Abstract
Background
Emergence agitation (EA) is a common post-anesthesia condition that presents with restlessness, excitation, disorientation, and inconsolable crying. Gabapentin is a structural analog of gamma-aminobutyric acid, which is an anticonvulsant medication that also acts as an anti-hyperalgesic and anti-nociceptive drug. In the present study, we evaluated the effect of the single-dose preoperative administration of gabapentin (600 mg) on EA after rhinoplasty.
Methods
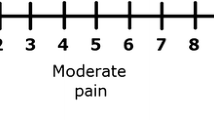
In this prospective, multicenter, double-blinded randomized controlled trial, we enrolled 120 rhinoplasty candidates from September 2019 to September 2020. Patients were randomly allocated into two groups to receive either gabapentin (600 mg) or a placebo before the operation. To assess postoperative pain, a numerical rating scale was used. Also, restlessness was evaluated based on a 7-point Riker Sedation-Agitation Scale extending from unarousable (point 1) to dangerous agitation (point 7). The patients with a median age of 31 years and a median weight of 65 kg were divided and matched based on age and weight between the two groups (receiving a single dose of gabapentin) and controls (receiving placebo).
Results
The gabapentin group demonstrated a significantly lower restlessness score, both during extubation and after recovery compared to the control group (P =0.001 and 0.001). Regarding postoperative pain, nausea, and dizziness, although these values were lower in the intervention group, there was no statistically significant difference between the two groups (P=0.462, 0.494, and 0.163, respectively).
Conclusions
Preoperative oral administration of gabapentin (600 mg) significantly reduced restlessness during recovery and extubation.
Level of evidence
Level I, therapeutic study


Similar content being viewed by others
Abbreviations
- EA:
-
emergence agitation
- GABA:
-
gamma-aminobutyric acid
- ASA:
-
American Society of Anesthesiologists
- RSAS:
-
Riker Sedation-Agitation Scale
- NRS:
-
numerical rating scale
- GCP:
-
good clinical practice
References
Demir CY, Yuzkat N (2018) Prevention of emergence agitation with ketamine in rhinoplasty. Aesthetic Plast Surg 42(3):847–853
Vlajkovic GP, Sindjelic RP (2007) Emergence delirium in children: many questions, few answers. Anesth Analg 104(1):84–91
Singh R, Kharbanda M, Sood N, Mahajan V, Chatterji C (2012) Comparative evaluation of incidence of emergence agitation and post-operative recovery profile in paediatric patients after isoflurane, sevoflurane and desflurane anaesthesia. Indian J Anaesth 56(2):156–161
Badawy AA, Kasem SA, Rashwan D, Al Menesy T, Adel G, Mokhtar AM et al (2018) The role of gabapentin oral solution in decreasing desflurane associated emergence agitation and delirium in children after stabismus surgery, a prospective randomized double-blind study. BMC Anesthesiol 18(1):73
Huang H-W, Yan L-M, Yang Y-L, He X, Sun X-M, Wang Y-M et al (2018) Bi-frontal pneumocephalus is an independent risk factor for early postoperative agitation in adult patients admitted to intensive care unit after elective craniotomy for brain tumor: a prospective cohort study. PLoS One. 13:e0201064
Lepousé C, Lautner CA, Liu L, Gomis P, Leon A (2006) Emergence delirium in adults in the post-anaesthesia care unit. Br J Anaesth 96(6):747–753
Anghelescu DL, Rakes LC, Shearer JR, Bikhazi GB (2011) Prevention of emergence agitation in seven children receiving low-dose ketamine and propofol total intravenous anesthesia. AANA J 79(3):238–242
Sato M, Shirakami G, Tazuke-Nishimura M, Matsuura S, Tanimoto K, Fukuda K (2010) Effect of single-dose dexmedetomidine on emergence agitation and recovery profiles after sevoflurane anesthesia in pediatric ambulatory surgery. J Anesth 24(5):675–682
Kwak KH (2010) Emergence agitation/delirium: we still don’t know. Korean J Anesthesiol 59(2):73–74
Kawai M, Kurata S, Sanuki T, Mishima G, Kiriishi K, Watanabe T et al (2019) The effect of midazolam administration for the prevention of emergence agitation in pediatric patients with extreme fear and non-cooperation undergoing dental treatment under sevoflurane anesthesia, a double-blind, randomized study. Drug Des Devel Ther 13:1729–1737
Kim D, Doo AR, Lim H, Son JS, Lee JR, Han YJ et al (2013) Effect of ketorolac on the prevention of emergence agitation in children after sevoflurane anesthesia. Korean J Anesthesiol 64(3):240–245
Funk W, Hollnberger H, Geroldinger J (2008) Physostigmine and anaesthesia emergence delirium in preschool children: a randomized blinded trial. Eur J Anaesthesiol 25(1):37–42
Kim KM, Lee KH, Kim YH, Ko MJ, Jung J-W, Kang E (2016) Comparison of effects of intravenous midazolam and ketamine on emergence agitation in children: randomized controlled trial. J Int Med Res 44(2):258–266
Sanders JG, Dawes PJ (2016) Gabapentin for perioperative analgesia in otorhinolaryngology-head and neck surgery: systematic review. Otolaryngol Head Neck Surg 155(6):893–903
Salama ER, Amer AF (2018) The effect of pre-emptive gabapentin on anaesthetic and analgesic requirements in patients undergoing rhinoplasty: a prospective randomised study. Indian J Anaesth 62(3):197–201
Menda F, Köner O, Sayın M, Ergenoğlu M, Küçükaksu S, Aykaç B (2010) Effects of single-dose gabapentin on postoperative pain and morphine consumption after cardiac surgery. J Cardiothorac Vasc Anesth 24(5):808–813
Hassani V, Pazouki A, Nikoubakht N, Chaichian S, Sayarifard A, Shakib KA (2015) The effect of gabapentin on reducing pain after laparoscopic gastric bypass surgery in patients with morbid obesity: a randomized clinical trial. Anesth. Pain Med 5(1):e22372-e
Turan A, Karamanlioğlu B, Memiş D, Hamamcioglu MK, Tükenmez B, Pamukçu Z et al (2004) Analgesic effects of gabapentin after spinal surgery. Anesthesiology 100(4):935–938
Öztürk G (2021) Prevention of nasal deviation related to preservation rhinoplasty in non-deviated noses using suturing approaches. Aesthetic Plast Surg 45(4):1693–1702. https://doi.org/10.1007/s00266-020-02105-2
Pan Y, Cai W, Cheng Q, Dong W, An T, Yan J (2015) Association between anxiety and hypertension: a systematic review and meta-analysis of epidemiological studies. Neuropsychiatr Dis Treat 11:1121
Liu M-Y, Li N, Li WA, Khan H (2017) Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res 39(6):573–580
Johnson HM (2019) Anxiety and hypertension: is there a link? A literature review of the comorbidity relationship between anxiety and hypertension. Curr Hypertens Rep 21(9):1–7
Riker RR, Fraser GL, Simmons LE, Wilkins ML (2001) Validating the sedation-agitation scale with the bispectral index and visual analog scale in adult ICU patients after cardiac surgery. Intensive Care Med 27(5):853–858
World Medical Association Declaration of Helsinki (2013) ethical principles for medical research involving human subjects. JAMA. 310(20):2191–4. https://doi.org/10.1001/jama.2013.281053
Salman AE, Camkıran A, Oğuz S, Dönmez A (2013) Gabapentin premedication for postoperative analgesia and emergence agitation after sevoflurane anesthesia in pediatric patients. Agri 25(4):163–168
Kim H-J, Kim D-K, Kim H-Y, Kim J-K, Choi S-W (2015) Risk factors of emergence agitation in adults undergoing general anesthesia for nasal surgery. Clin Exp Otorhinolaryngol 8(1):46–51
Azemati S, Gholami Dokouhaki A, Talei A, Khademi S, Moin-Vaziri N (2013) Evaluation of the effect of a preoperative single dose of gabapentin on emergence agitation in patients undergoing breast cancer surgery. Middle East J Cancer 4(4):145–151
Sen H, Sizlan A, Yanarates O, Emirkadi H, Ozkan S, Dagli G et al (2009) A comparison of gabapentin and ketamine in acute and chronic pain after hysterectomy. Anesth Analg 109(5):1645–50. https://doi.org/10.1213/ANE.0b013e3181b65ea0
Pourfakhr P, Khajavi MR, Jalali A, Memari F, Etezadi F, Momeni Roochi M et al (2019) Low-dose preoperative pregabalin improves postoperative pain management in septorhinoplasty surgery: a double-blind randomized clinical trial. Eur Arch Oto-Rhino-Laryngol 276(8):2243–2249
Mathiesen O, Møiniche S, Dahl JB (2007) Gabapentin and postoperative pain: a qualitative and quantitative systematic review, with focus on procedure. BMC Anesthesiol 7(1):6
Park IJ, Kim G, Ko G, Lee YJ, Hwang SH (2016) Does preoperative administration of gabapentin/pregabalin improve postoperative nasal surgery pain? Laryngoscope 126(10):2232–2241
Hu J, Huang D, Li M, Wu C, Zhang J (2018) Effects of a single dose of preoperative pregabalin and gabapentin for acute postoperative pain: a network meta-analysis of randomized controlled trials. J Pain Res 11:2633–2643
VanMeter SA, Kavanagh ST, Warren S, Barrett RW (2012) Dose response of gabapentin enacarbil versus placebo in subjects with moderate-to-severe primary restless legs syndrome: an integrated analysis of three 12-week studies. CNS Drugs 26(9):773–780
Grant MC, Lee H, Page AJ, Hobson D, Wick E, Wu CL (2016) The effect of preoperative gabapentin on postoperative nausea and vomiting: a meta-analysis. Anesth Analg 122(4):976–985
Acknowledgements
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran, and also the Center for Development of Clinical Research of Nemazee Hospital and Dr. Nasrin Shokrpour for editorial assistance.
Funding
No specific funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Study design: M.A.H.; data acquisition: H.H, R.J, A.A.; data analysis: R.S, M.A.H.; data interpretation: M.A.H, H.H, K.R, A.A.; manuscript preparation: H.K, R.S, K.R, M.A.H, H.H.; manuscript revision: all authors. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics committee of Shiraz University of Medical Sciences (IR.SUMS.MED.REC.1398.395), the Institutional Review Board, and the Iranian Registry of Clinical Trials (IRCT20200907048652N2) on 2/1/2021. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Consent to participate
Informed consent was obtained from all patients or their legally authorized representatives for being included in the study.
Consent for publication
Informed consent was obtained from all patients or their legally authorized representatives for the publication of the study.
Competing interests
Mohammad Ali Hoghoughi, Reza Jouybar, Akbar Alvandi, Reza Shahriarirad, Hamidreza Hosseinpour, Keivan Ranjbar, and Hooman Kamran declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hoghoughi, M.A., Jouybar, R., Alvandi, A. et al. The effect of a preoperative single dose of gabapentin on emergence agitation in patients undergoing rhinoplasty: a randomized clinical trial. Eur J Plast Surg 46, 1019–1025 (2023). https://doi.org/10.1007/s00238-023-02116-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02116-7