Abstract
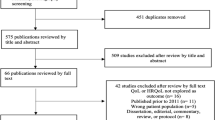
Families of children with congenital heart disease (CHD) cope differently depending on individual and familial factors beyond the severity of the child’s condition. Recent research has shifted from an emphasis on the psychopathology of family functioning to a focus on the resilience of families in coping with the challenges presented by a young child’s condition. The increasing number of studies on the relationship between psychological adaptation, parental coping and parenting practices and quality of life in families of children with CHD necessitates an in-depth re-exploration. The present study reviews published literature in this area over the past 25 years to generate evidence to inform clinical practice, particularly to better target parent and family interventions designed to enhance family coping. Twenty-five studies were selected for inclusion, using the PRISMA guidelines. Thematic analysis identified a number of themes including psychological distress and well-being, gender differences in parental coping, and variable parenting practices and a number of subthemes. There is general agreement in the literature that families who have fewer psychosocial resources and lower levels of support may be at risk of higher psychological distress and lower well-being over time, for both parent and the child. Moreover, familial factors such as cohesiveness and adaptive parental coping strategies are necessary for successful parental adaptation to CHD in their child. The experiences, needs and ways of coping in families of children with CHD are diverse and multi-faceted. A holistic approach to early psychosocial intervention should target improved adaptive coping and enhanced productive parenting practices in this population. This should lay a strong foundation for these families to successfully cope with future uncertainties and challenges at various phases in the trajectory of the child’s condition.

Similar content being viewed by others
References
Almesned S, Al-Akhfash A, Mesned AA (2013) Social impact on families of children with complex congenital heart disease. Ann Saudi Med 33(2):140
Arafa MA, Zaher SR, El-Dowaty AA, Moneeb DE (2008) Quality of life among parents of children with heart disease. Health Qual Life Outcomes 6:91. doi:10.1186/1477-7525-6-91
Berant E, Mikulincer M, Shaver PR (2008) Mothers’ attachment style, their mental health, and their children’s emotional vulnerabilities: a 7-year study of children with congenital heart disease. J Personal 76(1):31–65. doi:10.1111/j.1467-6494.2007.00479.x
Bright MA, Franich-Ray C, Anderson V, Northam E, Cochrane A, Menahem S, Jordan B (2013) Infant cardiac surgery and the father–infant relationship: feelings of strength, strain, and caution. Early Hum Dev 89(8):593–599. doi:10.1016/j.earlhumdev.2013.03.001
Brosig CL, Mussatto KA, Kuhn EM, Tweddell JS (2007) Psychosocial outcomes for preschool children and families after surgery for complex congenital heart disease. Pediatr Cardiol 28(4):255–262
Brosig CL, Whitstone BN, Frommelt MA, Frisbee SJ, Leuthner SR (2007) Psychological distress in parents of children with severe congenital heart disease: the impact of prenatal versus postnatal diagnosis. J Perinatol 27(11):687–692. doi:10.1038/sj.jp.7211807
Bruce E, Lilja C, Sundin K (2014) Mothers’ lived experiences of support when living with young children with congenital heart defects. J Spec Pediatr Nurs 19(1):54–67. doi:10.1111/jspn.12049
Carey LK, Nicholson BC, Fox RA (2002) Maternal factors related to parenting young children with congenital heart disease. J Pediatr Nurs 17(3):174–183. doi:10.1053/jpdn.2002.124111
Committee on Health and Behavior: Research, Practice, and Policy, Board on Neuroscience and Behavioral Health (2001) Health and behavior: The interplay of biological, behavioral and societal influences Washington: National Academies Press
Connor JA, Kline NE, Mott S, Harris SK, Jenkins KJ (2010) The meaning of cost for families of children with congenital heart disease. J Pediatr Health Care 24(5):318–325. doi:10.1016/j.pedhc.2009.09.002
Dale M, Solberg Ø, Holmstrøm H, Landolt M, Eskedal L, Vollrath M (2012) Mothers of infants with congenital heart defects: well-being from pregnancy through the child’s first six months. Qual Life Res 21(1):115–122. doi:10.1007/s11136-011-9920-9
Davis CC, Brown RT, Bakeman R, Campbell R (1998) Psychological adaptation and adjustment of mothers of children with congenital heart disease: stress, coping, and family functioning. J Pediatr Psychol 23(4):219–228
Doherty N, McCusker CG, Molloy B, Mulholland C, Rooney N, Craig B, Sands A, Stewart M, Casey F (2009) Predictors of psychological functioning in mothers and fathers of infants born with severe congenital heart disease. J Reprod Infant Psychol 27(4):390–400. doi:10.1080/02646830903190920
Franck LS, McQuillan A, Wray J, Grocott MPW, Goldman A (2010) Parent stress levels during children’s hospital recovery after congenital heart surgery. Pediatr Cardiol 31(7):961–968. doi:10.1007/s00246-010-9726-5
Franich-Ray C, Bright MA, Anderson V, Northam E, Cochrane A, Menahem S, Jordan B (2013) Trauma reactions in mothers and fathers after their infant’s cardiac surgery. J Pediatr Psychol 38(5):494–505. doi:10.1093/jpepsy/jst015
Frydenberg E, Deans E (2012) The early years coping project: building a shared language of coping. In: Molinelli B, Grimaldo V (eds) Handbook of psychology of Coping: New Research. Nova Publishers, New York, pp 225–242
Goldbeck L, Melches J (2005) Quality of life in families of children with congenital heart disease. Qual Life Res 14(8):1915–1924. doi:10.1007/s11136-005-4327-0
Goldbeck L, Melches J (2006) The impact of the severity of disease and social disadvantage on quality of life in families with congenital cardiac disease. Cardiol Young 16(1):67–75
Goldberg S, Simmons RJ, Newman J, Campbell K, Fowler RS (1991) Congenital heart disease, parental stress, and infant-mother relationships. J Pediatr 119(4):661–666. doi:10.1016/S0022-3476(05)82425-4
Graetz BW, Shute RH, Sawyer MG (2000) An Australian study of adolescents with cystic fibrosis: perceived supportive and non-supportive behaviours from family and friends and psychological adjustment. J Adolesc Health 26:64–67
Graf A, Landolt MA, Mori AC, Boltshauser E (2006) Quality of life and psychological adjustment in children and adolescents with neurofibromatosis type 1. J Pediatr 149:348–353
Green A, Meaux J, Huett A, Ainley K (2009) Constantly responsible, constantly worried, constantly blessed: parenting after pediatric heart transplant. Prog Transpl 19(2):122–127
Grootenhuis MA, Last BF (1995) Adjustment and coping by parents of children with cancer: a review of the literature. Support Care Cancer 5:466–484
Hiscock H, Williams L, Incledon E, Flowers A (2012) Supporting mental health, resilience and wellbeing in families experiencing a childhood chronic illness: A synthesis of evidence to support the Childhood Illness Resilience Program. Prepared for the Hunter Institute of Mental Health. Melbourne: Centre for Community Child Health & Murdoch Children’s Research Institute
Hoddap R, Dykens E, Masino L (1997) Families of children with Prader-Willi syndrome—stress-support and relations to child characteristics. J Autism Dev Disord 27(1):11–24
Jackson AC, Tsantefski M, Goodman H, Johnson B, Rosenfeld J (2003) The Psychosocial impacts on families of low-incidence, complex conditions in children: the case of craniopharyngioma. Soc Work Health Care 38(1):81–107
Jackson AC, Stewart H, O’Toole M, Tokatlian N, Enderby K, Miller J, Ashley D (2007) Pediatric brain tumour patients: their parents’ perceptions of the hospital experience. J Pediatr Oncol Nurs 24(2):95–105
Jackson AC, Enderby K, O’Toole M, Thomas SA, Ashley D, Rosenfeld JV, Simos E, Tokatlian N, Gedye R (2009) The role of social support in families coping with childhood brain tumour. J Psychosoc Oncol 27(1):1–24
Kazak AE (2006) Pediatric psychosocial preventative health model (PPPHM): research, practice and collaboration in pediatric family systems medicine. Fam Syst Health 24:381–395
Kazak AE, Nachman GS (1991) Family research on childhood chronic illness: pediatric oncology as an example. J Fam Psychol 4(4):462–483
Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R et al (1997) Posttraumatic stress, family functioning and social support in survivors of childhood leukaemia and their mothers and fathers. J Consult Clin Psychol 65:120–129
Kazak AE, Cant MC, Jensen M, McSherry M, Rourke M, Hwang W-T et al (2003) Identifying psychosocial risk indicative of subsequent resource utilization in families of newly diagnosed pediatric oncology patients. J Clin Oncol 21:3220–3225
Kazak AE, Rourke MT, Alderfer MA, Pai ALH, Reilly AF, Meadows AT (2007) Evidence-based assessment, intervention and psychosocial care in pediatric oncology: a blueprint for comprehensive services across treatment. J Pediatr Psychol 32(9):1099–1110
Kupst M (1992) Long-term family coping with acute lymphoblastic leukemia in childhood. In: La Greca AM, Siegel LJ, Wallander JL, Walker CE (eds) Stress and coping in child health. The Guilford Press, New York
Kupst M, Shulman JL (1988) Long-term coping with pediatric leukemia: a six-year follow-up study. J Pediatr Psychol 13(1):7–22
Kupst M, Natta MB, Richardson CC, Sculman JL, Lavigne JV, Das L (1995) Family coping with pediatric leukemia: ten years after treatment. J Pediatr Psychol 20(5):601–617
Landolt MA, Buechel EV, Latal B (2011) Predictors of parental quality of life after child open heart surgery: a 6-month prospective study. J Pediatr 158(1):37–43. doi:10.1016/j.jpeds.2010.06.037
Lawoko S, Soares JJF (2002) Distress and hopelessness among parents of children with congenital heart disease, parents of children with other diseases, and parents of healthy children. J Psychosom Res 52(4):193–208. doi:10.1016/S0022-3999(02)00301-X
Lawoko S, Soares JJF (2006) Psychosocial morbidity among parents of children with congenital heart disease: a prospective longitudinal study. Heart Lung: J Acute Crit Care 35(5):301–314. doi:10.1016/j.hrtlng.2006.01.004
Martin C, Nisa M (1996) Meeting the needs of children and families in chronic illness and disease: a greater role for the G.P.? Aust Fam Physician 25(8):1273–1281
Menon S, Valentini RP, Kapur G, Layfield S, Mattoo TK (2009) Effectiveness of a multidisciplinary clinic in managing children with chronic kidney disease. Clin J Am Soc Nephrol 4(7):1170–1175
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. doi:10.7326/0003-4819-151-4-200908180-00135
Pai ALH, Patino-Fernandez AM, McSherry M, Beele D, Alderfer MA, Reilly AT, Hwang W-T, Kazak AE (2008) The Psychosocial Assessment Tool (PAT2.) psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. J Pediatr Psychol 33(1):50–62
PRISMA. (2012). PRISMA endorsers. Retrieved from: http://www.prisma-statement.org/statement.htm
Rempel GR, Rogers LG, Ravindran V, Magill-Evans J (2012) Facets of parenting a child with hypoplastic left heart syndrome. Nurs Res Pract. doi:10.1155/2012/714178
Rempel GR, Ravindran V, Rogers LG, Magill-Evans J (2013) Parenting under pressure: a grounded theory of parenting young children with life-threatening congenital heart disease. J Adv Nurs 69(3):619–630. doi:10.1111/j.1365-2648.2012.06044.x
Rodenburg R, Marle Meijer A, Dekovic M, Aldenkamp AP (2006) Family predictors of psychopathology in children with epilepsy. Epilepsia 47:601–614
Sanger MS, Copeland DR, Davidson ER (1991) Psychosocial adjustment among paediatric cancer patients: a multidimensional assessment. J Paediatr Psychol 16:463–474
Sarajuuri A, Lönnqvist T, Schmitt F, Almqvist F, Jokinen E (2012) Patients with univentricular heart in early childhood: parenting stress and child behaviour. Acta Paediatr 101(3):252–257. doi:10.1111/j.1651-2227.2011.02509.x
Sawyer M, Spurrier N (1996) Families, parents and chronic childhood illness. Family Matters 44:12–15
Sawyer M, Antoniou G, Toogood I, Rice M (1997) Childhood cancer: a two-year prospective study of the psychological adjustment of children and parents. J Am Acad Child Adolesc Psychiatry 36(12):1736–1743
Scholler G, Kasparian N, Winlaw D (2011) How to treat: congenital heart disease. Australian Doctor, 21st October. http://www.australiandoctor.com.au/cmspages/getfile.aspx?guid=e534f9bb-15fe-4691-8f3e-71d9007f4e1c
Scott I, Vaughan L, Bell D (2009) Effectiveness of acute medical units in hospital: a systematic review. Int J Qual Health Care 21(6):397–407
Sloper P (1996) Needs and responses of parents following the diagnosis of childhood cancer. Child: Care Health Dev 22(3):187–202
Spijkerboer AW, Helbing WA, Bogers AJJC, Van Domburg RT, Verhulst FC, Utens EMWJ (2007) Long-term psychological distress, and styles of coping, in parents of children and adolescents who underwent invasive treatment for congenital cardiac disease. Cardiol Young 17(6):638–645
Swallow VM, Jacoby A (2001) Mother’s coping with childhood chronic illness: the effect of presymptomatic diagnosis of vesicoureric reflux. J Adv Nurs 33(1):69–78
Tak YR, McCubbin M (2002) Family stress, perceived social support and coping following the diagnosis of a child’s congenital heart disease. J Adv Nurs 39(2):190–198. doi:10.1046/j.1365-2648.2002.02259.x
Theofanidis D (2007) Chronic illness in childhood: psychosocial adaptation and nursing support for the child and family. Health Sci J 1(2). http://www.hsj.gr/index.files/VOLUME1_2.htm
Thompson RJ Jr, Armstrong FD, Link CL, Pegelow CH, Moser F, Wang WC (2003) A prospective study of the relationship over time of behavior problems, intellectual functioning, and family functioning in children with sickle cell disease: a report from the cooperative study of sickle cell disease. J Pediatr Psychol 28:59–65
Vrijmoet-Wiersma CMJ, Ottenkamp J, van Roozendaal M, Grootenhuis MA, Koopman HM (2009) A multicentric study of disease-related stress, and perceived vulnerability, in parents of children with congenital cardiac disease. Cardiol Young 19(6):608–614. doi:10.1017/S1047951109991831
Woods NF, Haberman MR, Packard NJ (1993) Demands of illness and individual, dyadic, and family adaptation in chronic illness. West J Nurs Res 15(1):10–30
Wray J, Sensky T (2004) Psychological functioning in parents of children undergoing elective cardiac surgery. Cardiol Young 14(2):131–139
Acknowledgments
This review was undertaken as part of a larger study, the Heart Child Family Project, conducted by the Heart Research Centre (HRC) and the Melbourne Graduate School of Education, University of Melbourne, funded by HeartKids Australia under the 2014 Grants-in-Aid program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jackson, A.C., Frydenberg, E., Liang, R.PT. et al. Familial Impact and Coping with Child Heart Disease: A Systematic Review. Pediatr Cardiol 36, 695–712 (2015). https://doi.org/10.1007/s00246-015-1121-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1121-9