Abstract
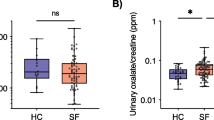
Antibiotics can alter the gut microbiome (GMB), which may be associated with stone disease. We sought to determine the effect that antibiotics have on the GMB, urine ion excretion and stone formation in genetic hypercalciuric stone-forming (GHS) rats. 116th generation GHS rats were fed a fixed amount of a normal calcium (1.2%) and phosphate (0.65%) diet, and divided into three groups (n = 10): control (CTL) diet, or supplemented with ciprofloxacin (Cipro, 5 mg/day) or Bactrim (250 mg/day). Urine and fecal pellets were collected over 6, 12 and 18 weeks. Fecal DNA was amplified across the 16S rRNA V4 region. At 18 weeks, kidney stone formation was visualized by Faxitron and blindly assessed by three investigators. After 18 weeks, urine calcium and oxalate decreased with Bactrim compared to CTL and Cipro. Urine pH increased with Bactrim compared to CTL and Cipro. Urine citrate increased with Cipro compared to CTL and decreased by half with Bactrim. Calcification increased with Bactrim compared to CTL and Cipro. Increased microbial diversity correlated with decreased urinary oxalate in all animals (R = − 0.46, p = 0.006). A potential microbial network emerged as significantly associated with shifts in urinary pH. Bactrim and Cipro differentially altered the GMB of GHS rats. The Bactrim group experienced a decrease in urine calcium, increased CaP supersaturation and increased calcification. The GMB is likely a contributing factor to changes in urine chemistry, supersaturation and stone risk. Further investigation is required to fully understand the association between antibiotics, the GMB and kidney stone formation.





Similar content being viewed by others
Availability of data and material
Available upon request.
References
Litwin M, Saigal C (2012) Economic impact of urologic disease. In: National Institute of Diabetes and Digestive and Kidney Diseases NIoH, US Department of Health and Human Services (ed). Urologic Diseases in America. NIH Publication 12-78652012, p 486
Alexander RT, Hemmelgarn BR, Wiebe N, Bello A, Morgan C, Samuel S et al (2012) Kidney stones and kidney function loss: a cohort study. BMJ 345:e5287
Ferraro PM, Taylor EN, Eisner BH, Gambaro G, Rimm EB, Mukamal KJ et al (2013) History of kidney stones and the risk of coronary heart disease. JAMA 310(4):408–415
Melton LJ 3rd, Crowson CS, Khosla S, Wilson DM, O’Fallon WM (1998) Fracture risk among patients with urolithiasis: a population-based cohort study. Kidney Int 53(2):459–464
Kartha GK, Li I, Comhair S, Erzurum SC, Monga M (2017) Co-occurrence of asthma and nephrolithiasis in children. PLoS One 12(1):e0168813
Lee JA, Abramowitz MK, Kipperman N, Drzewiecki BA, Melamed ML, Stern JM (2020) Exploring the association of asthma with urinary stone disease: results from the National Health and Nutrition Examination Survey 2007–2014. Eur Urol Focus 6(2):354–360
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI (2006) An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444(7122):1027–1031
Vrieze A, Van Nood E, Holleman F, Salojarvi J, Kootte RS, Bartelsman JF et al (2012) Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 143(4):913–916.e7
Wu H, Esteve E, Tremaroli V, Khan MT, Caesar R, Manneras-Holm L et al (2017) Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med 23:850
Everard A, Cani PD (2013) Diabetes, obesity and gut microbiota. Best Pract Res Clin Gastroenterol 27(1):73–83
Wang Z, Klipfell E, Bennett BJ, Koeth R, Levison BS, Dugar B et al (2011) Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472(7341):57–63
Larsen N, Vogensen FK, van den Berg FW, Nielsen DS, Andreasen AS, Pedersen BK et al (2010) Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS One 5(2):e9085
Stern JM, Urban-Maldonado M, Usyk M, Granja I, Schoenfeld D, Davies KP et al (2019) Fecal transplant modifies urine chemistry risk factors for urinary stone disease. Physiol Rep 7(4):e14012
Nobel YR, Cox LM, Kirigin FF, Bokulich NA, Yamanishi S, Teitler I et al (2015) Metabolic and metagenomic outcomes from early-life pulsed antibiotic treatment. Nat Commun 6:7486
Smith AD, Foss ED, Zhang I, Hastie JL, Giordano NP, Gasparyan L et al (2019) Microbiota of MR1 deficient mice confer resistance against Clostridium difficile infection. PLoS One 14(9):e0223025
Cox LM, Blaser MJ (2015) Antibiotics in early life and obesity. Nat Rev Endocrinol 11(3):182–190
Kharlamb V, Schelker J, Francois F, Jiang J, Holmes RP, Goldfarb DS (2011) Oral antibiotic treatment of Helicobacter pylori leads to persistently reduced intestinal colonization rates with Oxalobacter formigenes. J Endourol 25(11):1781–1785
Mittal RD, Kumar R, Bid HK, Mittal B (2005) Effect of antibiotics on Oxalobacter formigenes colonization of human gastrointestinal tract. J Endourol Endourol Soc 19(1):102–106
Tasian GE, Jemielita T, Goldfarb DS, Copelovitch L, Gerber JS, Wu Q et al (2018) Oral antibiotic exposure and kidney stone disease. J Am Soc Nephrol JASN 29(6):1731–1740
Ferraro PM, Curhan GC, Gambaro G, Taylor EN (2019) Antibiotic use and risk of incident kidney stones in female nurses. Am J Kidney Dis 74:736–741
Miller AW, Orr T, Dearing D, Monga M (2019) Loss of function dysbiosis associated with antibiotics and high fat, high sugar diet. ISME J 13(6):1379–1390
Krieger NS, Asplin JR, Granja I, Ramos FM, Flotteron C, Chen L et al (2019) Chlorthalidone is superior to potassium citrate in reducing calcium phosphate stones and increasing bone quality in hypercalciuric stone-forming rats. J Am Soc Nephrol JASN 30(7):1163–1173
Krieger NS, Asplin JR, Frick KK, Granja I, Culbertson CD, Ng A et al (2015) Effect of potassium citrate on calcium phosphate stones in a model of hypercalciuria. J Am Soc Nephrol JASN 26(12):3001–3008
Stern JM, Moazami S, Qiu Y, Kurland I, Chen Z, Agalliu I et al (2016) Evidence for a distinct gut microbiome in kidney stone formers compared to non-stone formers. Urolithiasis 44(5):399–407
Zhang D, Chen G, Manwani D, Mortha A, Xu C, Faith JJ et al (2015) Neutrophil ageing is regulated by the microbiome. Nature 525(7570):528–532
Ghartey JP, Smith BC, Chen Z, Buckley N, Lo Y, Ratner AJ et al (2014) Lactobacillus crispatus dominant vaginal microbiome is associated with inhibitory activity of female genital tract secretions against Escherichia coli. PLoS One 9(5):e96659
Smith BC, McAndrew T, Chen Z, Harari A, Barris DM, Viswanathan S et al (2012) The cervical microbiome over 7 years and a comparison of methodologies for its characterization. PLoS One 7(7):e40425
Smith BC, Zolnik CP, Usyk M, Chen Z, Kaiser K, Nucci-Sack A et al (2016) Distinct ecological niche of anal, oral, and cervical mucosal microbiomes in adolescent women. Yale J Biol Med 89(3):277–284
Kaplan RC, Wang Z, Usyk M, Sotres-Alvarez D, Daviglus ML, Schneiderman N, Talavera GA, Gellman MD, Thyagarajan B, Moon J-Y, Vasquez-Baeza Y, McDonald D, Williams-Nguyen JS, Wu MC, North KE, Shaffer J, Sollecito CC, Qi Q, Isasi CR, Wang T, Knight R, Burk RD (2019) Gut microbiome composition in the Hispanic Community Health Study/Study of Latinos is shaped by geographic relocation, environmental factors and obesity. Genome Biol 20:2019
Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet C, Al-Ghalith GA et al (2018) QIIME 2: reproducible, interactive, scalable, and extensible microbiome data science. PeerJ Preprints. Report No.: 2167-9843
Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJA, Holmes SP (2016) DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods 13(7):581
Reyes N, Montes O, Figueroa S, Tiwari R, Sollecito CC, Emmerich R et al (2020) Staphylococcus aureus nasal carriage and microbiome composition among medical students from Colombia: a cross-sectional study. F1000Research 9:78
Wang Q, Garrity GM, Tiedje JM, Cole JR (2007) Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol 73(16):5261–5267
Team RC (2015) R: a language and environment for statistical computing. R (Version 3.2) ed. R Foundation for Statistical Computing, Vienna
Wickham H (2016) ggplot2: elegant graphics for data analysis. Springer, Berlin
Oksanen J, Blanchet FG, Kindt R, Legendre P, O’hara R, Simpson GL et al (2010) Vegan: community ecology package. R package version 1.17-4. http://cranr-project org>Acessoem 23:2010
Morton JT, Marotz C, Washburne A, Silverman J, Zaramela LS, Edlund A et al (2019) Establishing microbial composition measurement standards with reference frames. Nat Commun 10(1):2719
Mandal S, Van Treuren W, White RA, Eggesbø M, Knight R, Peddada SD (2015) Analysis of composition of microbiomes: a novel method for studying microbial composition. Microb Ecol Health Dis 26(1):27663
Miller AW, Choy D, Penniston KL, Lange D (2019) Inhibition of urinary stone disease by a multi-species bacterial network ensures healthy oxalate homeostasis. Kidney Int 96(1):180–188
Tavasoli S, Alebouyeh M, Naji M, Shakiba Majd G, Shabani Nashtaei M, Broumandnia N et al (2020) Association of intestinal oxalate-degrading bacteria with recurrent calcium kidney stone formation and hyperoxaluria: a case-control study. BJU Int 125(1):133–143
Miller AW, Oakeson KF, Dale C, Dearing MD (2016) Microbial community transplant results in increased and long-term oxalate degradation. Microb Ecol 72(2):470–478
Millán Rodríguez F, Sabiote Rubio L, Girón Nanne I, Sánchez Martín F, Emiliani E, Angerri Feu O (2020) The relationship between calcium oxalate lithiasis and chronic proinflammatory intestinal dysbiosis pattern: a prospective study. Urolithiasis 48(4):321–328
Tang R, Jiang Y, Tan A, Ye J, Xian X, Xie Y et al (2018) 16S rRNA gene sequencing reveals altered composition of gut microbiota in individuals with kidney stones. Urolithiasis 46(6):503–514
Ito H, Miura N, Masai M, Yamamoto K, Hara T (1996) Reduction of oxalate content of foods by the oxalate degrading bacterium, Eubacterium lentum WYH-1. Int J Urol 3(1):31–34
Funding
David A. Bushinsky is supported by NIH (RO1 DK075462). Joshua M. Stern is supported by The Complications of Diabetes Consortium (DIACOMP) and the Mouse Microbiome Metabolic Research Program (MMRP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflicts or competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stern, J.M., Burk, R.D., Asplin, J. et al. Kidney stone formation and the gut microbiome are altered by antibiotics in genetic hypercalciuric stone-forming rats. Urolithiasis 49, 185–193 (2021). https://doi.org/10.1007/s00240-020-01223-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-020-01223-5