Abstract
Purpose
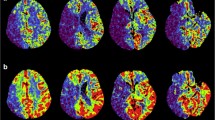
Endovascular treatment (EVT) of acute ischemic stroke can be complicated by vessel perforation. We studied the incidence and determinants of vessel perforations. In addition, we studied the association of vessel perforations with functional outcome, and the association between location of perforation on digital subtraction angiography (DSA) and functional outcome, using a large EVT registry.
Methods
We included all patients in the MR CLEAN Registry who underwent EVT. We used DSA to determine whether EVT was complicated by a vessel perforation. We analyzed the association with baseline clinical and interventional parameters using logistic regression models. Functional outcome was measured using the modified Rankin Scale at 90 days. The association between vessel perforation and angiographic imaging features and functional outcome was studied using ordinal logistic regression models adjusted for prognostic parameters. These associations were expressed as adjusted common odds ratios (acOR).
Results
Vessel perforation occurred in 74 (2.6%) of 2794 patients who underwent EVT. Female sex (aOR 2.0 (95% CI 1.2–3.2)) and distal occlusion locations (aOR 2.2 (95% CI 1.3–3.5)) were associated with increased risk of vessel perforation. Functional outcome was worse in patients with vessel perforation (acOR 0.38 (95% CI 0.23–0.63)) compared to patients without a vessel perforation. No significant association was found between location of perforation and functional outcome.
Conclusion
The incidence of vessel perforation during EVT in this cohort was low, but has severe clinical consequences. Female patients and patients treated at distal occlusion locations are at higher risk.


Similar content being viewed by others
Data availability
The datasets created in this study can be obtained from the corresponding author upon reasonable request. Additionally, the datasets analyzed in this study can be requested from the MR CLEAN trial office at mrclean@erasmusmc.nl.
Abbreviations
- A1-A2-A3:
-
Segment of anterior cerebral artery
- DSA:
-
Digital subtraction angiography
- EVT:
-
Endovascular thrombectomy
- eTICI:
-
Extended Treatment In Cerebral Ischemia score
- ICA:
-
Internal carotid artery
- IVT:
-
Intravenous thrombolysis
- M1-M2-M3:
-
M1-M2-M3 segment of middle cerebral artery
- mRS:
-
Modified Rankin Scale
- NIHSS:
-
National Institutes of Health Stroke Scale
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387(10029):1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Happi Ngankou E, Gory B, Marnat G, Richard S, Bourcier R, Sibon I et al (2021) Thrombectomy complications in large vessel occlusions: incidence, predictors, and clinical impact in the ETIS Registry. Stroke 52(12):e764–e768. https://doi.org/10.1161/STROKEAHA.121.034865
Salsano G, Pracucci G, Mavilio N, Saia V, Bandettini di Poggio M, Malfatto L et al (2021) Complications of mechanical thrombectomy for acute ischemic stroke: incidence, risk factors, and clinical relevance in the Italian registry of endovascular treatment in acute stroke. Int J Stroke 16(7):818–27. https://doi.org/10.1177/1747493020976681
Mokin M, Fargen KM, Primiani CT, Ren Z, Dumont TM, Brasiliense LBC et al (2017) Vessel perforation during stent retriever thrombectomy for acute ischemic stroke: technical details and clinical outcomes. J Neurointerv Surg 9(10):922–928. https://doi.org/10.1136/neurintsurg-2016-012707
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372(1):11–20. https://doi.org/10.1056/NEJMoa1411587
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372(24):2285–95. https://doi.org/10.1056/NEJMoa1415061
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372(11):1009–1018. https://doi.org/10.1056/NEJMoa1414792
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372(24):2296–2306. https://doi.org/10.1056/NEJMoa1503780
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372(11):1019–1030. https://doi.org/10.1056/NEJMoa1414905
Ducroux C, Boisseau W, Poppe AY, Daneault N, Deschaintre Y, Diestro JDB et al (2022) Successful reperfusion is associated with favorable functional outcome despite vessel perforation during thrombectomy: a case series and systematic review. AJNR Am J Neuroradiol 43(11):1633–1638. https://doi.org/10.3174/ajnr.A7650
Schulze-Zachau V, Brehm A, Ntoulias N, Krug N, Tsogkas I, Blackham KA et al (2023) Incidence and outcome of perforations during medium vessel occlusion compared with large vessel occlusion thrombectomy. J Neurointerv Surg. https://doi.org/10.1136/jnis-2023-020531
Jansen IGH, Mulder M, Goldhoorn RB, investigators MCR (2018) Endovascular treatment for acute ischaemic stroke in routine clinical practice: prospective, observational cohort study (MR CLEAN Registry). BMJ 360:949. https://doi.org/10.1136/bmj.k949
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Goyal M, Fargen KM, Turk AS, Mocco J, Liebeskind DS, Frei D et al (2014) 2C or not 2C: defining an improved revascularization grading scale and the need for standardization of angiography outcomes in stroke trials. J Neurointerv Surg 6(2):83–86. https://doi.org/10.1136/neurintsurg-2013-010665
Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES Jr et al (2006) Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery 59(1):21–7. https://doi.org/10.1227/01.neu.0000243277.86222.6c. (discussion -7)
Bamford JM, Sandercock PA, Warlow CP, Slattery J (1989) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 20(6):828. https://doi.org/10.1161/01.str.20.6.828
Venema E, Roozenbeek B, Mulder M, Brown S, Majoie C, Steyerberg EW et al (2021) Prediction of outcome and endovascular treatment benefit: validation and update of the MR PREDICTS decision tool. Stroke 52(9):2764–2772. https://doi.org/10.1161/STROKEAHA.120.032935
van Buuren S, Groothuis-Oudshoorn K (2011) mice: multivariate imputation by chained equations in R. J Stat Soft 45(3):1–67. https://doi.org/10.18637/jss.v045.i03
Team RC (2021) R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing
Minnerup J, Wersching H, Teuber A, Wellmann J, Eyding J, Weber R et al (2016) Outcome after thrombectomy and intravenous thrombolysis in patients with acute ischemic stroke: a prospective observational study. Stroke 47(6):1584–1592. https://doi.org/10.1161/STROKEAHA.116.012619
Keulers A, Nikoubashman O, Mpotsaris A, Wilson SD, Wiesmann M (2019) Preventing vessel perforations in endovascular thrombectomy: feasibility and safety of passing the clot with a microcatheter without microwire: the wireless microcatheter technique. J Neurointerv Surg 11(7):653–658. https://doi.org/10.1136/neurintsurg-2018-014267
Morkos K, Maingard J, Barras C, Kok HK, Hall J, Russell J et al (2023) Tranexamic acid as a novel adjunct in the management of vessel perforation complicating Endovascular Clot Retrieval. J Stroke Cerebrovasc Dis 32(6):107067. https://doi.org/10.1016/j.jstrokecerebrovasdis.2023.107067
Maslias E, Puccinelli F, Nannoni S, Hajdu SD, Bartolini B, Ricciardi F et al (2022) Predictors of endovascular treatment procedural complications in acute ischemic stroke: a single-center cohort study. AJNR Am J Neuroradiol 43(12):1743–1748. https://doi.org/10.3174/ajnr.A7705
Harteveld AA, Denswil NP, Van Hecke W, Kuijf HJ, Vink A, Spliet WGM et al (2018) Data on vessel wall thickness measurements of intracranial arteries derived from human circle of Willis specimens. Data Brief 19:6–12. https://doi.org/10.1016/j.dib.2018.04.116
Shatri J, Bexheti D, Bexheti S, Kabashi S, Krasniqi S, Ahmetgjekaj I et al (2017) Influence of gender and age on average dimensions of arteries forming the circle of Willis study by magnetic resonance angiography on Kosovo’s population. Open Access Maced J Med Sci 5(6):714–719. https://doi.org/10.3889/oamjms.2017.160
Cogswell PM, Lants SK, Davis LT, Donahue MJ (2019) Vessel wall and lumen characteristics with age in healthy participants using 3T intracranial vessel wall magnetic resonance imaging. J Magn Reson Imaging 50(5):1452–1460. https://doi.org/10.1002/jmri.26750
Zurada A, Gielecki J, Tubbs RS, Loukas M, Maksymowicz W, Cohen-Gadol AA et al (2011) Three-dimensional morphometrical analysis of the M1 segment of the middle cerebral artery: potential clinical and neurosurgical implications. Clin Anat 24(1):34–46. https://doi.org/10.1002/ca.21051
Pilgram-Pastor SM, Piechowiak EI, Dobrocky T, Kaesmacher J, Den Hollander J, Gralla J et al (2021) Stroke thrombectomy complication management. J Neurointerv Surg 13(10):912–917. https://doi.org/10.1136/neurintsurg-2021-017349
Xu H, Guan S, Liu C, Wang L, Yan B, Han H et al (2019) Rescue glue embolization of vessel perforation during mechanical thrombectomy for acute ischemic stroke: technical note. World Neurosurg 121:19–23. https://doi.org/10.1016/j.wneu.2018.09.131
Carpenter DA, Grubb RL Jr, Tempel LW, Powers WJ (1991) Cerebral oxygen metabolism after aneurysmal subarachnoid hemorrhage. J Cereb Blood Flow Metab 11(5):837–844. https://doi.org/10.1038/jcbfm.1991.143
Vergouwen MD, Ilodigwe D, Macdonald RL (2011) Cerebral infarction after subarachnoid hemorrhage contributes to poor outcome by vasospasm-dependent and-independent effects. Stroke 42(4):924–929. https://doi.org/10.1161/STROKEAHA.110.597914
Dankbaar JW, Rijsdijk M, van der Schaaf IC, Velthuis BK, Wermer MJ, Rinkel GJ (2009) Relationship between vasospasm, cerebral perfusion, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neuroradiology 51(12):813–819. https://doi.org/10.1007/s00234-009-0575-y
Halbach VV, Higashida RT, Dowd CF, Barnwell SL, Hieshima GB (1991) Management of vascular perforations that occur during neurointerventional procedures. AJNR Am J Neuroradiol 12(2):319–327
Ryu CW, Lee CY, Koh JS, Choi SK, Kim EJ (2011) Vascular perforation during coil embolization of an intracranial aneurysm: the incidence, mechanism, and clinical outcome. Neurointervention 6(1):17–22. https://doi.org/10.5469/neuroint.2011.6.1.17
Akpinar SH, Yilmaz G (2016) Periprocedural complications in endovascular stroke treatment. Br J Radiol 89(1057):20150267. https://doi.org/10.1259/bjr.20150267
Yi T, Chen W, Wu Y, Pan Z, Lin X, Lin D et al (2022) Intra-arterial injection of thrombin as rescue therapy of vessel perforation during mechanical thrombectomy for acute ischemic stroke. Brain Sci 12(6):760. https://doi.org/10.3390/brainsci12060760
Suzuki K, Matsumaru Y, Takeuchi M, Morimoto M, Kanazawa R, Takayama Y et al (2021) Effect of mechanical thrombectomy without vs with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke: the SKIP randomized clinical trial. JAMA 325(3):244–253. https://doi.org/10.1001/jama.2020.23522
LeCouffe NE, Kappelhof M, Treurniet KM, Rinkel LA, Bruggeman AE, Berkhemer OA et al (2021) A randomized trial of intravenous alteplase before endovascular treatment for stroke. N Engl J Med 385(20):1833–1844. https://doi.org/10.1056/NEJMoa2107727
van der Steen W, van de Graaf RA, Chalos V, Lingsma HF, van Doormaal PJ, Coutinho JM et al (2022) Safety and efficacy of aspirin, unfractionated heparin, both, or neither during endovascular stroke treatment (MR CLEAN-MED): an open-label, multicentre, randomised controlled trial. Lancet. https://doi.org/10.1016/S0140-6736(22)00014-9
Lapergue B, Blanc R, Costalat V, Desal H, Saleme S, Spelle L et al (2021) Effect of thrombectomy with combined contact aspiration and stent retriever vs stent retriever alone on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER2 randomized clinical trial. JAMA 326(12):1158–1169. https://doi.org/10.1001/jama.2021.13827
Renu A, Millan M, San Roman L, Blasco J, Marti-Fabregas J, Terceno M et al (2022) Effect of intra-arterial alteplase vs placebo following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke: the CHOICE randomized clinical trial. JAMA 327(9):826–835. https://doi.org/10.1001/jama.2022.1645
Menon BK, Buck BH, Singh N, Deschaintre Y, Almekhlafi MA, Coutts SB et al (2022) Intravenous tenecteplase compared with alteplase for acute ischaemic stroke in Canada (AcT): a pragmatic, multicentre, open-label, registry-linked, randomised, controlled, non-inferiority trial. Lancet 400(10347):161–169. https://doi.org/10.1016/S0140-6736(22)01054-6
Olthuis SGH, Pirson FAV, Pinckaers FME, Hinsenveld WH, Nieboer D, Ceulemans A et al (2023) Endovascular treatment versus no endovascular treatment after 6–24 h in patients with ischaemic stroke and collateral flow on CT angiography (MR CLEAN-LATE) in the Netherlands: a multicentre, open-label, blinded-endpoint, randomised, controlled, phase 3 trial. Lancet. https://doi.org/10.1016/S0140-6736(23)00575-5
Almekhlafi M, Ospel JM, Saposnik G, Kashani N, Demchuk A, Hill MD et al (2020) Endovascular treatment decisions in patients with M2 segment MCA occlusions. AJNR Am J Neuroradiol 41(2):280–285. https://doi.org/10.3174/ajnr.A6397
Acknowledgements
We thank the MR CLEAN Registry investigators for their contribution. A list of all investigators is given in the supplement material.
Funding
The MR CLEAN Registry was partly funded by TWIN Foundation, Erasmus MC University Medical Center, Maastricht University Medical Center, and Amsterdam UMC. Erasmus MC received funds from Stryker® by DD, AvdL, and Bracco Imaging® by DD. Amsterdam UMC received funds from Stryker® for consultations by CM, YR, and OB. MUMC received funds from Stryker® and Codman® for consultations by WZ. The current work on clinical consequence of vessel perforations was supported by Health-Holland (TKI Life Sciences and Health) through the Q-Maestro project under Grant EMCLSH19006 and Philips Healthcare (Best, The Netherlands).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethics approval
The central medical ethics committee of the Erasmus MC University Medical Center, Rotterdam, the Netherlands, evaluated the study protocol and granted permission to carry out the study as a registry (MEC-2014–235).
Consent to participate
All patients or their legal representatives provided written informed consent.
Conflict of interest
P. Matthijs van der Sluijs — no conflict of interest.
R. Su — no conflict of interest.
S.A.P. Cornelissen — no conflict of interest.
A.C.G.M. van Es — no conflict of interest.
G. Lycklama a Nijeholt — no conflict of interest.
B. Roozenbeek — no conflict of interest.
P.J. van Doormaal — no conflict of interest.
J. Hofmeijer — no conflict of interest.
A. van der Lugt — no conflict of interest.
T. van Walsum — no conflict of interest.
Standards of reporting
This study is reported in accordance with the STROBE guidelines (Strengthening the Reporting of Observational Studies in Epidemiology).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Full list of contributors is listed in the supplemental appendix.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
MR CLEAN Registry Investigators — group authors
Executive committee
Diederik W.J. Dippel1; Aad van der Lugt2; Charles B.L.M. Majoie3; Yvo B.W.E.M. Roos4; Robert J. van Oostenbrugge5,41; Wim H. van Zwam6,41; Jelis Boiten14; Jan Albert Vos8
Study coordinators
Ivo G.H. Jansen3; Maxim J.H.L. Mulder1,2; Robert- Jan B. Goldhoorn5,6,41; Kars C.J. Compagne2; Manon Kappelhof3; Josje Brouwer4; Sanne J. den Hartog1,2,40; Wouter H. Hinsenveld5,6
Local principal investigators
Diederik W.J. Dippel1; Bob Roozenbeek1; Aad van der Lugt2; Adriaan C.G.M. van Es2; Charles B.L.M. Majoie3; Yvo B.W.E.M. Roos4; Bart J. Emmer3; Jonathan M. Coutinho4; Wouter J. Schonewille7; Jan Albert Vos8; Marieke J.H. Wermer9; Marianne A.A. van Walderveen10; Julie Staals5,41; Robert J. van Oostenbrugge5,41; Wim H. van Zwam6,41; Jeannette Hofmeijer11; Jasper M. Martens12; Geert J. Lycklama à Nijeholt13; Jelis Boiten14; Sebastiaan F. de Bruijn15; Lukas C. van Dijk16; H. Bart van der Worp17; Rob H. Lo18; Ewoud J. van Dijk19; Hieronymus D. Boogaarts20; J. de Vries22; Paul L.M. de Kort21; Julia van Tuijl21; Jo P. Peluso26; Puck Fransen22; Jan S.P. van den Berg22; Boudewijn A.A.M. van Hasselt23; Leo A.M. Aerden24; René J. Dallinga25; Maarten Uyttenboogaart28; Omid Eschgi29; Reinoud P.H. Bokkers29; Tobien H.C.M.L. Schreuder30; Roel J.J. Heijboer31; Koos Keizer32; Lonneke S.F. Yo33; Heleen M. den Hertog22; Tomas Bulut35; Paul J.A.M. Brouwers34
Imaging assessment committee
Charles B.L.M. Majoie3 (chair); Wim H. van Zwam6,41; Aad van der Lugt2; Geert J. Lycklama à Nijeholt13; Marianne A.A. van Walderveen10; Marieke E.S. Sprengers3; Sjoerd F.M. Jenniskens27; René van den Berg3; Albert J. Yoo38; Ludo F.M. Beenen3; Alida A. Postma6,42; Stefan D. Roosendaal3; Bas F.W. van der Kallen13; Ido R. van den Wijngaard13; Adriaan C.G.M. van Es2; Bart J. Emmer,3; Jasper M. Martens12; Lonneke S.F. Yo33; Jan Albert Vos8; Joost Bot36; Pieter-Jan van Doormaal2; Anton Meijer27; Elyas Ghariq13; Reinoud P.H. Bokkers29; Marc P. van Proosdij37; G. Menno Krietemeijer33; Jo P. Peluso26; Hieronymus D. Boogaarts20; Rob Lo18; Wouter Dinkelaar2; Auke P.A. Appelman29; Bas Hammer16; Sjoert Pegge27; Anouk van der Hoorn29; Saman Vinke20
Writing committee
Diederik W.J. Dippel1 (chair); Aad van der Lugt2; Charles B.L.M. Majoie3; Yvo B.W.E.M. Roos4; Robert J. van Oostenbrugge5,41; Wim H. van Zwam6,41; Geert J. Lycklama à Nijeholt13; Jelis Boiten14; Jan Albert Vos8; Wouter J. Schonewille7; Jeannette Hofmeijer11; Jasper M. Martens12; H. Bart van der Worp17; Rob H. Lo18
Adverse event committee
Robert J. van Oostenbrugge5,41 (chair); Jeannette Hofmeijer11; H. Zwenneke Flach23
Trial methodologist
Hester F. Lingsma40
Research nurses/local trial coordinators
Naziha el Ghannouti1; Martin Sterrenberg1; Wilma Pellikaan7; Rita Sprengers4; Marjan Elfrink11; Michelle Simons11; Marjolein Vossers12; Joke de Meris14; Tamara Vermeulen14; Annet Geerlings19; Gina van Vemde22; Tiny Simons30; Gert Messchendorp28; Nynke Nicolaij28; Hester Bongenaar32; Karin Bodde24; Sandra Kleijn34; Jasmijn Lodico34; Hanneke Droste34; Maureen Wollaert5; Sabrina Verheesen5; D. Jeurrissen5; Erna Bos9; Yvonne Drabbe15; Michelle Sandiman15; Nicoline Aaldering11; Berber Zweedijk17; Jocova Vervoort21; Eva Ponjee22; Sharon Romviel19; Karin Kanselaar19; Denn Barning10
PhD/Medical students
Esmee Venema40; Vicky Chalos1,40; Ralph R. Geuskens3; Tim van Straaten19; Saliha Ergezen1; Roger R.M. Harmsma1; Daan Muijres1; Anouk de Jong1; Olvert A. Berkhemer1,3,6; Anna M.M. Boers3,39; J. Huguet3; P.F.C. Groot3; Marieke A. Mens3; Katinka R. van Kranendonk3; Kilian M. Treurniet3; Manon L. Tolhuisen3,39; Heitor Alves3; Annick J. Weterings3; Eleonora L.F. Kirkels3; Eva J.H.F. Voogd11; Lieve M. Schupp3; Sabine L. Collette28,29; Adrien E.D. Groot4; Natalie E. LeCouffe4; Praneeta R. Konduri39; Haryadi Prasetya39; Nerea Arrarte-Terreros39; Lucas A. Ramos39
List of affiliations
Department of Neurology1, Radiology2, Public Health40, Erasmus MC University Medical Center;
Department of Radiology and Nuclear Medicine3, Neurology4, Biomedical Engineering & Physics39, Amsterdam UMC, location University of Amsterdam;
Department of Neurology5, Radiology & Nuclear Medicine6, Maastricht University Medical Center; School for Cardiovascular Diseases Maastricht (CARIM)41; and MHeNs School for Mental Health and Neuroscience, Maastricht, the Netherlands42;
Department of Neurology7, Radiology8, Sint Antonius Hospital, Nieuwegein;
Department of Neurology9, Radiology10, Leiden University Medical Center;
Department of Neurology11, Radiology12, Rijnstate Hospital, Arnhem;
Department of Radiology13, Neurology14, Haaglanden MC, the Hague;
Department of Neurology15, Radiology16, HAGA Hospital, the Hague;
Department of Neurology17, Radiology18, University Medical Center Utrecht;
Department of Neurology19, Neurosurgery20, Radiology27, Radboud University Medical Center, Nijmegen;
Department of Neurology21, Radiology26, Elisabeth-TweeSteden ziekenhuis, Tilburg;
Department of Neurology22, Radiology23, Isala Klinieken, Zwolle;
Department of Neurology24, Radiology25, Reinier de Graaf Gasthuis, Delft;
Department of Neurology28, Radiology29, University Medical Center Groningen;
Department of Neurology30, Radiology31, Atrium Medical Center, Heerlen;
Department of Neurology32, Radiology33, Catharina Hospital, Eindhoven;
Department of Neurology34, Radiology35, Medisch Spectrum Twente, Enschede;
Department of Radiology36, Amsterdam UMC, Vrije Universiteit van Amsterdam, Amsterdam;
Department of Radiology37, Noordwest Ziekenhuisgroep, Alkmaar;
Department of Radiology38, Texas Stroke Institute, TX, USA.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van der Sluijs, P., Su, R., Cornelissen, S.A. et al. Clinical consequence of vessel perforations during endovascular treatment of acute ischemic stroke. Neuroradiology 66, 237–247 (2024). https://doi.org/10.1007/s00234-023-03246-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-023-03246-2