Abstract
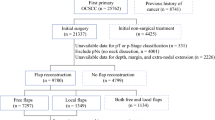
The objective of this study is to evaluate the impact of microsurgical reconstruction on local recurrence rates and disease-specific survival in patients with oral squamous cell carcinoma. This study is a retrospective review of patients treated at a tertiary cancer center. Six hundred and five patients were included in this study with 529 males (87.44%) and 76 females (12.56%). These were composed of 467 (77.19%) pedicled-flaps reconstructions and 138 (22.81%) free-flap procedures. There was no difference between the groups regarding T stage, N stage, or type of oncological surgery. Use of postoperative radiotherapy was more common in the free-flap group with a significantly shorter time interval than the pedicled-flap group. Free-flap patients had a lower proportion of compromised/close surgical margins (p < 0.0001). Univariate analysis disclosed as significant for local recurrence: gender, T stage, microsurgical reconstruction, lymphatic embolization, neural infiltration, and surgical margins. In a multivariate model, T stage (p < 0.001), neural infiltration (p < 0.001), and microsurgical reconstruction (p < 0.001) remained significant. Significant factors for survival in univariate analysis were: gender, T stage, N stage, synchronous neck dissection, microsurgical reconstruction, lymphatic embolization, neural infiltration, and surgical margins. In a multivariate analysis, T stage (p < 0.001), N stage (p < 0.001), synchronous neck dissection (p = 0.025), microsurgical reconstruction (p < 0.001), lymphatic embolization (p = 0.023), and neural infiltration (p < 0.001) remained significant. Regression trees show a significant impact of free flaps in T3/T4 primary tumors. Use of microsurgical flaps provides a significant improvement in local recurrence and survival in patients with T3–T4a primary tumors. It also reduces the interval between surgery and radiotherapy.




Similar content being viewed by others
References
Blackwell KE (1999) Unsurpassed reliability of free flaps for head and neck reconstuction. Arch Otolaryngol Head Neck Surg 125(3):295–299
Markannen-Leppänen M, Mäkitie AA, Haapanen ML, Suominen E, Asko-Seljavaara S (2006) Quality of life after free-flap reconstruction in patients with oral and pharyngeal cancer. Head Neck 28(3):210–216
Gal TJ, Futran ND (2002) Outcomes research in head and neck reconstruction. Facial Plast Surg 18(2):113–117
Tsue TT, Desyatnikova SS, Futran ND, Stack BC Jr, Weymuller EA, Glenn MG (1997) Comparison of cost and function in reconstruction of posterior oral cavity and oropharynx. Free vs. pedicled soft tissue transfer. Arch Otolaryngol Head Neck Surg 123(7):731–737
Chen PH, Shieh TY, Ho PS, Tsai CC, Yang YH, Lin YC et al (2007) Prognostic factors associated with the survival of oral and pharyngeal cancer in Taiwan. BMC Cancer 7(10):1–13
Mistry RC, Qureshi SS, Kumaran C (2005) Post-resection mucosal margin in oral cancer: quantification and significance. J Surg Oncol 91(2):131–133
Spiro RH, Guillamondegui O, Paulino AF, Huvos AG (1999) Pattern of invasion and margin assessment in patients with oral tongue cancer. Head Neck 21(5):408–413
Sessions DG, Spector GJ, Lenox J, Haughey B, Chao C, Marks J (2002) Analysis of treatment results for oral tongue cancer. Laryngoscope 112(4):616–625
Pandey M, Rao LP, Das SR, Shukla M (2009) Tumor stage and resection margins not the mandibular invasiondetermines the survival in patients with cancers of the oro-mandibular region. Eur J Surg Oncol 35(12):1337–1342
Bernier J, Cooper JS, Pajak TF, van Glabbeke M, Bourhis J, Forastiere A, Ozsahin EM, Jacobs JR, Jassem J, Ang KK, Lefèbvre JL (2005) Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head Neck 27(10):843–850
Hanasono MM, Friel MT, Klem C, Hsu PW, Robb GL, Weber RS, Roberts DB, Chang DW (2009) Impact of reconstructive microsurgery in patients with advanced oral cavity cancers. Head Neck 31(10):1289–1296
Roostaeian J, Suh JD, Sercarz JA, Abemayor E, Lee JT, Blackwell KE (2005) Factors affecting recurrence after microvascular flap reconstruction of the head and neck. Laryngoscope 115(8):1391–1394
Moncrieff MD, Spira K, Clark JR, Thompson JF, Clifford AR, O’Brien CJ, Shannon KF (2010) Free flap reconstruction for melanoma of the head and neck: indications and outcomes. J Plast Reconstr Aesthet Surg 63(2):205–212. doi:10.1016/j.bjps.2008.11.027
Vikram B (1979) Importance of the time interval between surgery and postoperative radiation therapy in the combined management of head & neck cancer. Int J Radiat Oncol Biol Phys 5(10):1837–1840
Conflict of interest
The authors have no conflict of interest or financial support to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rodrigues, M.L., Köhler, H.F., Magrin, J. et al. Which oral cancer patients benefit the most from microsurgical reconstruction?. Eur J Plast Surg 34, 75–80 (2011). https://doi.org/10.1007/s00238-010-0462-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-010-0462-0