Abstract
Background
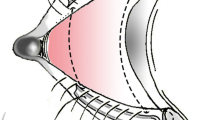
Lower eyelid malposition is a common clinical finding encountered by the oculoplastic surgeon. We examine the short-term results with the use of the tarSys spacer graft for the correction of lower eyelid malposition.
Methods
A retrospective chart review of one surgeon’s outcomes with use of tarSys spacer graft for lower eyelid malposition was conducted.
Results
Preoperative margin-to-reflex distance 2 (MRD2) ranged from 8 to 15 mm with a mean of 9.5 mm (±2.4 mm) and median 8.25 mm. Mean postoperative MRD2 was 6.2 (±3.4 mm) ranging from 4 to 17 mm with a median of 5.0 mm. Improvement in MRD2 averaged 3.33 (±2.07 mm), range −2 to 6 mm, and a median of 3.25 mm. Preoperative lagophthalmos ranged from 0 to 10 mm with mean 3.9 (±3.6 mm) and a median of 3.0 mm. Mean postoperative lagophthalmos was 1.3 (±1.5 mm) ranging from 0 to 4 mm with a median of 0.7 mm. Improvement in lagophthalmos averaged 2.5 (±2.7 mm).
Conclusions
The tarSys spacer graft should be thought of as a dependable allogenic implant for posterior lamellar support when correcting lower eyelid malposition.
Level of Evidence: Level V, therapeutic study.



Similar content being viewed by others
References
Milz S, Neufang J, Higashiyama I, Putz R et al (2005) An immunohistochemical study of the extracellular matrix of the tarsal plate in the upper eyelid in human beings. J Anat 206:37–45
Kakizaki H, Malhotra R, Madge SN, Selva D (2009) Lower eyelid anatomy: an update. Ann Plast Surg 63:344–51
Rafii AA, Enepekides DJ (2006) Upper and lower eyelid reconstruction: the year in review. Curr Opin Otolaryngol Head Neck Surg 14:227–33
Korn BS, Kikkawa DO, Cohen SR, Hartstein M et al (2008) Treatment of lower eyelid malposition with dermis fat grafting. Ophthalmol 115:744–751, e2
Wearne MJ, Sandy C, Rose GE, Pitts J et al (2001) Autogenous hard palate mucosa: the ideal lower eyelid spacer? Br J Ophthalmol 85:1183–7
Özkaya Ö, Karşidag S, Egemen O, Akçal AÖ, Şirvan S, Kabukçuoglu F (2012) Comparative analysis of the nail xenografts with cartilage autografts in eyelid reconstruction. J Craniofac Surg 23:1028–31
Sullivan SA, Dailey RA (2003) Graft contraction: a comparison of acellular dermis versus hard palate mucosa in lower eyelid surgery. Ophthal Plast Reconstr Surg 19:14–24
Badylak SF (2001) The extracellular matrix as a scaffold for tissue reconstruction. Semin Cell Dev Biol 13:377–383
Abraham GA, Murray J, Billiar K, Sullivan SJ (2005) Evaluation of the porcine intestinal collagen layer as a biomaterial. J Biomed Mater Res 51:442–52
Raghavan D, Kropp BP, Lin HK, Zhang Y et al (2005) Physical characteristics of small intestinal submucosa scaffolds are location-dependent. J Biomed Mater Res A 73:90–6
Ansaloni L, Cambrini P, Catena F et al (2007) Immune response to small intestinal submucosa (surgisis) implant in humans: preliminary observations. J Invest Surg 20:237–41
Harth KC, Rosen MJ (2009) Major complications associated with xenograft biologic mesh implantation in abdominal wall reconstruction. Surg Innov 16:324–329
Bedran EG, Pereira MV, Bernardes TF (2010) Ectropion. Semin Ophthalmol 25:59–65
Dryden RM, Soll DB (1977) The use of scleral transplantation in cicatricial entropion and eyelid retraction. Trans Am Ophthalmol Otol 83:669
Siegel R (1985) Palatal grafts for eyelid reconstruction. Plast Reconstr Surg 76:411–414
Tan I, Olver J, Wright M, Maini R, Neoh C et al (2004) The use of porous polyethylene (Medpor) lower eyelid spacers in lid heightening and stabilization. Br J Ophthalmol 88:1197–1200
Li TG, Shorr N, Goldberg RA (2005) Comparison of the efficacy of hard palate grafts with acellular human dermis grafts in lower eyelid surgery. Plast Reconstr Surg 116:873
Conflict of interest
Dr. Cohen was a paid speaker in 2012 for the IOP Corporation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leonard, J.H., Cohen, A.J. Use of the tarSys® for posterior lamellar grafting for lower eyelid malposition. Eur J Plast Surg 36, 733–738 (2013). https://doi.org/10.1007/s00238-013-0882-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-013-0882-8