Abstract
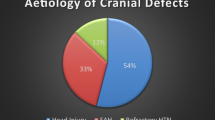
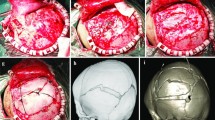
During the 5-year war in former Yugoslavia 294 patients were surgically treated for head injuries at the Neurosurgical Department of the Emergency Center, Clinical Center of Serbia in Belgrade. In addition to other problems related to direct trauma of brain tissue, some specific problems related to other tissue defects and their importance in further complications which changed the final outcome have been noted. This study analyzed methods and materials used for dura, bone, and skin reconstruction in a search for better management of this problem. We conclude that for dural reconstruction in these patients the best materials are autologous (autotransplantation of periosteum, galea aponeurotica, or fascia lata) since this results in fewer complications and better results. Local skin flaps were used for small skin defects, but more extensive skin defects required larger flaps with free skin grafting of secondary defects. Both dura and skin reconstruction should be performed as soon as possible to prevent infection and other complications, but delayed surgery is recommended for bone defects. Only bone defects with diameter over 3–4 cm were treated surgically (alloplastic material, Palacos, being used) after 6–12 months in cases with no signs of infection. This strategy yielded the best results.
Similar content being viewed by others
References
Aarabi B (1990) Surgical outcome in 435 patients who sustained missile head wounds during Iran-Iraq war. Neurosurgery 27:692–695
Baumer F, Golling M, Taruttis H (1992) Gunshot injuries-their incidence and surgical problems. Aktuelle Traumatol 22:96–101
Benzel EC, Day WT, Kesterson L, Willis BK, Kessler CW, Modling B, Hadeu TA (1991) Civilian craniocerebral gunshot wounds. Neurosurgery 29:67–72
Brandvold B, Levi L, Peinsod M, George ED (1990) Penetrating craniocerebral injuries in the Israeli involvement in the Lebanese conflict 1982–1985. Analyses of the less aggressive surgical approach. J Neurosurg 72:15–21
Carey ME, Sarna GS, Farrell JB, Happel LT (1989) Experimental missile wound to the brain. J Neurosurg 71:754–764
Chauhdri KA, Choudhury AR, al-Moutaery KR, Cybulsky GR (1994) Penetrating craniocerebral shrapnel injuries during Operation Desert Storm: early results of conservative surgical treatment. Acta Neurochir (Wien) 126–:120–123
Clark WC, Mühlbauer MS, Watridge CB, Ray MW (1986) Analyses of 76 civilian craniocerebral gunshot wounds. J Neurosurg 65:9–14
Cushing H (1918) A study of a series of wounds involving the brain and its enveloping structures. Br J Surg 5:558–684
Grahm TW, Williams FC Jr, Harrington T, Spetzler RF (1990) Civilian gunshot wounds to the head. A prospective study. Neurosurgery 27:696–700
Hammon WM (1971) Analyses of 2187 consecutive penetrating wounds of the brain from Vietnam. J Neurosurg 34:127–131
Jefferson G (1919) The physiological pathology of gunshot wounds of the head. Br J Surg 7:262–289
Kaufman HH (1993) Civilian gunshot wounds to the head. Neurosurgery 32:962–964
Khilkov VA, Usanov EI, Umerov EKH, Barchukov VG, Bolotov AA, Belozrov VV (1994) The prediction of cranioplasty outcomes after gunshot wounds of the skull and brain. Voen Med Zh 2:32–48
Piorrowski WP (1992) Results of treatment of brain gunshot injuries. Unfallchirurg 95:74–77
Segal DH, Oppenheim JS, Murovic JA (1994) Neurosurgical recovery after cranioplasty. Neurosurgery 34:729–731
Shul MR, Glawe H, Siedschlag WD, Nisch G, Winkelmann H (1992) Conservative or surgical treatment for foreign body injuries of the brain. Zentralbl Neurochir 53:69–73
Stone JL, Lictor T, Fitzgerald LF (1995) Gunshot wounds to the head in civilian practice. Neurosurgery 37:1104–1112
Author information
Authors and Affiliations
Corresponding author
Additional information
An invited commentary to this paper is available at: http://dx.doi.org./10.1007/s00238-003-0492-y
Rights and permissions
About this article
Cite this article
Vujotic, L.B., Jovanovic, M.J. & Colic, M.M. The selection of the most appropriate materials and the timing of procedures for dura, bone, and skin reconstruction in patients with wartime head injuries. Eur J Plast Surg 26, 181–184 (2003). https://doi.org/10.1007/s00238-003-0491-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-003-0491-z