Abstract
Background
With the recent safety communication issued by The Food and Drug Administration, squamous cell carcinoma breast-implant associated (BIA-SCC) has become part of the breast implant capsule related conditions. In the present paper, we review all cases of BIA-SCC currently reported in the literature.
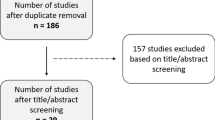
Methods
From October 2022 to February 2023, we conducted a systematic review of the literature in accordance with the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) statement. An electronic search was performed using PubMed/Medline, Scopus, and Cochrane Database. Only manuscripts written in English and featuring one or more clinical cases of BIA-SCC were included for full-text analysis.
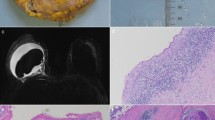
Results
Eight-hundred-sixty-seven articles were identified. After excluding duplicates, irrelevant and non-English-written papers, fifteen articles were deemed eligible for the review, featuring a total of eighteen cases. Eleven patients received bilateral breast augmentation, five bilateral or unilateral reconstruction either following mastectomy or for Poland syndrome, while in two cases the indication for implant placement was not reported. Time from implantation to clinical onset was less than ten years in three patients, over ten years in thirteen instances and not reported in two. History of capsular contracture was identified in eight patients, while complications including previous surgical revisions, implant exchange or exposure, extrusion or infection were reported in eight cases.
Conclusions
The paucity of literature on BIA-SCC still hinders us from drawing definitive conclusions. Nevertheless, we can infer that early detection of symptoms is pivotal in the decision-making process for the treatment and management of this nosological entity.
Level of evidence: Not gradable



Similar content being viewed by others
References
ASPS statement on Breast Implant Associated- Squamous Cell Carcinoma (BIA-SCC) (n.d.). https://www.plasticsurgery.org/for-medical-professionals/publications/psn-extra/news/asps-statement-on-breast-implant-associated-squamous-cell-carcinoma. Accessed 29 Nov 2022
Center for Devices and Radiological Health. Breast implants: Reports of cancers in capsule around implants. U.S. Food and Drug Administration (n.d.) https://www.fda.gov/medical-devices/safety-communications/breast-implants-reports-squamous-cell-carcinoma-and-various-lymphomas-capsule-around-implants-fda. Accessed 29 Nov 2022
Keech JA Jr, Creech BJ (1997) Anaplastic T-cell lymphoma in proximity to a saline-filled breast implant. Plast Reconstr Surg 100(2):554–555. https://doi.org/10.1097/00006534-199708000-00065
Swerdlow SH, Campo E, Pileri SA et al (2016) The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127(20):2375–2390. https://doi.org/10.1182/blood-2016-01-643569
Santanelli di Pompeo F, Sorotos M, Clemens MW et al (2022) Mortality Rate in Breast Implant Surgery: Is an Additional Procedure Worthwhile to Mitigate BIA-ALCL Risk? [published online ahead of print, 2022 Nov 14]. Aesthetic Plast Surg. https://doi.org/10.1007/s00266-022-03138-5
Di Pompeo FS, Panagiotakos D, Firmani G, Sorotos M (2022) BIA-ALCL Epidemiological Findings From a Retrospective Study of 248 Cases Extracted from Relevant Case Reports and Series: A Systematic Review [published online ahead of print, 2022 Nov 29] [published correction appears in Aesthet Surg J. 2023 Feb 22;:]. Aesthet Surg J. https://doi.org/10.1093/asj/sjac312
Vorstenbosch J, Chu JJ, Ariyan CE, McCarthy CM, Disa JJ, Nelson JA (2023) Clinical Implications and Management of Non-BIA-ALCL Breast Implant Capsular Pathology. Plast Reconstr Surg 151(1):20e–30e. https://doi.org/10.1097/PRS.0000000000009780
Paletta C, Paletta FX Jr, Paletta FX Sr (1992) Squamous cell carcinoma following breast augmentation. Ann Plast Surg 29(5):425–432. https://doi.org/10.1097/00000637-199211000-00009
Smahel J, Clodius L (1978) Epidermal lining in the capsule of a breast prosthesis. Br J Plast Surg 31(2):173–175
Smahel J, Clodius L (1993) Re: Squamous cell carcinoma following breast augmentation. Ann Plast Surg 30(6):569
Smahel J (1977) The healing of skin grafts. Clin Plast Surg 4(3):409–424
Kitchen SB, Paletta CE, Shehadi SI, Bauer WC (1994) Epithelialization of the lining of a breast implant capsule. Possible origins of squamous cell carcinoma associated with a breast implant capsule. Cancer 73(5):1449–1452. https://doi.org/10.1002/1097-0142(19940301)73:5%3c1449::aid-cncr2820730520%3e3.0.co;2-j
Clemens MW, Jacobsen ED, Horwitz SM (2019) NCCN Consensus Guidelines on the Diagnosis and Treatment of Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). Aesthet Surg J 39(Suppl_1):S3–S13. https://doi.org/10.1093/asj/sjy331
Satgunaseelan L, Cheung D, Reddy J (2015) Breast Implant-Associated Squamous Cell Carcinoma – A Rare Long Term Complication. Pathology 47(1):S72–S73
Olsen DL, Keeney GL, Chen B, Visscher DW, Carter JM (2017) Breast implant capsule-associated squamous cell carcinoma: a report of 2 cases. Hum Pathol 67:94–100. https://doi.org/10.1016/j.humpath.2017.07.011
Buchanan PJ, Chopra VK, Walker KL, Rudolph R, Greco RJ (2018) Primary Squamous Cell Carcinoma Arising From a Breast Implant Capsule: A Case Report and Review of the Literature. Aesthet Surg J 38(7). https://doi.org/10.1093/asj/sjy092
Goel P, Gould DJ, Kim AW et al (2019) Squamous cell carcinoma following multiple revision breast surgeries with massive chest wall reconstruction via flow-through double ALT free flaps. Eur J Plast Surg 42:517–522. https://doi.org/10.1007/s00238-019-01525-x
Goldberg MT, Llaneras J, Willson TD et al (2021) Squamous Cell Carcinoma Arising in Breast Implant Capsules. Ann Plast Surg 86(3):268–272. https://doi.org/10.1097/SAP.0000000000002524
Liu Z, Liu C, Chengglong Z, Yu Q, Zhang G, Wang X, Yu Z (2021) Breast prosthetic implant-associated Squamous Cell Carcinoma: A case report and Literature Review. Res Square. https://doi.org/10.21203/rs.3.rs-141167/v1
Whaley RD, Aldrees R, Dougherty RE, Prieto Granada C, Badve SS, Al DS (2022) Breast Implant Capsule-Associated Squamous Cell Carcinoma: Report of 2 Patients. Int J Surg Pathol 30(8):900–907. https://doi.org/10.1177/10668969221086940
Xia Z, Han B, Wang L et al (2023) Breast implant-associated squamous cell carcinoma in a male patient: A case report and review of the medical literature. Front Surg 9:983611. https://doi.org/10.3389/fsurg.2022.983611. (Published 2023 Jan 10)
Zomerlei TA, Samarghandi A, Terando AM (2016) Primary Squamous Cell Carcinoma Arising from a Breast Implant Capsule. Plast Reconstr Surg Glob Open 3(12):e586. https://doi.org/10.1097/GOX.0000000000000567. (Published 2016 Jan 7)
Zhou YM, Chaudhry HE, Shah A, Andrews J (2018) Breast Squamous Cell Carcinoma Following Breast Augmentation. Cureus 10(10):e3405. https://doi.org/10.7759/cureus.3405. (Published 2018 Oct 3)
Alfaro L, Roca M, Jimenez A, Vazquez C (2019) Breast implantassociated squamous cell carcinoma. Virchows Arch 475:S64–S64
Soni SE, Laun JC, Beard AS, Kuykendall LV (2022) Breast Implant Capsule-Associated Squamous Cell Carcinoma during Pregnancy: A Mimicker of Breast Implant-Associated Anaplastic Large-Cell Lymphoma. Plast Reconstr Surg 150(4):926e–928e. https://doi.org/10.1097/PRS.0000000000009506
Klopfleisch R, Jung F (2017) The pathology of the foreign body reaction against biomaterials. J Biomed Mater Res A 105(3):927–940. https://doi.org/10.1002/jbm.a.35958
Barr LH, Menard JW (1983) Marjolin’s ulcer. The LSU experience. Cancer 52(1):173–175. https://doi.org/10.1002/1097-0142(19830701)52:1%3c173::aid-cncr2820520131%3e3.0.co;2-6
Alikhan MB, Nassar A, Mansoor I (2010) Squamous metaplasia on the breast implant capsule. Int J Surg Pathol 18(6):570–574. https://doi.org/10.1177/1066896908329587
Yoo H, Park JU, Chang H (2022) Comprehensive Evaluation of the Current Knowledge on Breast Implant Associated-Anaplastic Large Cell Lymphoma. Arch Plast Surg 49(2):141–149. https://doi.org/10.1055/s-0042-1744422
Hu H, Jacombs A, Vickery K, Merten SL, Pennington DG, Deva AK (2015) Chronic biofilm infection in breast implants is associated with an increased T-cell lymphocytic infiltrate: implications for breast implant-associated lymphoma. Plast Reconstr Surg 135(2):319–329. https://doi.org/10.1097/PRS.0000000000000886
De Jong WH, Panagiotakos D, Proykova A et al (2021) Final opinion on the safety of breast implants in relation to anaplastic large cell lymphoma: Report of the scientific committee on health, emerging and environmental risks (SCHEER). Regul Toxicol Pharmacol 125:104982. https://doi.org/10.1016/j.yrtph.2021.104982
Santanelli di Pompeo F, Clemens MW, Atlan M et al (2022) Practice Recommendation Updates From the World Consensus Conference on BIA-ALCL. Aesthet Surg J 42(11):1262–1278. https://doi.org/10.1093/asj/sjac133
Di Pompeo FS, Panagiotakos D, Firmani G, Sorotos M (2022) BIA-ALCL Epidemiological Findings From a Retrospective Study of 248 Cases Extracted from Relevant Case Reports and Series: A Systematic Review [published online ahead of print, 2022 Nov 29] [published correction appears in Aesthet Surg J. 2023 Feb 22;:]. Aesthet Surg J sjac312. https://doi.org/10.1093/asj/sjac312
Morgenstern L, Gleischman SH, Michel SL, Rosenberg JE, Knight I, Goodman D (1985) Relation of free silicone to human breast carcinoma. Arch Surg 120(5):573–577. https://doi.org/10.1001/archsurg.1985.01390290051008
James SJ, Pogribna M, Miller BJ, Bolon B, Muskhelishvili L (1997) Characterization of cellular response to silicone implants in rats: implications for foreign-body carcinogenesis. Biomaterials 18(9):667–675. https://doi.org/10.1016/s0142-9612(96)00189-5
Cordon-Cardo C, Prives C (1999) At the crossroads of inflammation and tumorigenesis. J Exp Med 190(10):1367–1370. https://doi.org/10.1084/jem.190.10.1367
Hudson JD, Shoaibi MA, Maestro R, Carnero A, Hannon GJ, Beach DH (1999) A proinflammatory cytokine inhibits p53 tumor suppressor activity. J Exp Med 190(10):1375–1382. https://doi.org/10.1084/jem.190.10.1375
Cuomo R (2021) The State of the Art about Etiopathogenetic Models on Breast Implant Associated-Anaplastic Large Cell Lymphoma (BIA-ALCL): A Narrative Review. J Clin Med 10(10):2082. https://doi.org/10.3390/jcm10102082. (Published 2021 May 12)
Medical Device Reports of Breast Implant-Associated Anaplastic Large Cell Lymphoma (n.d.). https://www.fda.gov/medical-devices/breast-implants/medical-device-reports-breast-implant-associated-anaplastic-large-cell-lymphoma. Accessed 29 Nov 2022
Ogita M, Shiraishi K, Karasawa K et al (2020) Clinical outcome of adjuvant radiotherapy for squamous cell carcinoma of the breast; a multicenter retrospective cohort study. Breast 52:88–94. https://doi.org/10.1016/j.breast.2020.05.003
Jewell ML, Walden JL, Fontbona M, Triana L (2023) US FDA Safety Communication on Breast Implant Associated Squamous Cell Carcinoma BIA-SCC) [published online ahead of print, 2023 Feb 23]. Aesthetic Plast Surg. https://doi.org/10.1007/s00266-023-03283-5
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study did not require any ethics approval.
Informed consent
This article does not contain any studies involving human participants or animals performed by any of the authors.
Conflict of interest
Domenico Pagliara, Federica Grieco, Roberto Cuomo, Laurenza Schiavone, Filippo Boriani, Andrea Figus, Matteo Atzeni, Diego Ribuffo, Marzia Salgarello, Corrado Rubino declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pagliara, D., Grieco, F., Cuomo, R. et al. Breast implant-associated squamous cell carcinoma: an evidence-based systematic review. Eur J Plast Surg 46, 875–886 (2023). https://doi.org/10.1007/s00238-023-02078-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02078-w