Abstract
Background
Hyaluronidases are commonly employed in aesthetic medicine to reverse the effects of the injected hyaluronic acid filler, eliminating nodules, correcting the injection of excessive quantities of filler, or reducing the odds of ischemic complications, although toxicity studies and clear guidelines are lacking in the literature. The objective of this study was to evaluate effects of hyaluronidases on skin and soft tissue viability.
Methods
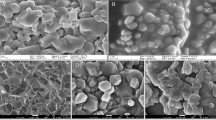
Human fibroblast cell and human skin cultures were grown under different concentrations of hyaluronidases. Cell viability and proliferation were tested with the hemocytometric assay with Trypan blue and colorimetric assay with 4,5-dimethylthiazol-22,5-difenil tetrazolium bromide.
Results
The viability of fibroblast cultures was not significantly affected by the enzyme concentration or the time of exposure, exceeding 70 % of viability in all cases. The viability of the tissue samples showed a decrease, inferior to 70 % of viability at 6.5 and 14 U, independently from the time of exposure, although not statistically significant.
Conclusions
Hyaluronidases do not affect fibroblast proliferation, although high concentrations of the enzyme may be able to inhibit human skin viability. This result could be influenced by the absence of growth medium; this result should be confirmed by further studies.






Similar content being viewed by others
References
Girish KS, Kemparaju K (2007) The magic glue hyaluronan and its eraser hyaluronidase: a biological overview. Life Sci 80(21):1921–1943
Meyer K (1971) Hyaluronidases. In: Boyer PD (ed) The enzymes. Academic, New York, pp 307–320
El-Saforya NS, Fazaryb AE, Leea CK (2010) Hyaluronidases, a group of glycosidases: current and future perspectives. Carb Pol 81:165–181
Hotez PJ, Narasimhan S, Haggerty J, Milstone L, Bhopale V, Schad GA et al (1992) Hyaluronidase from infective Ancylostoma hookworm larva and its possible function as a virulence factor in tissue invasion and in cutaneous larva migrans. Infect Immun 60:1018–1023
Duran-Reynals F (1928) Exaltation de l’activité du virus vaccinal par les extraits de certains organs. Comptes Rendus des Séances de la Société de Biologie et de Ses Filiales, 99, pp 6–7
Kohno N, Ohnuma T, Truog P (1994) Effects of hyaluronidase on doxorubicin penetration into squamous carcinoma multicellular tumor spheroids and its cell letality. J Cancer Res Clin Oncol 120:293–297
Kempeneers A, Dralands L, Ceuppens J (1992) Hyaluronidase induced orbital pseudotumor as complication of retrobulbar anesthesia. Bull Soc Belge Ophtalmol 243:159–166
Kim JH, Choi GS, Ye YM, Nahm DH, Park HS (2009) Acute urticaria caused by the injection of goat-derived hyaluronidase. Allergy Asthma Immunol Res 1(1):48–50
Schulze C, Bittorf T, Walzel H, Kundt G, Bader R, Mittelmeier W (2008) Experimental evaluation of hyaluronidase activity in combination with specific drugs applied in clinical techniques of interventional pain management and local anaesthesia. Pain Physician 11(6):877–883
Evison M, Wing V (2009) Human recombinant hyaluronidase (Cumulase®) improves intracytoplasmic sperm injection survival and fertilization rates. Reproductive BioMedicine Online 18(6):811–814
Racz GB, Heavner JE, Trescot A (2008) Percutaneous lysis of epidural adhesions—evidence for safety and efficacy. Pain Pract 8:277–286
Dunn AL, Heavner JE, Racz G, Day M (2010) Hyaluronidase: a review of approved formulations, indications and off-label use in chronic pain management. Expert Opin Biol Ther 10(1):127–131
Narins RS, Coleman WP, Glogau RG (2009) Recommendations and treatment options for nodules and other filler complications. Dermatol Surg 35:1667–1671
Kim DW, Yoon ES, Ji YH, Park SH, Lee BI, Dhong ES (2011) Vascular complications of hyaluronic acid fillers and the role of hyaluronidase in management. J Plast Reconstr Aesthet Surg 64(12):1590–1595
Szepfalusi Z, Nentwich I, Dobner M, Pillwein K, Urbanek R (1997) IgE-mediated allergic reaction to hyaluronidase in paediatric oncological patients. Eur J Pediatr 156(3):199–203
Escolano F, Pares N, Gonzalez I, Castillo J, Valero A, Bartolome B (2005) Allergic reaction to hyaluronidase in cataract surgery. Eur J Anaesthesiol 22(9):729–730
Kim TW, Lee JH, Yoon KB, Yoon DM (2011) Allergic reactions to hyaluronidase in pain management—a report of three cases. Korean J Anesthesiol 60(1):57–59
Sclafani AP, Fagien S (2009) Treatment of injectable soft tissue filler complications. Dermatol Surg 35(Suppl 2):1672–1680
Hengstler JG, Van der Burg B, Steinberg P, Oesch F (1999) Interspecies differences in cancer susceptibility and toxicity. Drug Metab Rev 31(4):917–970
Erickson-Miller CL, May RD, Tomaszewski J, Osborn B, Murphy MJ, Page JG et al (1997) Differential toxicity of camptothecin, topotecan and 9-aminocamptothecin to human, canine, and murine myeloid progenitors (CFU-GM) in vitro. Cancer Chemother Pharmacol 39(5):467–472
Fotakis G, Timbrell JA (2006) In vitro cytotoxicity assays: comparison of LDH, neutral red, MTT and protein assay in hepatoma cell lines following exposure to cadmium chloride. Toxicol Lett 160(2):171–177
ISO 10993-5, 2009. Biological evaluation of medical devices. Part 5: Tests for in vitro cytotoxicity
Menon H, Thomas M, D’silva J (2010) Low dose of hyaluronidase to treat over correction by HA filler—a case report. J Plast Reconstr Aesthet Surg 63:e416–417
Hirsch RJ, Cohen JL, Carruthers JD (2007) Successful management of an unusual presentation of impending necrosis following a hyaluronic acid injection embolus and a proposed algorithm for management with hyaluronidase. Dermatol Surg 33(3):357–360
Gottlieb JL, Antoszyk AN, Hatchell DL, Saloupis P (1990) The safety of intravitreal hyaluronidase. A clinical and histologic study. Invest Ophthalmol Vis Sci 31(11):2345–2352
Jumper JM, McCauley MB, Equi RA, Duncan KG, Duncan J, Schwartz DM (2002) Corneal toxicity of intraocular hyaluronidase. J Ocul Pharmacol Ther 18(1):89–97
Birkenmaier C, Redeker J, Sievers B, Melcher C, Jansson V, Mayer-Wagner S (2011) An evaluation of medications commonly used for epidural neurolysis procedures in a human fibroblast cell culture model. Reg Anesth Pain Med 36(2):140–144
Park TH, Seo SW, Kim JK, Chang CH (2011) Clinical experience with hyaluronic acid-filler complications. J Plast Reconstr Aesthet Surg 64:892–897
Hirsch R, Narurkar V, Carruthers J (2006) Management of injected hyaluronic acid induced Tyndall effects. Lasers Surg Med 38:202–204
Cox S (2009) Clinical experience with filler complications. Dermatol Surg 35(S2):1661–1666
Van Dyke S, Hays G, Caglia A, Caglia M (2010) Severe acute local reactions to a hyaluronic acid-derived dermal filler. J Clin Aesthet Dermatol 3(5):32–35
Lambros V (2004) Letter to the editor: the use of hyaluronidase to reverse the effects of hyaluronic acid filler. Plast Reconstr Surg 114:277
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cavallini, M., Antonioli, B., Gazzola, R. et al. Hyaluronidases for treating complications by hyaluronic acid dermal fillers: evaluation of the effects on cell cultures and human skin. Eur J Plast Surg 36, 477–484 (2013). https://doi.org/10.1007/s00238-013-0855-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-013-0855-y