Abstract
Few recent studies have assessed the epidemiology of health care-associated infections (HAIs) in the pediatric population after cardiac surgery. A retrospective cohort study was performed to assess the epidemiology of several types of HAIs in children 18 years of age or younger undergoing cardiac surgery from July 2010 to June 2012. Potential pre-, intra-, and postoperative risk factors, including adherence to the perioperative antibiotic prophylaxis regimen at the authors’ hospital, were assessed by multivariable analysis using Poisson regression models. Microorganisms associated with HAIs and their susceptibility patterns were described. Overall, 634 surgeries were performed, 38 (6 %) of which were complicated by an HAI occurring within 90 days after surgery. The HAIs included 7 central line-associated bloodstream infections (CLABSIs), 12 non-CLABSI bacteremias, 6 episodes of early postoperative infective endocarditis (IE), 9 surgical-site infections (SSIs), and 4 ventilator-associated pneumonias (VAPs). Mechanical ventilation (rate ratio [RR] 1.07 per day; 95 % confidence interval [CI] 1.03–1.11; p = 0.0002), postoperative transfusion of blood products (RR 3.12; 95 %, CI 1.38–7.06; p = 0.0062), postoperative steroid use (RR 3.32; 95 % CI 1.56–7.02; p = 0.0018), and continuation of antibiotic prophylaxis longer than 48 h after surgery (RR 2.56; 95 % CI 1.31–5.03; p = 0.0062) were associated with HAIs. Overall, 66.7 % of the pathogens associated with SSIs were susceptible to cefazolin, the perioperative antibiotic prophylaxis used by the authors’ hospital. In conclusion, HAIs occurred after 6 % of cardiac surgeries. Bacteremia and CLABSI were the most common. This study identified several potentially modifiable risk factors that suggest interventions. Further studies should assess the role of improving adherence to perioperative antibiotic prophylaxis, the age of transfused red blood cells, and evidence-based guidelines for postoperative steroids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States, 36,000 children are born each year with congenital heart disease, and currently, 1.3 million children and adults are alive with a history of congenital heart disease [36]. Despite advances in survival, postoperative infections remain a significant cause of morbidity and mortality in children undergoing cardiac surgery for both congenital and acquired heart disease [25]. The postoperative course of 2.7–8 % of these patients is complicated by a hospital-associated infection (HAI) such as a surgical-site infection (SSI) or a bloodstream infection (BSI) [25, 34]. These HAIs can contribute to increased hospital length of stay (LOS) and medical expenses [35]. Postoperative mediastinitis, for example, is associated with an increased mortality rate, a prolonged LOS, and poor long-term quality of life [3, 34].
In recent years, numerous patient safety and quality interventions have been implemented in efforts to reduce HAIs. These include strategies to prevent central line (CL)-associated bloodstream infections (CLABSIs) and ventilator-associated pneumonia (VAP) in both pediatric and adult populations [19]. In addition, perioperative antibiotic prophylaxis regimens have been shown to decrease the risk of SSIs [4, 6, 16], but specific recommendations for perioperative prophylaxis in pediatric populations are extrapolated largely from adult data [5].
This study aimed to describe the epidemiology of postoperative HAIs including SSIs, CLABSIs, BSIs, postoperative endocarditis, and VAP among children undergoing cardiac surgery; to delineate the causative organisms and their resistance patterns; and to evaluate potential risk factors for HAIs in this population, including adherence to an institutional perioperative antimicrobial prophylaxis regimen.
Methods
Study Design and Study Site
We performed a retrospective study of children undergoing cardiac surgery from July 1, 2010 to June 30, 2012 who were admitted postoperatively to the pediatric cardiac intensive care unit (PCICU) at NewYork-Presbyterian Morgan Stanley Children’s Hospital, Columbia University Medical Center (CUMC). The PCICU has 14 beds and approximately 650 annual admissions. Institutional Review Board approval from CUMC was granted to perform this study with a waiver of informed consent.
Inclusion and Exclusion Criteria
Surgical procedures were eligible for inclusion if they were performed for patients 18 years of age or younger, if the indication was congenital or acquired heart disease including heart transplantation, and if the patient was admitted postoperatively to the PCICU.
Surgical procedures were excluded if they were performed in patients older than 18 years of age, if a pacemaker was implanted (because the perioperative prophylaxis regimen is different for such procedures), or if the patient died 24 h or less after surgery. Case finding was performed by review of the electronic operating room manager for procedures performed during the study period.
Infection Prevention and Control Strategies for HAIs
New York State has mandatory reporting to the Centers for Disease Control and Prevention’s (CDC) National Healthcare Safety Network (NHSN) for CLABSIs that occur in all intensive care units (ICUs), including the PCICU. Our PCICU participated in the National Association of Children’s Hospitals and Related Institutions (NACHRI) CLABSI reduction collaboration [15]. Insertion and maintenance bundles for CLs have been in use since 2006 and 2008, respectively. We also have had a VAP prevention program since 2010 but do not report VAPs to NHSN. Our PCICU also participates in the Society of Thoracic Surgeons (STS) database [16] and has had a local quality initiative to reduce SSIs since 2011.
Case Findings and Definitions for HAIs
The study team reviewed the electronic medical records (EMRs) of all the subjects for 90 days after surgery to confirm HAIs independently. For the study, NHSN HAI case definitions were used [21]. Briefly, CLABSIs were defined as a blood culture positive for a known pathogen (or two cultures positive for a common skin contaminant) in a patient with a CL and symptoms (e.g., fever, chills, or hypotension) unrelated to another infection. Additionally, in this study, the definition of primary bacteremia was broadened to include a positive blood culture for which an attending physician prescribed a course of intravenous antibiotic therapy.
In this study, SSIs were defined by clinical evidence of a wound infection (e.g., fever and drainage), and VAPs were defined as a combination of signs and symptoms of infection (e.g., fever and elevated white blood cell count), worsening gas exchange, and radiographic changes in a mechanically ventilated patient. Early postoperative IE was defined as a positive blood culture with echocardiographic evidence of vegetations and/or embolic phenomena within 8 weeks of cardiac surgery.
During the study period, CLABSIs, SSIs, and VAPs were assessed in real time by the Department of Infection Prevention and Control and the cardiac surgical team (SSIs). As all positive blood cultures are reviewed for possible CLABSIs by the Department of Infection Prevention and Control, primary bacteremias in patients without CL and episodes of early postoperative infective endocarditis (IE) also were captured. Potential HAIs were discussed, and disagreements were resolved by consensus. The causative pathogens and their antimicrobial susceptibility also were collected.
Potential Risk Factors for HAIs
Potential preoperative risk factors were abstracted from the electronic medical record and included demographic characteristics (e.g., age, sex, race, ethnicity); body mass index (BMI); chronic medical conditions including cardiac disease requiring medication (e.g., furosemide); extracardiac disease including chronic kidney disease, asplenia, and polysplenia; chromosomal abnormalities (e.g., DiGeorge syndrome, Williams syndrome, trisomy 21); and prior immunosuppression (e.g., the use of immunosuppressant medication or steroids).
The potential intraoperative risk factors included use of deep hypothermic circulatory arrest, use of intraoperative steroids, and transfusion of blood products (including packed red blood cells, platelets, or fresh frozen plasma), as well as the durations of cardiopulmonary bypass (CPB), aortic cross-clamp, and surgery.
The potential postoperative risk factors included the use of invasive devices (e.g., pacing wires, CLs, and chest tubes), receipt of blood products or steroids, and delayed closure of the sternal wound. The durations of parenteral nutrition and mechanical ventilation also were calculated.
We measured compliance with our hospital’s perioperative antibiotic prophylaxis regimen. The parameters included correct agent (i.e., cefazolin), correct dose (i.e., 30 mg/kg; maximum dose, 2 g), correct timing (i.e., within 60 min before incision), intraoperative redosing for surgery longer than 4 h, and correct duration (i.e., discontinuation within 48 h after the surgery end time). Continuation of antibiotics or broadening antibiotic coverage for a suspected infection were not considered an incorrect duration of prophylactic antibiotics. Vancomycin (15 mg/kg) was prescribed for patients who had previous colonization or infection with methicillin-resistant Staphylococcus aureus (MRSA) or allergy to β-lactam agents. Vancomycin and gentamicin were prescribed postoperatively for patients with delayed sternal closure and discontinued within 24 h after chest closure.
Statistical Analysis
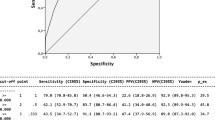
Statistical analysis was performed using SAS 9.3 (version 9.3 for Windows; SAS Institute, Inc., Cary, NC). The risk for HAI was regressed on the aforementioned pre-, intra-, and postoperative risk factors using Poisson regression models in PROC GENMOD (SAS version 9.3; SAS Institute, Inc., Cary, NC). An offset corresponding to the log of person-time was included in the model to provide rate ratios. Patients were censored 90 days after surgery or at the time of the HAI diagnosis, whichever came first.
For medical devices (e.g., CL), person-time was accumulated until the device was removed. If more than one surgical procedure was performed within 1 week, risk factors attributable to the first surgery were analyzed. If two or more surgical procedures were performed more than 1 week apart, each surgical procedure was considered a separate observation. To adjust for nonindependent observations that resulted from a patient having more than one surgery, the repeated statement in the PROC GENMOD was used.
Individual predictors for HAIs were assessed using Poisson regression bivariate analyses. Significant risk factors (p < 0.05) in the bivariate analysis were included in the multivariable analysis. Risk factors highly correlated in the bivariate analysis (r > 0.30) were not included in the multivariable analysis together.
In the risk factor analysis, the mean duration of cardiopulmonary bypass, aortic cross-clamp procedure, and surgery were analyzed for those procedures with and without HAIs. The rate of adherence to individual perioperative antibiotic prophylaxis recommendations (e.g., correct preoperative dose, correct timing of intraoperative redosing) as well as complete adherence to all the perioperative antibiotic prophylaxis recommendations was determined. The association between adherence to these recommendations and HAIs was assessed using a Poisson regression.
We performed an ad hoc power calculation for a sample size of 650, a median follow-up period of 40 days, a minimal detectable rate ratio of 2.0, and a type 1 error of 0.05. This study had a power greater than 99 % to detect significant associations between risk factors and outcomes.
Results
Study Procedures and Population
During the study period, 729 cardiac surgical procedures were performed, and 634 procedures (609 subjects) were eligible for inclusion in the study. A total of 95 surgeries were excluded including 55 surgeries performed in patients older than 18 years, 39 surgeries with pacemaker placement, and 1 surgery associated with death 24 h or less after surgery.
HAIs and Causative Pathogens
In this study, 38 HAIs were diagnosed including 9 SSIs, 7 CLABSIs, 12 BSIs, 4 VAPs, and 6 episodes of IE (Table 1). Three subjects had two HAIs. During the study period, the CLABSI rate was 1.2 per 1,000 CL days, and the VAP rate was 1.0 per 1,000 ventilator days. Six SSIs were superficial, and three were organ-space infections (2 cases of mediastinitis and 1 case of pericarditis). All SSIs presented within 30 days after the surgery.
The pathogens causing HAIs and their susceptibility to cefazolin are shown in Table 1. All nine SSIs were caused by S. aureus, three of which were MRSA. The pathogens causing CLABSIs, BSIs, VAPs, and early postoperative IE were more likely to be resistant to cefazolin than the pathogens causing SSIs (67 vs 28 %, respectively; p = 0.03) and more likely to be Gram-negative pathogens (41 vs 0 %; p = 0.02).
The overall rate of HAIs was 5.99 per 100 surgeries. The rates of individual HAIs ranged from 0.63 VAP per 100 surgical procedures to 1.89 BSIs per 100 surgical procedures (Table 1). The patients with an HAI had an average PCICU stay of 38 days, whereas those without an HAI had an average PCICU stay of 6 days (p < 0.001).
Risk Factors for HAIs
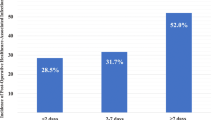
In the bivariate analysis, the preoperative factors significantly associated with HAIs included younger age, race, lower weight, and prior stay in another hospital (Table 2). As the race of 30 % of children was classified as ‘other,’ this analysis did not find that a particular race was associated with an increased risk of HAIs. The intraoperative factors included heart transplantation, longer duration of surgery, transfusion of blood products, and treatment with steroids (Table 2). The postoperative factors included delayed sternal closure, longer duration of chest tube placement, longer duration of mechanical ventilation, transfusion of blood products, and treatment with steroids. The steroids included dexamethasone, methylprednisolone, hydrocortisone, prednisolone, and prednisone given for a mean of 8 days (range 1–99 days). Continuing perioperative antibiotic prophylaxis longer than 48 h after surgery (excluding patients with delayed sternal closure) also was a risk factor for HAIs.
The duration of cardiopulmonary bypass was highly correlated (r > 0.3) with surgery length as well as with intra- and postoperative transfusion of blood products. Thus, the duration of cardiopulmonary bypass was not included in the multivariable model. Postoperative transfusion and duration of mechanical ventilation also were highly correlated (r = 0.38), but both remained statistically significant in the multivariable model (p < 0.05) and were subsequently included in the model.
In the multivariable analysis, mechanical ventilation, postoperative transfusion of blood products, use of postoperative steroids, and continuation of prophylactic antibiotics longer than 48 h after the end of surgery were associated with HAIs (Table 3).
Discussion
During the past decade, increasing efforts have been made to understand the rates and risk factors for HAIs experienced by pediatric patients after cardiac surgery and to reduce these complications [1, 10, 25, 26, 29, 32, 33]. In 2012, the mean pooled CLABSI rate (n = 41 sites) and VAP rate (n = 20 sites) for PCICUs reported to NHSN were 1.4 per 1,000 CL days and 0.2 per 1,000 ventilator days, respectively [13]. At our center, the CLABSI rate was similar to the national mean (1.2 per 1,000 CL days), whereas the VAP rate was higher than the national mean (1.0 per 1,000 ventilator days).
In this study, we identified four potentially modifiable risk factors for HAIs, all of which occurred during the postoperative period. These included prolonged use of perioperative antibiotic prophylaxis, prolonged mechanical ventilation, postoperative steroids, and transfusion of blood products.
The most common HAIs were BSIs (n = 12), CLABSIs (n = 7), and SSIs (n = 9). The majority of SSIs in our study population (6 of 9, 67 %) were caused by methicillin-susceptible S. aureus (MSSA), a microorganism susceptible to cefazolin, our institution’s prophylactic agent. The majority of the patients (5/6) who experienced an MSSA infection had received correct prophylactic antibiotics. This observation raises concern for inadequate tissue levels of cefazolin in children who require cardiopulmonary bypass and aortic cross-clamp procedures. Prior data for infants and adults [2, 18] have suggested that continuous administration of cefazolin may be beneficial because it provides more stable serum levels, lower inter-patient variability, and higher myocardial tissue penetration.
Of the three SSIs caused by MRSA, one patient was known to be colonized with MRSA and had received correct prophylactic antibiotics (i.e., vancomycin). Although it is not our current policy to screen children for MRSA before surgery, others have suggested that active MRSA screening, decolonization, or both can significantly decrease the burden of MRSA HAIs [30, 37].
The clinical benefit of antibiotic prophylaxis after surgery is controversial. To our knowledge, only a single study has addressed this issue for adults undergoing cardiac surgery. The findings showed that continuing antibiotic prophylaxis longer than 48 h after surgery did not reduce SSIs but did increase antimicrobial resistance [19]. Nonetheless, current recommendations, including those of the Surgical Care Improvement Project [4], The Society for Healthcare Epidemiology of America [11], and most recently, the Infectious Diseases Society of America [7] endorse prophylaxis for 48 h after cardiac surgery. However, administration of antibiotics longer than 48 h after surgery has not been shown to reduce the rate of SSIs [14] and can increase the risk of infections with resistant organisms or Clostridium difficile [8, 19]. In the current study, we demonstrated that continuing antibiotics longer than 48 h after surgery was associated with an increase in HAIs.
We also found that increased duration of mechanical ventilation postoperatively was associated with HAIs. We speculate that prolonged intubation is associated with increased LOS and the subsequent risk of HAIs [17]. Furthermore, the invasive nature of endotracheal intubation may increase the risk of HAIs.
Postoperative transfusion of blood products also was a significant risk factor for acquiring an HAI. Studies have shown that a relationship exists between the number of units of blood products received and the number of bacterial infections postoperatively [22]. Furthermore, older age of the transfused red blood cells (RBCs) also may increase the risk of bacteremia. The explanation for this observation is unclear, but theories include the availability of free iron for bacterial growth, adverse effects on macrophage function, alterations in cytokines, and changes in microvascular flow [12, 20]. The use of older RBCs for infants and small children may be of particular concern. For these patients, it is a frequent practice for one unit of blood to be transfused in small aliquots over weeks to avoid potential exposure to multiple donors and wastage of donated blood [27].
As previously described [28], the use of steroids postoperatively also was associated with HAIs in our patient population. Steroids may be used during the postoperative period to blunt the inflammatory response to cardiopulmonary bypass [9, 24] and to facilitate extubation [23]. In the current study, steroids remained a risk factor for HAIs in the multivariable analysis with adjustment for prolonged intubation. However, too few patients underwent heart transplantation for the risk of steroids to be assessed with adjustment for transplantation.
This study had several limitations. It was a single center study, which limits the generalizability of the findings. At our institution, most neonates undergoing cardiac surgery receive their postoperative care in a neonatal cardiac care ICU. We have studied risk factors for BSIs and SSIs in the infant population and have found that incorrect preoperative antibiotic prophylaxis timing is a risk factor for SSIs [31]. Although HAIs were assessed prospectively, potential risk factors were collected retrospectively. We were unable to determine the risk factors for each type of HAI due to the small number of HAIs in our study.
Furthermore, catheter-associated urinary tract infections were not included because this HAI was not tracked at our institution until 2012. We did not assess the age of transfused RBCs due to a lack of power and because the analysis of transfusions included packed RBCs, platelets, and fresh frozen plasma rather than RBCs exclusively. Finally, it is possible that we may have not captured all HAIs if patients presented to another facility after discharge, but it is NHSN practice to report HAIs to the institution at which the original surgery occurred.
Conclusion
To our knowledge, this is one of the few studies in the pediatric population to assess several types of HAIs after cardiac surgery in the era of bundle strategies, quality initiatives, and mandatory HAI reporting. Whereas perioperative prophylaxis guidelines have been developed for adult populations, such guidelines are lacking for the pediatric population.
Our study found four potentially modifiable risk factors including the risk of prolonged perioperative prophylaxis. Our findings also suggest that current policies and practices for transfusions, steroids, and mechanical ventilation should be evaluated to develop strategies for limiting these exposures. Multicenter studies should be performed to assess the validity of our findings.
References
Abou Elella R, Najm HK, Balkhy H, Bullard L, Kabbani MS (2010) Impact of bloodstream infection on the outcome of children undergoing cardiac surgery. Pediatr Cardiol 31:483–489. doi:10.1007/s00246-009-9624-x
Adembri C, Ristori R, Chelazzi C, Arrigucci S, Cassetta MI, De Gaudio AR, Novelli A (2010) Cefazolin bolus and continuous administration for elective cardiac surgery: improved pharmacokinetic and pharmacodynamic parameters. J Thorac Cardiovasc Surg 140:471–475. doi:10.1016/j.jtcvs.2010.03.038
Alphonso N, Anagnostopoulos PV, Scarpace S, Weintrub P, Azakie A, Raff G, Karl TR (2007) Perioperative antibiotic prophylaxis in paediatric cardiac surgery. Cardiol Young 17:12–25
Bratzler DW, Hunt DR (2006) The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 43:322–330
Bratzler DW, Houck PM, Richards C, Steele L, Dellinger EP, Fry DE, Wright C, Ma A, Carr K, Red L (2005) Use of antimicrobial prophylaxis for major surgery: baseline results from the National Surgical Infection Prevention Project. Arch Surg 140:174–182. doi:10.1001/archsurg.140.2.174
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect 14:73–156. doi:10.1089/sur.2013.9999
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 70:195–283
Carignan A, Allard C, Pepin J, Cossette B, Nault V, Valiquette L (2008) Risk of Clostridium difficile infection after perioperative antibacterial prophylaxis before and during an outbreak of infection due to a hypervirulent strain. Clin Infect Dis 46:1838–1843. doi:10.1086/588291
Clarizia NA, Manlhiot C, Schwartz SM, Sivarajan VB, Maratta R, Holtby HM, Gruenwald CE, Caldarone CA, Van Arsdell GS, McCrindle BW (2011) Improved outcomes associated with intraoperative steroid use in high-risk pediatric cardiac surgery. Ann Thorac Surg 91:1222–1227. doi:10.1016/j.athoracsur.2010.11.005
Costello JM, Graham DA, Morrow DF, Morrow J, Potter-Bynoe G, Sandora TJ, Pigula FA, Laussen PC (2010) Risk factors for surgical-site infection after cardiac surgery in children. Ann Thorac Surg 89:1833–1841
Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM (2007) Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 44:159–177
Doctor A, Spinella P (2012) Effect of processing and storage on red blood cell function in vivo. Semin Perinatol 36:248–259. doi:10.1053/j.semperi.2012.04.005
Dudeck MA, Weiner LM, Allen-Bridson K, Malpiedi PJ, Peterson KD, Pollock DA, Sievert DM, Edwards JR (2013) National Healthcare Safety Network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Control 41:1148–1166. doi:10.1016/j.ajic.2013.09.002
Edwards FH, Engelman RM, Houck P, Shahian DM, Bridges CR, Society of Thoracic Surgeons (2006) The Society of Thoracic Surgeons practice guideline series: antibiotic prophylaxis in cardiac surgery, part I: duration. Ann Thorac Surg 81:397–404. doi:10.1016/j.athoracsur.2005.06.034
Edwards JR, Peterson KD, Andrus ML, Tolson JS, Goulding JS, Dudeck MA, Mincey RB, Pollock DA, Horan TC (2007) National Healthcare Safety Network (NHSN) Report, data summary for 2006, issued June 2007. Am J Infect Control 35:290–301
Engelman R, Shahian D, Shemin R, Guy TS, Bratzler D, Edwards F, Jacobs M, Fernando H, Bridges C (2007) The Society of Thoracic Surgeons practice guideline series: antibiotic prophylaxis in cardiac surgery, part II: antibiotic choice. Ann Thorac Surg 83:1569–1576. doi:10.1016/j.athoracsur.2006.09.046
Farias JA, Frutos F, Esteban A, Flores JC, Retta A, Baltodano A, Alia I, Hatzis T, Olazarri F, Petros A, Johnson M (2004) What is the daily practice of mechanical ventilation in pediatric intensive care units? A multicenter study. Intensive Care Med 30:918–925. doi:10.1007/s00134-004-2225-5
Haessler D, Reverdy ME, Neidecker J, Brule P, Ninet J, Lehot JJ (2003) Antibiotic prophylaxis with cefazolin and gentamicin in cardiac surgery for children less than ten kilograms. J Cardiothorac Vasc Anesth 17:221–225. doi:10.1053/jcan.2003.51S1053077003000260
Harbarth S, Samore MH, Lichtenberg D, Carmeli Y (2000) Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical-site infections and antimicrobial resistance. Circulation 101:2916–2921
Hod EA, Brittenham GM, Billote GB, Francis RO, Ginzburg YZ, Hendrickson JE, Jhang J, Schwartz J, Sharma S, Sheth S, Sireci AN, Stephens HL, Stotler BA, Wojczyk BS, Zimring JC, Spitalnik SL (2011) Transfusion of human volunteers with older, stored red blood cells produces extravascular hemolysis and circulating non-transferrin-bound iron. Blood 118:6675–6682. doi:10.1182/blood-2011-08-371849blood-2011-08-371849
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Houbiers JG, van de Velde CJ, van de Watering LM, Hermans J, Schreuder S, Bijnen AB, Pahlplatz P, Schattenkerk ME, Wobbes T, de Vries JE, Klementschitsch P, van de Maas AH, Brand A (1997) Transfusion of red cells is associated with increased incidence of bacterial infection after colorectal surgery: a prospective study. Transfusion 37:126–134
Khemani RG, Randolph A, Markovitz B (2009) Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev. doi:10.1002/14651858.CD001000.pub3
Kilger E, Weis F, Briegel J, Frey L, Goetz AE, Reuter D, Nagy A, Schuetz A, Lamm P, Knoll A, Peter K (2003) Stress doses of hydrocortisone reduce severe systemic inflammatory response syndrome and improve early outcome in a risk group of patients after cardiac surgery. Crit Care Med 31:1068–1074. doi:10.1097/01.CCM.0000059646.89546.98
Levy I, Ovadia B, Erez E, Rinat S, Ashkenazi S, Birk E, Konisberger H, Vidne B, Dagan O (2003) Nosocomial infections after cardiac surgery in infants and children: incidence and risk factors. J Hosp Infect 53:111–116
Maher KO, VanDerElzen K, Bove EL, Mosca RS, Chenoweth CE, Kulik TJ (2002) A retrospective review of three antibiotic prophylaxis regimens for pediatric cardiac surgical patients. Ann Thorac Surg 74:1195–1200
Mangel J, Goldman M, Garcia C, Spurll G (2001) Reduction of donor exposures in premature infants by the use of designated adenine-saline preserved split red blood cell packs. J Perinatol 21:363–367. doi:10.1038/sj.jp.7210545
Mastropietro CW, Barrett R, Davalos MC, Zidan M, Valentine KM, Delius RE, Walters HL III (2013) Cumulative corticosteroid exposure and infection risk after complex pediatric cardiac surgery. Ann Thorac Surg 95:2133–2139. doi:10.1016/j.athoracsur.2013.02.026
Mehta PA, Cunningham CK, Colella CB, Alferis G, Weiner LB (2000) Risk factors for sternal wound and other infections in pediatric cardiac surgery patients. Pediatr Infect Dis J 19:1000–1004
Mehta S, Hadley S, Hutzler L, Slover J, Phillips M, Bosco JA III (2013) Impact of preoperative MRSA screening and decolonization on hospital-acquired MRSA burden. Clin Orthop Relat Res 471:2367–2371. doi:10.1007/s11999-013-2848-3
Murray MT, Krishnamurthy G, Corda R, Turcotte RF, Jia H, Bacha E, Saiman L (2013) Surgical-site infections and bloodstream infections in infants after cardiac surgery. J Thorac Cardiovasc Surg. doi:10.1016/j.jtcvs.2013.08.048
Nateghian A, Taylor G, Robinson JL (2004) Risk factors for surgical-site infections following open-heart surgery in a Canadian pediatric population. Am J Infect Control 32:397–401
Roeleveld PP, Guijt D, Kuijper EJ, Hazekamp MG, de Wilde RB, de Jonge E (2011) Ventilator-associated pneumonia in children after cardiac surgery in The Netherlands. Intensive Care Med 37:1656–1663. doi:10.1007/s00134-011-2349-3
Sohn AH, Schwartz JM, Yang KY, Jarvis WR, Guglielmo BJ, Weintrub PS (2010) Risk factors and risk adjustment for surgical site infections in pediatric cardiothoracic surgery patients. Am J Infect Control 38:706–710
Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ (2011) Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol 32:101–114. doi:10.1086/657912
Understand your risk for congenital heart defects. Retrieved 25 February 2013 at http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/UnderstandYourRiskforCongenitalHeartDefects/Understand-Your-Risk-for-Congenital-Heart-Defects_UCM_001219_Article.jsp
Zanetti G, Goldie SJ, Platt R (2001) Clinical consequences and cost of limiting use of vancomycin for perioperative prophylaxis: example of coronary artery bypass surgery. Emerg Infect Dis 7:820–827. doi:10.3201/eid0705.010508
Author information
Authors and Affiliations
Corresponding author
Additional information
Rebecca F. Turcotte and Ava Brozovich have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Turcotte, R.F., Brozovich, A., Corda, R. et al. Health Care-Associated Infections in Children After Cardiac Surgery. Pediatr Cardiol 35, 1448–1455 (2014). https://doi.org/10.1007/s00246-014-0953-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-0953-z