Abstract
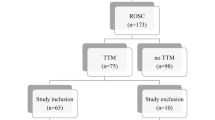
Induced supraventricular tachycardia (SVT) during electrophysiology studies (EPS) can be associated with hemodynamic changes. Traditionally, invasive arterial blood pressure has been used for continuous monitoring of these changes. This prospective study evaluated the efficacy of near-infrared spectroscopy (NIRS) monitoring during SVT. The use of NIRS has expanded with evidence of its accuracy and benefit in detecting cerebral hypoperfusion. This study aimed first to determine the hemodynamic changes associated with electrophysiology testing for SVT and second to determine whether the hemodynamic changes are associated with similar changes in the cerebral saturation as determined by NIRS. The study enrolled 30 patients 5–20 years of age with a history of SVT who underwent an EPS. The demographic data included age, gender, weight, height, and type of SVT. Hemodynamic data (invasive blood pressure and heart rate), NIRS, bispectral index (BIS), end-tidal carbon dioxide, and pulse oximetry were collected before and during three episodes of induced SVT. The linear correlation coefficient (r) was measured to calculate the relationship of the changes in systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) to the changes in NIRS values during the SVT episodes. Data from 22 patients were collected. The induction of SVT was associated mainly with a change in SBP and a less prominent change in DBP and MAP from baseline. The changes in hemodynamic status were associated with minimal changes in cerebral saturations, as evidenced by an average absolute change in NIRS of <1 from baseline value. The changes in hemodynamics were correlated linearly with cerebral saturation. Changes in SBP, DBP, and MAP were correlated positively with changes in NIRS, as denoted by (r) values of 0.52, 0.57, and 0.67 respectively, and a P value less than 0.05 for all three association tests. Induction of SVT during electrophysiology testing is associated with hemodynamic changes, mainly in SBP. In this study, these hemodynamic changes resulted in a minimal decrease in cerebral perfusion, as evidenced by minimal changes in the cerebral saturation measured by NIRS (0.7% from baseline). Although the changes in the cerebral saturation were minimal, these changes were linearly correlated with the changes in the hemodynamics. This study is the first to demonstrate the possible application of NIRS monitoring during EPS and to document that despite changes in the hemodynamic status, the changes in cerebral oxygenation are minimal, thereby confirming the safety of EPS for SVT.

Similar content being viewed by others
References
Fleck T, Schubert S, Redlin M et al (2010) Influence of external cardiac pacing on cerebral oxygenation measured by near-infrared spectroscopy in children after cardiac surgery. Paediatr Anaesth 20:553–558
Goldreyer BN, Kastor JA, Kershbaum KL (1976) The hemodynamic effects of induced supraventricular tachycardia in man. Circulation 54:783–789
Kugler JD, Danford DA, Houston K et al (1997) Radiofrequency catheter ablation for paroxysmal supraventricular tachycardia in children and adolescents without structural heart disease. Pediatric EP society, radiofrequency catheter ablation registry. Am J Cardiol 80:1438–1443
Kuhlkamp V, Bosch R, Mewis C (2001) Syncope and supraventricular tachycardia. Circulation 104:E102
Laurent G, Leong-Poi H, Mangat I et al (2009) Influence of ventriculoatrial timing on hemodynamics and symptoms during supraventricular tachycardia. J Cardiovasc Electrophysiol 20:176–181
Mobilij A, Annunzio ED’, Paloscia L et al (1982) Hemodynamic changes induced by supraventricular tachycardia. G Ital Cardiol 12:327–333
Naguib AN, Winch P, Ro PS et al (2011) Changes in near-infrared spectroscopy and the bispectral index during tilt-table examination. Pediatr Cardiol 32:234–236
Rao RP, Danduran MJ, Dixon JE et al (2010) Near infrared spectroscopy: guided tilt table testing for syncope. Pediatr Cardiol 31:674–679
Sganzerla P, Fabbiocchi F, Grazi S et al (1989) Electrophysiologic and haemodynamic correlates in supraventricular tachycardia. Eur Heart J 10:32–39
Taneja T, Kadish AH, Parker MA et al (2002) Acute blood pressure effects at the onset of supraventricular and ventricular tachycardia. Am J Cardiol 90:1294–1299
Vasdekis SN, Tsivgoulis G, Athanasiadis D, et al (2011) Cerebrovascular reacivity assessment in patients with carotid artery disease: a combined TCD and NIRS study. J Neuroimaging. doi:10.1111/j.1552-6569.2011.00595.x
Zunker P, Haase C, Borggrefe M et al (1998) Cerebral hemodynamics during induced tachycardia in routine electrophysiologic studies: a transcranial Doppler study. Neurol Res 20:504–508
Acknowledgment
The authors acknowledge Julie Rice, BSN, RN, CCRC, and Tami Ackley, RN, for their help with data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hershenson, J.A., Ro, P.S., Miao, Y. et al. Changes in Hemodynamic Parameters and Cerebral Saturation During Supraventricular Tachycardia. Pediatr Cardiol 33, 286–289 (2012). https://doi.org/10.1007/s00246-011-0133-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-011-0133-3