Abstract
Background
Current literature demonstrates that factors contributing to prolonged drain duration in the subpectoral implant-based and autologous populations include older age, higher body mass index (BMI), history of neoadjuvant chemotherapy, textured tissue expanders, large volumes of initial tissue expander inflation, use of acellular dermal matrix, hypertension, and reoperation. We aim to examine factors contributing to prolonged drain duration in the prepectoral staged implant-based breast reconstruction population.
Methods
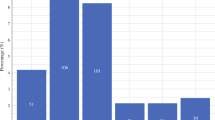
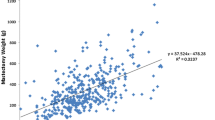
This was a retrospective investigation of 336 patients who underwent prepectoral staged implant-based breast reconstruction between 2018 and 2021 at a single institution. Prolonged drain duration was defined as patients whose drain duration period was at the 75th percentile or above. Patient demographics, comorbidities, medical histories, perioperative variables, and complication rates were recorded. Chi-square and multivariable regression tests were performed to evaluate variables that would impact prolonged drain duration and post-operative complications.
Results
Of 336 patients (mean age 49.30 ± 10.73), 88 experienced prolonged drain duration (18 days). Higher BMI (obese category) (p = 0.003) was the only significant predictor of prolonged drain duration.
Conclusions
In patients undergoing prepectoral staged implant-based reconstruction, BMI above the obese threshold increases the risk of prolonged drain duration. In contrast to prior studies performed in autologous reconstruction and subpectoral reconstruction, other demographic and perioperative factors were not significant predictors of prolonged drain. Given the increasing prevalence and preference for prepectoral breast reconstruction, this study can be used to guide postoperative management concerning drain removal and follow-up parameters.
Level of evidence: Level III, Risk/Prognostic
Similar content being viewed by others
References
Albornoz CR, Bach PB, Mehrara BJ et al (2013) A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 131(1):15–23. https://doi.org/10.1097/PRS.0b013e3182729cde
Walia GS, Aston J, Bello R et al (2018) Prepectoral versus subpectoral tissue expander placement: a clinical and quality of life outcomes study. Plast Reconstr Surg Glob Open 6(4):e1731. https://doi.org/10.1097/GOX.0000000000001731. (Published 2018 Apr 20)
Yang JY, Kim CW, Lee JW, Kim SK, Lee SA, Hwang E (2019) Considerations for patient selection: prepectoral versus subpectoral implant-based breast reconstruction. Arch Plast Surg 46(6):550–557. https://doi.org/10.5999/aps.2019.00353
Murray JD, Elwood ET, Jones GE, Barrick R, Feng J (2009) Decreasing expander breast infection: a new drain care protocol. Can J Plast Surg 17(1):17–21
Xue DQ, Qian C, Yang L, Wang XF (2012) Risk factors for surgical site infections after breast surgery: a systematic review and meta-analysis. Eur J Surg Oncol 38(5):375–381. https://doi.org/10.1016/j.ejso.2012.02.179
Lee KT, Hong SH, Jeon BJ, Pyon JK, Mun GH, Bang SI (2019) Predictors for prolonged drainage following tissue expander-based breast reconstruction. Plast Reconstr Surg 144(1):9e–17e. https://doi.org/10.1097/PRS.0000000000005697
Edwards BL, Stukenborg GJ, Brenin DR, Schroen AT (2014) Use of prophylactic postoperative antibiotics during surgical drain presence following mastectomy. Ann Surg Oncol 21(10):3249–3255. https://doi.org/10.1245/s10434-014-3960-7
Chen CF, Lin SF, Hung CF, Chou P (2016) Risk of infection is associated more with drain duration than daily drainage volume in prosthesis-based breast reconstruction: a cohort study. Medicine (Baltimore) 95(49):e5605. https://doi.org/10.1097/MD.0000000000005605
Dinis J, Allam O, Junn A, et al (2021) Predictors for prolonged drain use following autologous breast reconstruction [published online ahead of print, 2021 Jul 20]. J Reconstr Microsurg. https://doi.org/10.1055/s-0041-1731765
Felippe WA, Werneck GL, Santoro-Lopes G (2007) Surgical site infection among women discharged with a drain in situ after breast cancer surgery. World J Surg 31(12):2293–2301. https://doi.org/10.1007/s00268-007-9248-3
Brahmbhatt RD, Huebner M, Scow JS et al (2012) National practice patterns in preoperative and postoperative antibiotic prophylaxis in breast procedures requiring drains: survey of the American Society of Breast Surgeons. Ann Surg Oncol 19(10):3205–3211. https://doi.org/10.1245/s10434-012-2477-1
Khansa I, Hendrick RG Jr, Shore A, Meyerson J, Yang M, Boehmler JH IV (2014) Breast reconstruction with tissue expanders: implementation of a standardized best-practices protocol to reduce infection rates. Plast Reconstr Surg 134:11–18
Phillips BT, Wang ED, Mirrer J et al (2011) Current practice among plastic surgeons of antibiotic prophylaxis and closed- suction drains in breast reconstruction: experience, evi- dence, and implications for postoperative care. Ann Plast Surg 66:460–465
Antoniak K, Hansdorfer-Korzon R, Mrugacz M, Zorena K (2021) Adipose tissue and biological factors. Possible Link between Lymphatic System Dysfunction and Obesity. Metabolites 11(9):617. https://doi.org/10.3390/metabo11090617. (Published 2021 Sep 11)
García Nores GD, Cuzzone DA, Albano NJ et al (2016) Obesity but not high-fat diet impairs lymphatic function. Int J Obes (Lond) 40(10):1582–1590. https://doi.org/10.1038/ijo.2016.96
Stapleton PA, James ME, Goodwill AG, Frisbee JC (2008) Obesity and vascular dysfunction. Pathophysiology 15(2):79–89. https://doi.org/10.1016/j.pathophys.2008.04.007
Haddock N, Levine J (2010) Breast reconstruction with implants, tissue expanders and AlloDerm: predicting volume and maximizing the skin envelope in skin sparing mastectomies. Breast J 16(1):14–19. https://doi.org/10.1111/j.1524-4741.2009.00866.x
Suga H, Shiraishi T, Shibasaki Y, Takushima A, Harii K (2016) Predictive factors for drainage volume after expander-based breast reconstruction. Plast Reconstr Surg Global Open 4(6):e727. https://doi.org/10.1097/GOX.0000000000000752
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This is a retrospective observational study. The Stanford University Research Ethics Committee has confirmed that no ethical approval is required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Patient consent
Patients signed informed consent regarding publishing their data and photographs. To add, no identifying patient data was used as all data extracted were blinded.
Conflict of interest
Kometh Thawanyarat, Jennifer K. Shah, Gina Eggert, Mallory Rowley, Trudy Kim, Pooja S. Yesantharao, Elizabeth Turner, Brian Thornton and Rahim Nazerali declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thawanyarat, K., Shah, J.K., Eggert, G. et al. Factors contributing to prolonged drain duration in prepectoral staged implant-based breast reconstruction. Eur J Plast Surg 46, 1121–1127 (2023). https://doi.org/10.1007/s00238-023-02092-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02092-y