Abstract
Background
Glomus is uncommon benign tumours presenting as a form of chronic pain syndrome that is often disabling with resultant poor quality of life. The lack of an imaging protocol further impedes timely diagnosis, especially when presenting atypically. The objective of this study aims to reflect on the efficacy of imaging modalities based on strong clinical suspicion for glomus tumours.
Methods
This is an observational retrospective study recorded over a decade in 23 patients who presented with neuropathic pain and symptoms suspicious of glomus tumours to the outpatient departments of neurology and plastic surgery of a single hospital centre with quaternary level of health care.
Results
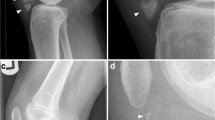
Twenty-two patients had presented with the classical symptoms of pain and pinpoint tenderness while 7 had temperature sensitivity. Imaging studies were done in 19 patients. There was preponderance of thumb followed by the middle finger with regard to presenting site, the mean age of the patient was close to 39 years and mean duration of presentation was approximately 3.5 years. A rare case of disuse atrophy associated with the presence of glomus tumour in the midsole of the left foot in one of our patients diagnosed solely through MRI of the foot is detailed as well in this study.
Conclusions
We emphasise on the need for a high index of clinical suspicion and vigilance aided by ultrasound and MRI when pain and disability are almost always disproportionate to the size of the affected area. Prompt diagnosis leads to early surgical excision providing relief.
Level of evidence
Level IV, Diagnostic









Similar content being viewed by others
Data availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
References
Boussakri H, Elibrahimi A, Hahem C et al (2016) Les tumeurs glomiques de la main: une étude rétrospective de 11 cas (Glomus tumors of the hand: a retrospective study of 11 cases). Pan Afr Med J 24:262
Masson P (1924) Le lomus neuromyoarteriel des regions tactiles et ses tumeurs. Lyon Chirurgical 21:257–80.x
Wood W (1812) On Painful Subcutaneous Tubercle. Edinb Med Surg J 8(31):283–291
Santoshi JA, Kori VK, Khurana U (2019) Glomus tumor of the fingertips: a frequently missed diagnosis. J Family Med Prim Care 8(3):904–908
Kumar S, Tiwary SK, More R, Kumar P, Khanna AK (2020) Digital glomus tumor: an experience of 57 cases over 20 years. J Family Med Prim Care 9(7):3514–3517
Bisceglia M, Bisceglia S, Ciampi C, Panniello G, Galliani C (2018) Glomus coccygeum: a review. Pathologica 110(4):287–293
Jing H, Weiwen C, Meihong C, Xiaohong G (2022) Glomus tumour of the iris: a case report. Eur J Ophthalmol 32(1):NP203–NP207
Novis E, Raman A, Maclean F, Lazzaro E (2018) Glomus tumour of the kidney: a case report and review of the literature. ANZ J Surg 88(6):653–654
Quah BL, Donofrio CA, La Rosa S et al (2021) Primary glomus tumour of the pituitary gland: diagnostic challenges of a rare and potentially aggressive neoplasm. Virchows Arch 478(5):977–984
Tullie STE, Quraishi MK, Karawita T, Anjarwalla S (2019) Rare presentation of a testicular glomus tumour. BMJ Case Rep 12(11):e230935
Idoudi S, Arousse A, Boussofara L (2019) Glomus tumor of the buttock. Dermatol Pract Concept 9(4):318–319
Chen IY, Fazili BG, Liao X (2020) Glomus tumor of the colon: a rare case report and review of literature. Int J Surg Pathol 28(6):691–695
Sasaki S, Takami Y, Wada Y et al (2020) Glomus tumor of the duodenum: a rare case report. Surg Case Rep 6(1):305
Tewattanarat N, Srinakarin J, Wongwiwatchai J et al (2020) Imaging of a glomus tumor of the liver in a child. Radiol Case Rep 15(4):311–315
Tamaki I, Hosoda Y, Sasano H et al (2020) Primary pancreatic glomus tumor invading into the superior mesenteric vein: a case report. Surg Case Rep 6(1):279
Lin J, Shen J, Yue H, Li Q, Cheng Y, Zhou M (2020) Gastric glomus tumor: a clinicopathologic and immunohistochemical study of 21 cases. Biomed Res Int 2020:5637893
Nakajima E, Takashi H, Taira O et al (2021) Glomus tumor in a segmental bronchus: a case report. Ann Thorac Cardiovasc Surg 27(6):407–409
Zhao SN, Jin Y, Xie HK, Wu CY, Li Y, Zhang LP (2020) Zhonghua Bing Li Xue Za Zhi 49(12):1282–1287
Sbai MA, Benzarti S, Gharbi W, Khoffi W, Maalla R (2018) Glomus tumor of the leg: a case report. Pan Afr Med J 31:186
Kunz EM, Ram B (2020) Atypical presentation of a glomus tumor in the rearfoot: a case report. J Am Podiatr Med Assoc 110(6). https://doi.org/10.7547/19-184
Glazebrook KN, Most MJ, Schiefer TK, Inwards CY, Sim FH (2010) Multiple glomus tumors of the lower leg. J Ultrasound Med 29(4):667–670
Hufschmidt K, Foissac R, Camuzard O, Cardot-Leccia N, Chignon-Sicard B, Balaguer T (2017) Glomus tumors of the upper limb: single-center retrospective study of clinical and functional outcomes. Hand Surg Rehabil 36(4):290–295
Grover C, Jayasree P, Kaliyadan F (2021) Clinical and onychoscopic characteristics of subungual glomus tumor: a cross-sectional study. Int J Dermatol 60(6):693–702
Akechi Y, Miura S, Ochi M et al (2021) Unilateral lower limb atrophy associated with glomus tumors: a case report. J Med Case Rep 15(1):8
Rodríguez JM, Idoate MA, Pardo-Mindán FJ (2003) The role of mast cells in glomus tumours: report of a case of an intramuscular glomus tumour with a prominent mastocytic component. Histopathology 42(3):307–308
Cooke SA (1971) Misleading features in the clinical diagnosis of the peripheral glomus tumour. Br J Surg 58(8):602–606
Kloping LP, Widhiyanto L, Irianto KA, Sindrawati O, Kloping YP (2020) Glomus tumor-induced lower extremity pain: a case report. Int J Surg Case Rep 75:352–356
Morey VM, Garg B, Kotwal PP (2016) Glomus tumours of the hand: review of literature. J Clin Orthop Trauma 7(4):286–291
Otsu A (1977) Glomus tumour and pain. Pain 3:88
Colorado B (2021) Sonographic imaging of an atypical glomus tumor. PM R 13(1):103–104
Funding
The authors declare that no financial support or funding of any kind was received for the preparation of this manuscript and its submission.
Author information
Authors and Affiliations
Contributions
The study was planned and drafted by Dr Sreevishnu Kalaga V P. Patients were consulted by Dr Pramod and Dr Uday Murgod and were reviewed and referred to the Department of Plastic Surgery. Dr Anantheswar Y N, Dr Ashok B C and Dr Srikant V operated on the patients and reviewed their follow-up in the outpatient services post-op with assistance from Dr Harish Kumar Kabilan. Data collection and compilation were done by Dr Sreevishnu Kalaga V P and Dr Harish Kumar Kabilan. Relevant statistical measures were performed by Dr Sreevishnu Kalaga V P. Radiological data and figure legends were provided by Dr Seema Janardhan and histopathological reports were given by Dr Susmita Rakshit H. The final draft was proofread by Dr Sreevishnu Kalaga V P and Dr Pramod Krishnan and reviewed by all authors before submission. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Patient consent
All patients have given informed consent for this study. All the patient’s details have been sufficiently anonymised.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Local Ethics Committee confirmed that approval was not required for this study.
Competing interests
Sreevishnu Kalaga V P, Pramod Krishnan, Uday Murgod, Anantheswar Y N, Ashok B C, Srikanth V, Harish Kumar Kabilan, Seema Janardhan and Susmita Rakshit H declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kalaga, S.V., Krishnan, P., Murgod, U. et al. Glomus tumour: a disabling but curable chronic pain syndrome—a retrospective observational study. Eur J Plast Surg 46, 1237–1246 (2023). https://doi.org/10.1007/s00238-023-02120-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02120-x