Abstract
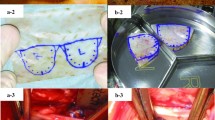
Pectus excavatum is the most common congenital chest wall deformity. Customised silicone implants have been used to camouflage this deformity with good short-term outcomes. In the long term, permanent implants have a significant risk of capsular contracture, migration and extrusion. Scaffold-guided tissue engineering provides an alternative autologous solution which avoids issues associated with permanent implants. We implanted a 3D-printed, custom-made, biodegradable and highly porous scaffold filled with autologous fat graft. We were able to sustain autologous fat in the construct. There was an excellent aesthetic outcome and the highly porous polycaprolactone implant was well tolerated by the patient. This case illustrates the first-in-human trial of soft tissue engineering to camouflage a pectus excavatum defect not reconstructable by conventional techniques.
Level of evidence: Level V, therapeutic study.




Similar content being viewed by others
Data availability
There is availability of the data and material for this case study.
References
Shamberger RC (1996) “Congenital chest wall deformities”, (in eng). Curr Probl Surg 33(6):469–542. https://doi.org/10.1016/s0011-3840(96)80005-0
Buziashvili D, Gopman JM, Weissler H, Bodenstein L, Kaufman AJ, Taub PJ (2019) An evidence-based approach to management of pectus excavatum and carinatum. Ann Plast Surg 82(3):352–358. https://doi.org/10.1097/sap.0000000000001654
Obermeyer RJ, Cohen NS, Jaroszewski DE (2018) “The physiologic impact of pectus excavatum repair”, (in eng). Semin Pediatr Surg 27(3):127–132. https://doi.org/10.1053/j.sempedsurg.2018.05.005
Kelly RE Jr (2008) “Pectus excavatum: historical background, clinical picture, preoperative evaluation and criteria for operation”, (in eng). Semin Pediatr Surg 17(3):181–193. https://doi.org/10.1053/j.sempedsurg.2008.03.002
Koumbourlis AC (2009) “Pectus excavatum: pathophysiology and clinical characteristics”, (in eng). Paediatr Respir Rev 10(1):3–6. https://doi.org/10.1016/j.prrv.2008.12.002
Chavoin JP et al (2016) Correction of pectus excavatum by custom-made silicone implants: contribution of computer-aided design reconstruction. A 20-year experience and 401 cases,” (in eng). Plast Reconstr Surg 137(5):860e–71e. https://doi.org/10.1097/prs.0000000000002071
Kelly RE Jr et al (2008) “Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study”, (in eng). Pediatrics 122(6):1218–1222. https://doi.org/10.1542/peds.2007-2723
Deva AK, Cuss A, Magnusson M, Cooter R (2019) The “game of implants”: a perspective on the crisis-prone history of breast implants,” (in eng). Aesthet Surg J 39(Suppl_1):S55-s65. https://doi.org/10.1093/asj/sjy310
Ariani N et al (2013) ”Current state of craniofacial prosthetic rehabilitation,” (in eng). Int J Prosthodont 26(1):57–67. https://doi.org/10.11607/ijp.3220
Wagner RD, Braun TL, Zhu H, Winocour S (2019) “A systematic review of complications in prepectoral breast reconstruction”, (in eng). J Plast Reconstr Aesthet Surg 72(7):1051–1059. https://doi.org/10.1016/j.bjps.2019.04.005
Pool SMW, Wolthuizen R, Mouës-Vink CM (2018) “Silicone breast prostheses: a cohort study of complaints, complications, and explantations between 2003 and 2015”, (in eng). J Plast Reconstr Aesthet Surg 71(11):1563–1569. https://doi.org/10.1016/j.bjps.2018.07.010
Leberfinger AN et al (2017) “Breast implant-associated anaplastic large cell lymphoma: a systematic review”, (in eng). JAMA Surg 152(12):1161–1168. https://doi.org/10.1001/jamasurg.2017.4026
Loch-Wilkinson A et al (2017) “Breast implant-associated anaplastic large cell lymphoma in Australia and New Zealand: high-surface-area textured implants are associated with increased risk”, (in eng). Plast Reconstr Surg 140(4):645–654. https://doi.org/10.1097/prs.0000000000003654
Rocha FP, Pires JA, Torres VF, Fagundes DJ (2012) “Treatment of bilateral mammary ptosis and pectus excavatum through the same incision in one surgical stage”, (in eng). Sao Paulo Med J 130(3):198–201. https://doi.org/10.1590/s1516-31802012000300010
Grappolini S, Fanzio PM, D’Addetta PG, Todde A, Infante M (2008) “Aesthetic treatment of pectus excavatum: a new endoscopic technique using a porous polyethylene implant”, (in eng). Aesthetic Plast Surg 32(1):105–110. https://doi.org/10.1007/s00266-007-9025-6
Loch-Wilkinson A et al (2020) Breast implant-associated anaplastic large cell lymphoma in Australia: a longitudinal study of implant and other related risk factors. Aesthet Surg J 40(8):838–846. https://doi.org/10.1093/asj/sjz333
Rubin JP, Yaremchuk MJ (1997) “Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: a comprehensive review of the literature”, (in eng). Plast Reconstr Surg 100(5):1336–1353. https://doi.org/10.1097/00006534-199710000-00043
Lin CW, Liao SL (2017) “Long-term complications of different porous orbital implants: a 21-year review”, (in eng). Br J Ophthalmol 101(5):681–685. https://doi.org/10.1136/bjophthalmol-2016-308932
Ho Quoc C, Delaporte T, Meruta A, La Marca S, Toussoun G, Delay E (2013) ”Breast asymmetry and pectus excavatum improvement with fat grafting in eng,” (in eng). Aesthet Surg J 33(6):822–9. https://doi.org/10.1177/1090820x13493907
Groen JW et al (2016) “Autologous fat grafting in onco-plastic breast reconstruction: a systematic review on oncological and radiological safety, complications, volume retention and patient/surgeon satisfaction”, (in eng). J Plast Reconstr Aesthet Surg 69(6):742–764. https://doi.org/10.1016/j.bjps.2016.03.019
Kobbe P, Laubach M, Hutmacher DW, Alabdulrahman H, Sellei RM, Hildebrand F (2020) ”Convergence of scaffold-guided bone regeneration and RIA bone grafting for the treatment of a critical-sized bone defect of the femoral shaft,”(in eng). Eur J Med Res 25(1):70. https://doi.org/10.1186/s40001-020-00471-w
Les AS et al (2019) “3D-printed, externally-implanted, bioresorbable airway splints for severe tracheobronchomalacia”, (in eng). Laryngoscope 129(8):1763–1771. https://doi.org/10.1002/lary.27863
Probst FA, Hutmacher DW, Müller DF, Machens HG, Schantz JT (2010) “[Calvarial reconstruction by customized bioactive implant]”, (in ger). Handchir Mikrochir Plast Chir 42(6):369–373. https://doi.org/10.1055/s-0030-1248310.RekonstruktionderKalvariadurcheinpräfabriziertesbioaktivesImplantat
Seen S, Young S, Lang SS, Lim TC, Amrith S, Sundar G (2021) “Orbital implants in orbital fracture reconstruction: a ten-year series”, (in eng). Craniomaxillofac Trauma Reconstr 14(1):56–63. https://doi.org/10.1177/1943387520939032
Seen S et al (2018) “Permanent versus bioresorbable implants in orbital floor blowout fractures”, (in eng). Ophthalmic Plast Reconstr Surg 34(6):536–543. https://doi.org/10.1097/iop.0000000000001077
Sood V, Green GE, Les A, Ohye RG (2021) “Advanced therapies for severe tracheobronchomalacia: a review of the use of 3D-printed, patient-specific, externally implanted, bioresorbable airway splints”, (in eng). Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 24:37–43. https://doi.org/10.1053/j.pcsu.2021.02.001
Vikingsson L, Gómez-Tejedor JA, Gallego Ferrer G, Gómez Ribelles JL (2015) ”An experimental fatigue study of a porous scaffold for the regeneration of articular cartilage,”(in eng). J Biomech 48(7):1310–7. https://doi.org/10.1016/j.jbiomech.2015.02.013
Coleman SR (1997) “Facial recontouring with lipostructure”, (in eng). Clin Plast Surg 24(2):347–367
Woodruff MA, Hutmacher DW (2010) ”The return of a forgotten polymer-polycaprolactone in the 21st century,”. Progress in Polymer Science 35(10):1217–1256. https://doi.org/10.1016/j.progpolymsci.2010.04.002
Y. Yuan, S. Zhang, J. Gao, and F. Lu 2015 “Spatial structural integrity is important for adipose regeneration after transplantation,” (in Eng), Archives of dermatological research, https://doi.org/10.1007/s00403-015-1574-y.
Chhaya MP, Balmayor ER, Hutmacher DW, Schantz JT (2016) Transformation of breast reconstruction via additive biomanufacturing. Sci Rep 6:28030. https://doi.org/10.1038/srep28030
Cheng M et al (2021) A preclinical animal model for the study of scaffold-guided breast tissue engineering. Tissue Eng Part C Methods 27(6):366–377. https://doi.org/10.1089/ten.TEC.2020.0387
Acknowledgements
The authors would like to thank Mohit P. Chhaya, PhD, and Sara Lucarotti, M.E. (BellaSeno GmbH) for designing and manufacturing the pectus excavatum scaffold.
Author information
Authors and Affiliations
Contributions
All authors contributed to this work as defined by the International Committee of Medical Journal Editors.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This case was reviewed by our institution’s clinical ethics committee where it was agreed that offering the patient an experimental treatment was acceptable (Approval number: HREC/2021/QMS/69789).
Patient consent
The patient gave written consent regarding publishing her data and photographs.
Competing interests
Dietmar W. Hutmacher is a founder and shareholder of BellaSeno GmbH. Matthew E. Cheng, Jan Janzekovic, Harrison J. Theile, Caitlin Rutherford Heard, Marie Luise Wille, Chris Cole, Thomas B. Lloyd, Richard J. W. Theile and Michael Wagels declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheng, M.E., Janzekovic, J., Theile, H.J. et al. Pectus excavatum camouflage: a new technique using a tissue engineered scaffold. Eur J Plast Surg 45, 177–182 (2022). https://doi.org/10.1007/s00238-021-01902-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-021-01902-5