Abstract
Background
Post-burn axillary adduction contractures (PBAAC) are commonly seen burn sequelae. They occur in various forms. By imposing colossal restriction on the range of mobility of the shoulder, they completely intervene with the upper limb over head functions.
Methods
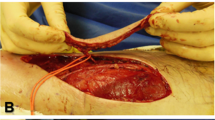
In 15 fresh frozen cadavers, 30 specimens of thoracodorsal vessel axes were studied after dye injection. Cadaveric study was conducted to standardise and stratify the clinical approach for harvesting perforator propeller flaps based on the thoracodorsal vessel axis (TDVA) by clear demonstration of various types of perforators arising from them. Three types of perforators (musculocutaneous, septocutaneous and direct cutaneous perforators were demonstrated), their dimensions, distribution and surface anatomy were defined. This knowledge paved the way for a stratified approach in harvesting the TDAPs (thoracodorsal artery perforator propeller flaps) for the reconstruction of PBAACs. The documents containing the data of 36 patients who underwent PBAAC reconstruction from 2010 to 2016 using perforators from TDVA (thoraco dorsal vessels axis) were collected for the retrospective study. Twelve patients underwent TDVA septofasciocutaneous perforator-based flap reconstruction for type 2 PBAACs. In 14 patients, post-burn axillary contractures were reconstructed with musculocutaneous perforator of TDVA (for type 3 PBAACs). Ten patients with type 1 PBAACs were reconstructed with direct cutaneous perforators of the TDVA. The average follow-up period was 18 months.
Results
All the flaps survived completely with no major complications. Average pre-operative range of abduction was 45.5°. The average post-operative pain free abduction obtained in 36 cases was 146.38° at an average of 18 months.
Conclusion
The challenging reconstruction of PBAACs can be simplified by the stratified approach using TDVA perforator-based propeller flaps. Perforator propeller flap based on the direct cutaneous perforator from the TDVA is most suitable for type 1 PBAAC reconstruction, whereas type 2 and type 3 PBAACs can be best served by septofasciocutaneous and musculocutaneous based perforator propeller flaps, respectively.
Level of Evidence: Level IV, therapeutic study.







Similar content being viewed by others
References
Kurtzman LC, Stern PJ (1990) Upper extremity burn contractures. Hand Clin 6:261–279
Wolfe, Hotchkiss, Pederson, Kozin (2011) Greens operative hand surgery, 6th edn. Elsevier, Churchill Livingstone, p 2106
Stekelenburg CM, Jaspers ME, Jongen SJ, Baas DC, Gardien KL, Hiddingh J, van Zuijlen PP (2017) Perforator-based interposition flaps perform better than full-thickness grafts for the release of burn scar contractures: a multicenter randomized controlled trial. Plast Reconstr Surg 139(2):501e–509e
Moroz VY, Yudenich AA, Sarygin PV, Sharobaro VI (2003) The elimination of post burn scar contractures and deformities of the shoulder joint. Ann Burns Fire Disasters 16:140–143
Tanaka A, Hatoko M, Tada H, Kuwahara M (2003) An evaluation of functional improvement following surgical corrections of severe burn contractures in axilla. Burns 29:153–157
Angrigiani C, Grilli D, Siebert J (1995) Latissimus dorsi musculocutaneous flap without muscle. Plast Reconstr Surg 96:1608–1614
Spinelli HM, Fink JA, Muzaffar AR (1996) The latissimus dorsi perforator-based fasciocutaneous flap. Ann Plast Surg 37:500–506
Schwabegger AH, Bodner G, Ninkovic M, Piza-Katzer H (2002) Thoracodorsal artery perforator (TAP) flap: report of our experience and review of the literature. Br J Plast Surg 55:390–395
Heitmann C, Guerra A, Metzinger SW, Levin LS, Allen RJ (2003) The thoracodorsal artery perforator flap: anatomic basis and clinical application. Ann Plast Surg 51(1):23–29
Guerra AB, Metzinger SE, Lund KM, Cooper MM, Allen RJ, Dupin CL (2004) The thoracodorsal artery perforator flap: clinical experience and anatomic study with emphasis on harvest techniques. Plast Reconstr Surg 114:32–41
Laredo-Ortiz C, Salvador-Sanz J, Marquez Mendoza M et al (2005) Pedicled thoracodorsal arterial perforator flap for re- construction of a large defect post-burn in posterior side of the arm. Burns 31:108–112
Er E, Ucar C (2005) Reconstruction of axillary contractures with thoracodorsal perforator island flap. Burns 31:726–730
Rehman N, Kannan RY, Hassan S, Hart NB (2005) Thoracodorsal artery perforator (TAP) type I V-Y advancement flap in axillary hidradenitis suppurativa. Br J Plast Surg 58:441–444
George C, Cormack B, George H, Lamberty (1994) The arterial anatomy of skin flaps. Chruchill Livingstone 2nd ed. 160-161: 473–477
De Coninck A, Boeckx W, Vanderlinden E, Claessen G (1975) Autotransplants avec micro sutures vasculaires. Anatomie des zones donneuses. Ann Chir Plast 20:163–170
Cabanie H, Garbe J-F, Guimberteau J-C (1980) Anatomical basis of the thoracodorsal axillary flap with respect to its transfer by means of microvascular surgery. Anat Clin 2:65–73 6
Yang ZN, Shih H-R, Chao L, Shih T-S (1983) Free transplantation of sub-axillary lateral thoracodorsal flap in bum surgery. Bums 10:164–169
Chandra R, Kumar P, Abdi SHM (1988) The subaxillary pedicled flap. Br J Plast Surg 41:169–173
Walash A, Kishk T, Ghareeb FM (2014) Treatment of postburn axillary contracture. Menofia Med J 27:278–283
Ogawa R, Hyakusoku H, Murakami M, Koike S (2003) Reconstruction of axillary scar contractures—retrospective study of 124 cases over 25 years. Br J Plast Surg 56:100–105
Kim DY, Cho SY, Kim KS, Lee SY, Cho BH (2000) Correction of axillary burn contractures with thoracodorsal perforator based cutaneous island flaps. Ann Plast Surg 44:181–187
Rowsell AR, Eisenberg DN, Taylor GI (1984) The anatomy of the subscapular-thoracodorsal arterial sys- tem: a study of 100 cadaver dissections. Br J Plast Surg 37:574–576
Khoobehi K, Allen RJ, Montegut WJ (1996) Thora- codorsal artery perforator flaps for reconstruction (Ab-stract). South Med J 89(Suppl):S110
Kim JT, Koo BS, Kim SK (2001) The thin latissimus dorsi perforator-based free flap for resurfacing. Plast Reconstr Surg 107:374–382
Koshima I, Saisho H, Kawada S, Hamanaka T, Umeda N, Moriguchi T (1999) Flow-through thin latissimus dorsi perforator flap for repair of soft-tissue defects in the legs. Plast Reconstr Surg 103:1483–1490
Karki D, Mehta N, Narayan RP (2014) Post-burn axillary contracture: A therapeutic challenge! Indian J Plast Surg 47(3):375–380
Acknowledgements
We sincerely thank Dr. P. Parasakthi, MD, Professor and head of the department of Forensic medicine for facilitating the cadaveric dissection and injection studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Institutional ethical committee approval was obtained for both cadaveric and clinical studies. Apart from the informed consent obtained from each patient, permission was taken from each one of them for exhibition of their photos and clinical materials for the research and study.
Conflicts of interests
Thalaivirithan Margabandu Balakrishnan, Janhavi Venkataraman and Janardhanam Jaganmohan declare that they have no conflict of interest.
Funding
Nil.
Patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal.
The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Rights and permissions
About this article
Cite this article
Balakrishnan, T.M., Venkataraman, J. & Jaganmohan, J. A stratified reconstructive approach for the post burn axillary adduction contractures based on the anatomical study of thoracodorsal vessel perforator system. Eur J Plast Surg 41, 693–702 (2018). https://doi.org/10.1007/s00238-018-1440-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-018-1440-1