Abstract
Background
Today, the surgical approach in the treatment of complex injuries is changing in that complex and intricate procedures, such as microvascular surgery, are no longer kept as a last resort. In Plastic and Reconstructive surgery, microvascular surgery has been described in the treatment of extensive tissue defects using free tissue transfer. This study discusses the incorporation of microvascular training in residency programs, as well as identifying the factors that influence residents’ confidence in performing microsurgery without supervision.
Methods
This is a cross-sectional study conducted on thirteen current and former Plastic and Reconstructive surgery residents who practiced microsurgery during the past 8 years at the American University of Beirut Medical Center in Lebanon.
Results
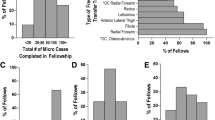
Nine residents (69.2%) started scrubbing in and became actively involved in microsurgery procedures at the PGY IV level with the majority being exposed to cases every 2–3 weeks (69.2%). Residents were mostly exposed to breast (100%) and orthopedic reconstruction (92.3%), and facial trauma reconstruction was the least practiced (46.2%). Eleven residents (84.6%) reported that music and choice of OR staff assisting in the operation significantly affected their speed and performance. Eleven residents (84.6%) were satisfied with the training program, and ten found the training program beneficial for their career (76.9%).
Conclusion
Our findings suggest that residents who had a higher workload and were actively involved in microsurgery early during residency felt more confident in performing the procedure by themselves. The choice of operating staff, playing music, and the presence of different attendings in the operating room were found to affect the speed and performance of residents.
Level of evidence
Level V, Risk/Prognostic.


Similar content being viewed by others
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Mavrogenis AF, Markatos K, Saranteas T, Ignatiadis I, Spyridonos S, Bumbasirevic M, Georgescu AV, Beris A, Soucacos PN (2019) The history of microsurgery. Eur J Orthop Surg Traumatol 29(2):247–254
Nangole WF, Khainga S, Aswani J, Kahoro L, Vilembwa A (2015) Free flaps in a resource constrained environment: a five-year experience-outcomes and lessons learned. Plast Surg Int 2015:194174
Turrà F, Padula SL, Razzano S et al (2013) Microvascular free-flap transfer for head and neck reconstruction in elderly patients. BMC Surg 13(Suppl 2):S27
Kim HS, Chung CH, Chang YJ (2020) Free-flap reconstruction in recurrent head and neck cancer: a retrospective review of 124 cases. Arch Craniofac Surg 21(1):27–34
Girish Rao S, Aditya TN, Gopinath KS, Anand K (2009) Free fibula flap in the reconstruction of mandible: a report of six cases. J Maxillofac Oral Surg 8(3):275–278
Rose J, Puckett Y (2022) Breast reconstruction free flaps. In: StatPearls, Treasure Island (FL)
Koulaxouzidis G, Schlagnitweit P, Anderl C, Braig D, Märdian S (2022) Microsurgical reconstruction in orthopedic tumor resections as part of a multidisciplinary surgical approach for sarcomas of the extremities. Life 12(11):1801
Park JW, Moon J, Lee KT, Woo KJ, Oh H, Jeon BJ, Lim SY, Pyon JK, Mun GH (2020) Comparison of surgical outcomes of free flap reconstructions performed by expert microsurgeons and trainees who completed a structured microsurgical training program in a teaching hospital. J Plast Reconstr Aesthet Surg 73(10):1834–1844
Banda CH, Georgios P, Narushima M, Ishiura R, Fujita M, Goran J (2019) Challenges in global reconstructive microsurgery: the sub-Saharan African surgeons’ perspective. JPRAS Open 20:19–26
Ruan QZ, Ricci JA, Silvestre J, Ho OA, Ganor O, Lee BT (2017) Academic productivity of faculty associated with craniofacial surgery fellowship programs. J Craniofac Surg 28(8):1988–1992
Hassan B, Abou Koura A, Makarem A, Abi Mosleh K, Dimassi H, Tamim H, Ibrahim A (2023) Predictors of surgical site infection following reconstructive flap surgery: a multi-institutional analysis of 37,177 patients. Front Surg 10:1080143
Irawati N, Every J, Dawson R, Leinkram D, Elliott M, Ch’ng S, Low H, Palme CE, Clark J, Wykes J (2023) Effect of operative time on complications associated with free flap reconstruction of the head and neck. Clin Otolaryngol 48(2):175–181
Luginbuhl A, Pribitkin E, Krein H, Heffelfinger R (2010) Assessment of microvascular anastomosis training in otolaryngology residencies: survey of United States program directors. Otolaryngology 143:633–636
Bennion DM, Dziegielewski PT, Boyce BJ, Ducic Y, Sawhney R (2019) Fellowship training in microvascular surgery and post-fellowship practice patterns: a cross sectional survey of microvascular surgeons from facial plastic and reconstructive surgery programs. J Otolaryngol Head Neck Surg 48(1):19
Selber JC, Chang EI, Liu J, Suami H, Adelman DM, Garvey P, Hanasono MM, Butler CE (2012) Tracking the learning curve in microsurgical skill acquisition. Plast Reconstr Surg 130(4):550e–557e
Kania K, Chang DK, Abu-Ghname A, Reece EM, Chu CK, Maricevich M, Buchanan EP, Winocour S (2020) Microsurgery training in plastic surgery. Plast Reconstr Surg Glob Open 8(7):e2898
Shakir A, Chattopadhyay A, Paek LS, McGoldrick RB, Chetta MD, Hui K, Lee GK (2017) The effects of music on microsurgical technique and performance: a motion analysis study. Ann Plast Surg 78(5 Suppl 4):S243–S247
Oomens P, Fu VX, Kleinrensink GJ, Jeekel J (2019) The effect of music on simulated surgical performance: a systematic review. Surg Endosc 33(9):2774–2784
Han Y, Zheng B, Zhao L et al (2022) Impact of background music on the performance of laparoscopy teams. BMC Med Educ 22:439
Belykh E, Onaka NR, Abramov IT, Yağmurlu K, Byvaltsev VA, Spetzler RF, Nakaj P, Preul MC (2018) Systematic review of factors influencing surgical performance: practical recommendations for microsurgical procedures in neurosurgery. World Neurosurg 112:e182–e207
Piromchai P, Avery A, Laopaiboon M, Kennedy G, O’Leary S (2015) Virtual reality training for improving the skills needed for performing surgery of the ear, nose or throat. Cochrane Database Syst Rev 2015(9):CD010198
Nagendran M, Gurusamy KS, Aggarwal R, Loizidou M, Davidson BR (2013) Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2013(8):CD006575
Ulbrich M, Van den Bosch V, Bönsch A, Gruber LJ, Ooms M, Melchior C, Motmaen I, Wilpert C, Rashad A, Kuhlen TW, Hölzle F, Puladi B (2023 Jan) Advantages of a training course for surgical planning in virtual reality for oral and maxillofacial surgery: crossover study. JMIR Serious Games 19(11):e40541
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by first, second, and third authors. The first draft of the manuscript was written by first and second authors, and all authors commented on previous versions of the manuscript. The corresponding author supervised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This project was approved by the American University of Beirut Institutional Review Board (SBS-2021-0105). This paper is not currently being considered for publication elsewhere. It reflects the authors’ own research and analysis in a truthful and complete manner. All authors have been personally and actively involved in substantial work leading to the paper and will take public responsibility for its content.
Consent to participate
An online consent form was sent explaining the purpose of the study and confidentiality followed by a link that redirects participants to the survey.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hajjar, M.S., Koura, A.A., Zerdan, M.B. et al. Microvascular surgery training in a low volume setting: a single healthcare center experience. Eur J Plast Surg 46, 1377–1382 (2023). https://doi.org/10.1007/s00238-023-02111-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02111-y