscitated with 21 and 100 % oxygen. J Appl Physiol 111:1441–1447
Fullerton DA, Kirson LE, St Cyr JA, Kinnard T, Whitman GJ (1993) Influence of hydrogen ion concentration versus carbon dioxide tension on pulmonary vascular resistance after cardiac operation. J Thorac Cardiovasc Surg 106:528–536
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P, Slutsky AS (2007) Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 131:711–717
Colombo D, Cammarota G, Bergamaschi V, De Lucia M, Corte FD, Navalesi P (2008) Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med 34:2010–2018
Terzi N, Pelieu I, Guittet L, Ramakers M, Seguin A, Daubin C, Charbonneau P, du Cheyron D, Lofaso F (2010) Neurally adjusted ventilatory assist in patients recovering spontaneous breathing after acute respiratory distress syndrome: physiological evaluation. Crit Care Med 38:1830–1837
Lellouche F, Brochard L (2009) Advanced closed loops during mechanical ventilation (PAV, NAVA, ASV, SmartCare). Best Pract Res Clin Anaesthesiol 23:81–93
Walsh MA, Merat M, La Rotta G, Joshi P, Joshi V, Tran T, Jarvis S, Caldarone CA, Van Arsdell GS, Redington AN, Kavanagh BP (2011) Airway pressure release ventilation improves pulmonary blood flow in infants after cardiac surgery. Crit Care Med 39:2599–2604
Ogawa Y, Iwasaki K, Aoki K, Gokan D, Hirose N, Kato J, Ogawa S (2010) The different effects of midazolam and propofol sedation on dynamic cerebral autoregulation. Anesth Analg 111:1279–1284
Karsli C, Luginbuehl I, Farrar M, Bissonnette B (2002) Propofol decreases cerebral blood flow velocity in anesthetized children. Can J Anaesth 49:830–834
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no conflicts of interests to declare.
Human Participants and/or Animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Zhu, L., Xu, Z., Gong, X. et al. Mechanical Ventilation After Bidirectional Superior Cavopulmonary Anastomosis for Single-Ventricle Physiology: A Comparison of Pressure Support Ventilation and Neurally Adjusted Ventilatory Assist. Pediatr Cardiol 37, 1064–1071 (2016). https://doi.org/10.1007/s00246-016-1392-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1392-9