Abstract
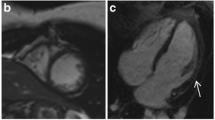
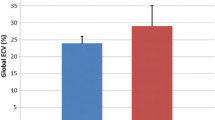
The goal of our study was to characterize the degree of myocardial fibrosis and left ventricular dysfunction in our cohort of Duchenne muscular dystrophy (DMD) carriers using cardiac magnetic resonance imaging (CMR). Seventy percent of males with DMD have mothers who are carriers of the Xp21 mutation. Carrier phenotypic characteristics range from asymptomatic to left ventricular (LV) dysfunction and cardiomyopathy. The true prevalence of cardiac involvement in DMD carriers is unknown. We performed a retrospective observational study. All female DMD carriers who underwent clinical CMR studies at Cincinnati Children’s Hospital Medical Center from December 6, 2006, to August 28, 2013, were evaluated. Patients underwent standard CMR assessment with LV function assessment and late gadolinium enhancement (LGE). In addition, offline feature tracking strain analysis was performed on the basal, mid, and apical short axis. Twenty-two patients were studied, of which 20 underwent adequate testing for myocardial LGE. Four of 22 patients (18 %) were found to have LV dysfunction (ejection fraction <55 %). Seven of 20 DMD carriers (35 %) were found to have LGE. The patients with evidence of LGE had an overall trend to lower absolute deformation parameters; however, this did not meet statistical significance when correcting for multiple comparisons. Our study demonstrates a high rate of LGE as well as LV dysfunction in DMD carriers. Cardiovascular and musculoskeletal symptoms were not statistically different between those with and without cardiac involvement. This study demonstrates the importance of surveillance CMR evaluation of DMD carriers.




Similar content being viewed by others
Abbreviations
- AAP:
-
American Academy of Pediatrics
- ACE:
-
Angiotensin-converting enzyme
- CMR:
-
Cardiac magnetic resonance
- DMD:
-
Duchenne muscular dystrophy
- EF:
-
Ejection fraction
- FT:
-
Feature tracking
- Gd-DTPA:
-
Gadolinium diethylene triamine penta-acetic acid
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- SSFP:
-
Steady-state free precession
References
American Academy of Pediatrics Section on Cardiology Cardiac Surgery (2005) Cardiovascular health supervision for individuals affected by Duchenne or Becker muscular dystrophy. Pediatrics 116(6):1569–1573
Augustine D, Lewandowski AJ, Lazdam M, Rai A, Francis J, Myerson S et al (2013) Global and regional left ventricular myocardial deformation measures by magnetic resonance feature tracking in healthy volunteers: comparison with tagging and relevance of gender. J Cardiovasc Magn Reson 15:8
Bobo JK, Kenneson A, Kolor K, Brown MA (2009) Adherence to american academy of pediatrics recommendations for cardiac care among female carriers of duchenne and becker muscular dystrophy. Pediatrics 123(3):e471–e475
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4):539–542
Cohen N, Muntoni F (2004) Multiple pathogenetic mechanisms in X linked dilated cardiomyopathy. Heart 90(8):835–841
Duboc D, Meune C, Lerebours G et al (2005) Effect of perindopril on the onset and progression of left ventricular dysfunction in Duchenne muscular dystrophy. J Am Coll Cardiol 45(6):855–857
Finsterer J, Stollberger C (2003) The heart in human dystrophinopathies. Cardiology 99(1):1–19
Gotte MJ, Germans T, Russel IK, Zwaneburg JJ, Marcus JT, van Rossum AC, van Velduisen DJ (2006) Myocardial strain and torsion quantified by cardiovascular magnetic resonance tissue tagging: studies in normal and impaired left ventricular function. J Am Coll Cardiol 48(10):2002–2011
Grain L, Cortina-Borja M, Forfar C, Hilton-Jones D, Hopkin J, Burch M (2001) Cardiac abnormalities and skeletal muscle weakness in carriers of Duchenne and Becker muscular dystrophies and controls. Neuromuscul Disord 11(2):186–191
Greenberg NL, Firstenberg MS, Castro PL, Castro PL, Main M, Travaglini A et al (2002) Doppler-derived myocardial systolic strain rate is a strong index of left ventricular contractility. Circulation 105(1):99–105
Hoogerwaard EM, van der Wouw PA, Wilde AA, Bakker E, Ippel PF, Oosterwijk JC et al (1999) Cardiac involvement in carriers of Duchenne and Becker muscular dystrophy. Neuromusc Disord 9(5):347–351
Hor KN, Wansapura J, Markham LW, Mazur W, Cripe LH, Fleck R et al (2009) Circumferential strain analysis identifies strata of cardiomyopathy in Duchenne muscular dystrophy: a cardiac magnetic resonance tagging study. J Am Coll Cardiol 53(14):1204–1210
Hor KN, Gottliebson WM, Carson C, Wash E, Cnota J, Fleck R et al (2010) Comparison of magnetic resonance feature tracking for strain calculation with harmonic phase imaging analysis. JACC Cardiovasc Imaging 3(2):144–151
Ishikawa Y, Bach JR, Minami R (1999) Cardioprotection for Duchenne’s muscular dystrophy. Am Heart J 137(5):895–902
Jefferies JL, Eidem BW, Belmont JW, Craigen WJ, Ware SM, Fernback SD et al (2005) Genetic predictors and remodeling of dilated cardiomyopathy in muscular dystrophy. Circulation 112(18):2799–2804
Lewandowski AJ, Augustine D, Lamata P, Davis EF, Lazdam M, Francis J et al (2013) Preterm heart in adult life: cardiovascular magnetic resonance reveals distinct differences in left ventricular mass, geometry, and function. Circulation 127(2):197–206
Mavrogeni S, Bratis K, Papavasiliou A, Skouteli E, Karanasios E, Georgakopoulos D et al (2013) CMR detects subclinical cardiomyopathy in mother-carriers of Duchenne and Becker muscular dystrophy. JACC Cardiovasc Imaging 6(4):526–528
Pennell DJ, Sechtem UP, Higgins CB, Manning WJ, Pohost GM, Rademakers FE et al (2004) Clinical indications for cardiovascular magnetic resonance (CMR): consensus Panel report. J Cardiovasc Magn Reson 6(4):727–765
Perloff JK, Henze E, Schelbert HR (1984) Alterations in regional myocardial metabolism, perfusion, and wall motion in Duchenne muscular dystrophy studied by radionuclide imaging. Circulation 69(1):33–42
Pohost GM, Hung L, Doyle M (2003) Clinical use of cardiovascular magnetic resonance. Circulation 108(6):647–653
Politano L, Nigro V, Nigro G, Petretta VR, Passamano L, Papparella S et al (1996) Development of cardiomyopathy in female carriers of Duchenne and Becker muscular dystrophies. JAMA 275(17):1335–1338
Rafael-Fortney JA, Chimanji NS, Schill KE, Martin CD, Murray JD, Ganguly R et al (2011) Early treatment with lisinopril and spironolactone preserves cardiac and skeletal muscle in Duchenne muscular dystrophy mice. Circulation 124(5):582–588
Schade van Westrum SM, Hoogerwaard EM, Dekker L, Standaar TS, Bakker E, Ippel PF et al (2011) Cardiac abnormalities in a follow-up study on carriers of Duchenne and Becker muscular dystrophy. Neurology 77(1):62–66
Silva MC, Meira ZM, Gurgel Giannetti J, da Silva MM, Campos AF, Barbosa Mde M et al (2007) Myocardial delayed enhancement by magnetic resonance imaging in patients with muscular dystrophy. J Am Coll Cardiol 49(18):1874–1879
Verhaert D, Richards K, Rafael-Fortney JA, Raman SV (2011) Cardiac involvement in patients with muscular dystrophies: magnetic resonance imaging phenotype and genotypic considerations. Circ Cardiovasc Imaging 4(1):67–76
White JA, Patel MR (2007) The role of cardiovascular MRI in heart failure and the cardiomyopathies. Cardiol Clin 25(1):71–95
Yilmaz A, Gdynia HJ, Ludolph AC, Klingel K, Kandolf R, Sechtem U (2010) Images in cardiovascular medicine. Cardiomyopathy in a Duchenne muscular dystrophy carrier and her diseased son: similar pattern revealed by cardiovascular MRI. Circulation 121(10):e237-9
Acknowledgments
The authors declare that they have no competing interests.
Conflict of interest
No conflicts to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
S.M. Lang and S. Shugh contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Lang, S.M., Shugh, S., Mazur, W. et al. Myocardial Fibrosis and Left Ventricular Dysfunction in Duchenne Muscular Dystrophy Carriers Using Cardiac Magnetic Resonance Imaging. Pediatr Cardiol 36, 1495–1501 (2015). https://doi.org/10.1007/s00246-015-1192-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1192-7