Abstract
Purpose
The first-pass effect (FPE), defined as complete revascularization after a single thrombectomy pass in large vessel occlusion, is a predictor of good prognosis in patients with acute ischemic stroke (AIS) receiving mechanical thrombectomy (MT). We aimed to evaluate obesity-related indicators if possible be predictors of FPE.
Methods
We consecutively enrolled patients with AIS who were treated with MT between January 2019 and December 2021 at our institution. Baseline characteristics, procedure-related data, and laboratory test results were retrospectively analyzed. A multivariable logistic regression analysis was performed to evaluate the independent predictors of FPE.
Results
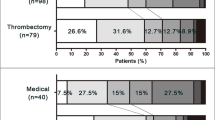
A total of 151 patients were included in this study, of whom 47 (31.1%) had FPE. After adjusting for confounding factors, the independent predictors of achieving FPE were low levels of body mass index (BMI) (OR 0.85, 95% CI 0.748 to 0.971), non-intracranial atherosclerotic stenosis (OR 4.038, 95% CI 1.46 to 11.14), and non-internal carotid artery occlusion (OR 13.14, 95% CI 2.394 to 72.11). Patients with lower total cholesterol (TC) (< 3.11 mmol/L) were more likely to develop FPE than those with higher TC (≥ 4.63 mmol/L) (OR 4.280; 95% CI 1.24 to 14.74)
Conclusion
Lower BMI, non-intracranial atherosclerotic stenosis, non-internal carotid artery occlusion, and lower TC levels were independently associated with increased rates of FPE in patients with AIS who received MT therapy. FPE was correlated with better clinical outcomes after MT.

Similar content being viewed by others
References
Feigin VL, Stark BA, Johnson CO et al (2021) Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol| 20:795–820. https://doi.org/10.1016/S1474-4422(21)00252-0
Eskey CJ, Meyers PM, Nguyen TN et al (2018) Indications for the performance of intracranial endovascular neurointerventional procedures: a scientific statement from the American Heart Association. Circulation 137:e661–e689. https://doi.org/10.1161/CIR.0000000000000567
Berkhemer OA, Fransen PSS, Beumer D et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20. https://doi.org/10.1056/NEJMoa1411587
Jovin TG, Chamorro A, Cobo E et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306. https://doi.org/10.1056/NEJMoa1503780
Zaidat OO, Castonguay AC, Linfante I et al (2018) First pass effect: a new measure for stroke thrombectomy devices. Stroke 49:660–666. https://doi.org/10.1161/STROKEAHA.117.020315
Mokin M, Primiani CT, Castonguay AC et al (2020) First pass effect in patients treated with the trevo stent-retriever: a TRACK Registry study analysis. Front Neurol 11:83. https://doi.org/10.3389/fneur.2020.00083
Di Maria F, Kyheng M, Consoli A et al (2021) Identifying the predictors of first-pass effect and its influence on clinical outcome in the setting of endovascular thrombectomy for acute ischemic stroke: results from a multicentric prospective registry. Int J Stroke 16:20–28. https://doi.org/10.1177/1747493020923051
Nikoubashman O, Dekeyzer S, Riabikin A et al (2019) True first-pass effect. Stroke 50:2140–2146. https://doi.org/10.1161/STROKEAHA.119.025148
Acute and Interventional Treatments | Stroke. https://www.ahajournals.org/doi/10.1161/STROKEAHA.122.041254?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed. Accessed 6 Mar 2023
Lu Y, Hajifathalian K, Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects) et al (2014) Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet 383:970–983. https://doi.org/10.1016/S0140-6736(13)61836-X
den Hartog SJ, Zaidat O, Roozenbeek B et al (2021) Effect of first-pass reperfusion on outcome after endovascular treatment for ischemic stroke. JAHA 10:e019988. https://doi.org/10.1161/JAHA.120.019988
Adams HP, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41. https://doi.org/10.1161/01.str.24.1.35
Barnett HJ, Taylor DW, Eliasziw M et al (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 339:1415–1425. https://doi.org/10.1056/NEJM199811123392002
Kim YD, Choi HY, Cho HJ et al (2010) Increasing frequency and burden of cerebral artery atherosclerosis in Korean stroke patients. Yonsei Med J 51:318. https://doi.org/10.3349/ymj.2010.51.3.318
von Kummer R, Broderick JP, Campbell BCV et al (2015) The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46:2981–2986. https://doi.org/10.1161/STROKEAHA.115.010049
Pasi M, Casolla B, Kyheng M et al (2021) Long-term functional decline of spontaneous intracerebral haemorrhage survivors. J Neurol Neurosurg Psychiatry 92:249–254. https://doi.org/10.1136/jnnp-2020-324741
Kalousek V, Yoo AJ, Sheth SA et al (2021) Cyclical aspiration using a novel mechanical thrombectomy device is associated with a high TICI 3 first pass effect in large-vessel strokes. J Neuroimaging 31:912–924. https://doi.org/10.1111/jon.12889
Schartz DA, Ellens NR, Kohli GS et al (2022) A meta-analysis of combined aspiration catheter and stent retriever versus stent retriever alone for large-vessel occlusion ischemic stroke. AJNR Am J Neuroradiol 43:568–574. https://doi.org/10.3174/ajnr.A7459
Serna Candel C, Aguilar Pérez M, Bäzner H et al (2021) First-pass reperfusion by mechanical thrombectomy in acute M1 occlusion: the size of retriever matters. Front Neurol 12:679402. https://doi.org/10.3389/fneur.2021.679402
Bai X, Zhang X, Wang J et al (2021) Factors influencing recanalization after mechanical thrombectomy with first-pass effect for acute ischemic stroke: a systematic review and meta-analysis. Front Neurol 12:628523. https://doi.org/10.3389/fneur.2021.628523
Bridging intravenous thrombolysis before mechanical thrombectomy for large artery occlusion may be detrimental with thrombus fragmentation | Bentham Science. http://www.eurekaselect.com/article/103161. Accessed 11 Apr 2022
Gutierrez J, Turan TN, Hoh BL, Chimowitz MI (2022) Intracranial atherosclerotic stenosis: risk factors, diagnosis, and treatment. The Lancet Neurology 21:355–368. https://doi.org/10.1016/S1474-4422(21)00376-8
Lee JS, Hong JM, Lee KS et al (2015) Endovascular therapy of cerebral arterial occlusions: intracranial atherosclerosis versus embolism. J Stroke Cerebrovasc Dis 24:2074–2080. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.05.003
Fitzgerald S, Dai D, Wang S et al (2019) Platelet-rich emboli in cerebral large vessel occlusion are associated with a large artery atherosclerosis source. Stroke 50:1907–1910. https://doi.org/10.1161/STROKEAHA.118.024543
Patel TR, Fricano S, Waqas M et al (2021) Increased perviousness on CT for acute ischemic stroke is associated with fibrin/platelet-rich clots. AJNR Am J Neuroradiol 42:57–64. https://doi.org/10.3174/ajnr.A6866
Yuki I, Kan I, Vinters HV et al (2012) The impact of thromboemboli histology on the performance of a mechanical thrombectomy device. AJNR Am J Neuroradiol 33:643–648. https://doi.org/10.3174/ajnr.A2842
Gunning GM, McArdle K, Mirza M, et al (2018). Clot friction variation with fibrin content; implications for resistance to thrombectomy. J Neurointerv Surg 10(1):34–38. https://doi.org/10.1136/neurintsurg-2016-012721
Dai L, Xu J, Zhang Y et al (2021) Cumulative burden of lipid profiles predict future incidence of ischaemic stroke and residual risk. Stroke Vasc Neurol 6:581–588. https://doi.org/10.1136/svn-2020-000726
Gu X, Li Y, Chen S et al (2019) Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke 50:3376–3384. https://doi.org/10.1161/STROKEAHA.119.026402
Rocha VZ, Libby P (2009). Obesity, inflammation, and atherosclerosis. Nature reviews. Cardiology 6(6):399–409. https://doi.org/10.1038/nrcardio.2009.55
Song K, Yi HJ, Lee DH, Sung JH (2021) Association of blood viscosity with first-pass reperfusion in mechanical thrombectomy for acute ischemic stroke. Clin Hemorheol Microcirc 77:233–244. https://doi.org/10.3233/CH-200979
Moreno L, Calderas F, Sanchez-Olivares G et al (2015) Effect of cholesterol and triglycerides levels on the rheological behavior of human blood. Korea-Aust Rheol J 27:1–10. https://doi.org/10.1007/s13367-015-0001-4
Rosenson RS, Shott S, Tangney CC (2002) Hypertriglyceridemia is associated with an elevated blood viscosity Rosenson: triglycerides and blood viscosity. Atherosclerosis 161:433–439. https://doi.org/10.1016/S0021-9150(01)00656-6
Ercan M, Konukoglu D, Yesim TE (2006) Association of plasma viscosity with cardiovascular risk factors in obesity: an old marker, a new insight. Clin Hemorheol Microcirc 35:441–446
Moriarty PM, Gibson CA (2005) Association between hematological parameters and high-density lipoprotein cholesterol. Curr Opin Cardiol 20:318–323. https://doi.org/10.1097/01.hco.0000167722.22453.47
Wang N, Tall AR (2016) Cholesterol in platelet biogenesis and activation. Blood 127:1949–1953. https://doi.org/10.1182/blood-2016-01-631259
Ma Y, Ashraf MZ, Podrez EA (2010) Scavenger receptor BI modulates platelet reactivity and thrombosis in dyslipidemia. Blood 116:1932–1941. https://doi.org/10.1182/blood-2010-02-268508
Fitzgerald S, Rossi R, Mereuta OM et al (2021) Large artery atherosclerotic clots are larger than clots of other stroke etiologies and have poorer recanalization rates. J Stroke Cerebrovasc Dis 30:105463. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105463
Darvall KAL, Sam RC, Silverman SH et al (2007) Obesity and thrombosis. Eur J Vasc Endovasc Surg 33:223–233. https://doi.org/10.1016/j.ejvs.2006.10.006
Blokhin IO, Lentz SR (2013) Mechanisms of thrombosis in obesity. Curr Opin Hematol 20:437–444. https://doi.org/10.1097/MOH.0b013e3283634443
Koge J, Tanaka K, Yoshimoto T et al (2022) Internal carotid artery tortuosity: impact on mechanical thrombectomy. Stroke. https://doi.org/10.1161/STROKEAHA.121.037904
Chen Z, Fan T, Zhao X, et al (2022) Simplified classification of cavernous internal carotid artery tortuosity: a predictor of procedural complexity and clinical outcomes in mechanical thrombectomy. Neurol Res 1–9. https://doi.org/10.1080/01616412.2022.2068851
Wang H-F, Wang D-M, Wang J-J et al (2017) Extracranial internal carotid artery tortuosity and body mass index. Front Neurol 8:508. https://doi.org/10.3389/fneur.2017.00508
Snelling BM, Sur S, Shah SS et al (2018) Unfavorable vascular anatomy is associated with increased revascularization time and worse outcome in anterior circulation thrombectomy. World Neurosurgery 120:e976–e983. https://doi.org/10.1016/j.wneu.2018.08.207
Kargman DE, Tuck C, Berglund L et al (1998) Lipid and lipoprotein levels remain stable in acute ischemic stroke: the Northern Manhattan Stroke Study. Atherosclerosis 139:391–399. https://doi.org/10.1016/S0021-9150(98)00085-9
Konopka A, Chodkowska E, Piotrowski W, Stepińska J (2004) Is the assessment of lipid profile performed up to seventy two hours from hospital admission due to acute coronary syndrome still valid? Kardiol Pol 61:243–250
Effect of balloon guide catheter on clinical outcomes and reperfusion in Trevo thrombectomy | Journal of NeuroInterventional Surgery. https://jnis.bmj.com/content/11/9/861.long. Accessed 6 Mar 2023
Balloon guide catheter improves revascularization and clinical outcomes with the solitaire device | Stroke. https://www.ahajournals.org/doi/10.1161/STROKEAHA.113.002407?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed . Accessed 6 Mar 2023
Funding
This study was supported by the Natural Science Foundation of Guangdong Province, China (NO. 2022A1515012191). Xiaodong Cai received the grant.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
T. Nguyen reports research support from Medtronic and the Society of Vascular and Interventional Neurology. The authors declare that they have no conflicts of interest and no competing interest.
Ethics approval
This single-center retrospective cohort study was approved by the ethics committee of the First People’s Hospital of Kashi Prefecture, Affiliated Kashi Hospital of Sun Yat-Sen University, Kashi China.
Informed consent
Patient informed consent was waived due to the retrospective study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Junliu Zhang, Ling Long, Jie Li and Heng Zhang contributed equally to the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, J., Long, L., Li, J. et al. Impact of obesity-related indicators on first-pass effect in patients with ischemic stroke receiving mechanical thrombectomy. Neuroradiology (2024). https://doi.org/10.1007/s00234-024-03350-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00234-024-03350-x