Abstract
Purpose
Sex differences in Alzheimer’s disease (AD) progression provide clues to pathogenesis and better patient management. We examined sex differences in emotional memory among AD patients, amnestic mild cognitive impairment (aMCI) patients, and healthy controls (HCs) as well as potential associations with altered regional cerebral blood flow (rCBF).
Methods
The recognition memory task with emotional pictures was applied to evaluate enhancement of emotional memory (EEM) and 3D pseudo-continuous arterial spin labeling MRI was performed to measure the rCBF in 74 AD patients (41 females), 74 aMCI patients (45 females), and 74 HCs (43 females). Group differences in EEM were tested by two-way analysis of covariance (ANCOVA) with repeated measures. The main effects of clinical group and sex as well as group × sex interactions on rCBF were assessed by two-way ANCOVA. Correlation analyses were conducted to investigate associations between EEM and rCBF.
Results
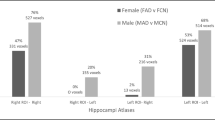
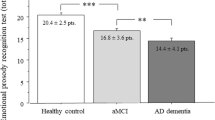
With disease progression, EEM gradually disappeared. Among aMCI patients, females exhibited a greater index of recollection (Pr) for positive/high-arousal and negative/low-arousal pictures versus neutral pictures (P = 0.005, P = 0.003), while males exhibited a greater Pr for negative/high-arousal versus neutral pictures (P = 0.001). There were significant sex × group effects on rCBF in left inferior parietal, supramarginal, superior temporal and middle temporal gyri, and rCBF of left inferior parietal gyrus was correlated with Pr for positive/high-arousal pictures among female aMCI patients (r = 0.584, q = 0.005).
Conclusion
Males and females exhibit distinct changes in EEM associated with altered rCBF, which should be considered in future neuroimaging studies.






Similar content being viewed by others
References
Marfany A, Sierra C, Camafort M, Domenech M, Coca A (2018) High blood pressure, Alzheimer disease and antihypertensive treatment. Panminerva Med 60(1):8–16. https://doi.org/10.23736/S0031-0808.18.03360-8
Mrdjen D, Fox EJ, Bukhari SA, Montine KS, Bendall SC, Montine TJ (2019) The basis of cellular and regional vulnerability in Alzheimer’s disease. Acta Neuropathol 138(5):729–749. https://doi.org/10.1007/s00401-019-02054-4
Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chetelat G, Teunissen CE, Cummings J, van der Flier WM (2021) Alzheimer’s disease. Lancet 397(10284):1577–1590. https://doi.org/10.1016/S0140-6736(20)32205-4
Gozdas E, Fingerhut H, Chromik LC, O’Hara R, Reiss AL, Hosseini SMH (2020) Focal white matter disruptions along the cingulum tract explain cognitive decline in amnestic mild cognitive impairment (aMCI). Sci Rep 10(1):10213. https://doi.org/10.1038/s41598-020-66796-y
Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L (2014) Mild cognitive impairment: a concept in evolution. J Intern Med 275(3):214–228. https://doi.org/10.1111/joim.12190
LaBar KS, Cabeza R (2006) Cognitive neuroscience of emotional memory. Nat Rev Neurosci 7(1):54–64. https://doi.org/10.1038/nrn1825
Hamann S (2001) Cognitive and neural mechanisms of emotional memory. Trends Cogn Sci 5(9):394–400. https://doi.org/10.1016/s1364-6613(00)01707-1
Kazui H, Mori E, Hashimoto M, Hirono N (2003) Enhancement of declarative memory by emotional arousal and visual memory function in Alzheimer’s disease. J Neuropsychiatry Clin Neurosci 15(2):221–226. https://doi.org/10.1176/jnp.15.2.221
Chainay H, Sava A, Michael GA, Landre L, Versace R, Krolak-Salmon P (2014) Impaired emotional memory enhancement on recognition of pictorial stimuli in Alzheimer’s disease: no influence of the nature of encoding. Cortex 50:32–44. https://doi.org/10.1016/j.cortex.2013.10.001
Hamann SB, Monarch ES, Goldstein FC (2000) Memory enhancement for emotional stimuli is impaired in early Alzheimer’s disease. Neuropsychology 14(1):82–92
Sava AA, Paquet C, Krolak-Salmon P, Dumurgier J, Hugon J, Chainay H (2015) Emotional memory enhancement in respect of positive visual stimuli in Alzheimer’s disease emerges after rich and deep encoding. Cortex 65:89–101. https://doi.org/10.1016/j.cortex.2015.01.002
Boller F, El Massioui F, Devouche E, Traykov L, Pomati S, Starkstein SE (2002) Processing emotional information in Alzheimer’s disease: effects on memory performance and neurophysiological correlates. Dement Geriatr Cogn Disord 14(2):104–112. https://doi.org/10.1159/000064932
Klein-Koerkamp Y, Baciu M, Hot P (2012) Preserved and impaired emotional memory in Alzheimer’s disease. Front Psychol 3:331. https://doi.org/10.3389/fpsyg.2012.00331
Niu H, Alvarez-Alvarez I, Guillen-Grima F, Aguinaga-Ontoso I (2017) Prevalence and incidence of Alzheimer’s disease in Europe: a meta-analysis. Neurologia 32(8):523–532. https://doi.org/10.1016/j.nrl.2016.02.016
Buckley RF, Mormino EC, Amariglio RE, Properzi MJ, Rabin JS, Lim YY, Papp KV, Jacobs HIL, Burnham S, Hanseeuw BJ, Dore V, Dobson A, Masters CL, Waller M, Rowe CC, Maruff P, Donohue MC, Rentz DM, Kirn D, Hedden T, Chhatwal J, Schultz AP, Johnson KA, Villemagne VL, Sperling RA, Alzheimer’s disease neuroimaging i, australian imaging B, Lifestyle study of a, Harvard Aging Brain S (2018) Sex, amyloid, and APOE epsilon4 and risk of cognitive decline in preclinical Alzheimer’s disease: findings from three well-characterized cohorts. Alzheimers Dement 14(9):1193–1203. https://doi.org/10.1016/j.jalz.2018.04.010
Oveisgharan S, Arvanitakis Z, Yu L, Farfel J, Schneider JA, Bennett DA (2018) Sex differences in Alzheimer’s disease and common neuropathologies of aging. Acta Neuropathol 136(6):887–900. https://doi.org/10.1007/s00401-018-1920-1
Lacalle-Aurioles M, Mateos-Perez JM, Guzman-De-Villoria JA, Olazaran J, Cruz-Orduna I, Aleman-Gomez Y, Martino ME, Desco M (2014) Cerebral blood flow is an earlier indicator of perfusion abnormalities than cerebral blood volume in Alzheimer’s disease. J Cereb Blood Flow Metab 34(4):654–659. https://doi.org/10.1038/jcbfm.2013.241
Hays CC, Zlatar ZZ, Wierenga CE (2016) The utility of cerebral blood flow as a biomarker of preclinical Alzheimer’s disease. Cell Mol Neurobiol 36(2):167–179. https://doi.org/10.1007/s10571-015-0261-z
Fazlollahi A, Calamante F, Liang X, Bourgeat P, Raniga P, Dore V, Fripp J, Ames D, Masters CL, Rowe CC, Connelly A, Villemagne VL, Salvado O, Australian Imaging B, Lifestyle Research G (2020) Increased cerebral blood flow with increased amyloid burden in the preclinical phase of alzheimer’s disease. J Magn Reson Imaging. 51(2):505–513. https://doi.org/10.1002/jmri.26810
Bron EE, Steketee RM, Houston GC, Oliver RA, Achterberg HC, Loog M, van Swieten JC, Hammers A, Niessen WJ, Smits M, Klein S, Alzheimer’s disease neuroimaging I (2014) Diagnostic classification of arterial spin labeling and structural MRI in presenile early stage dementia. Hum Brain Mapp 35(9):4916–4931. https://doi.org/10.1002/hbm.22522
Binnewijzend MA, Benedictus MR, Kuijer JP, van der Flier WM, Teunissen CE, Prins ND, Wattjes MP, van Berckel BN, Scheltens P, Barkhof F (2016) Cerebral perfusion in the predementia stages of Alzheimer’s disease. Eur Radiol 26(2):506–514. https://doi.org/10.1007/s00330-015-3834-9
Ding B, Ling HW, Zhang Y, Huang J, Zhang H, Wang T, Yan FH (2014) Pattern of cerebral hyperperfusion in Alzheimer’s disease and amnestic mild cognitive impairment using voxel-based analysis of 3D arterial spin-labeling imaging: initial experience. Clin Interv Aging 9:493–500. https://doi.org/10.2147/CIA.S58879
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):263–269. https://doi.org/10.1016/j.jalz.2011.03.005
Dubois B, Feldman HH, Jacova C, Dekosky ST, Barberger-Gateau P, Cummings J, Delacourte A, Galasko D, Gauthier S, Jicha G, Meguro K, O’Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Stern Y, Visser PJ, Scheltens P (2007) Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 6(8):734–746. https://doi.org/10.1016/S1474-4422(07)70178-3
Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J Intern Med 256(3):183–194. https://doi.org/10.1111/j.1365-2796.2004.01388.x
Li X, Li X, Chen S, Zhu J, Wang H, Tian Y, Yu Y (2020) Effect of emotional enhancement of memory on recollection process in young adults: the influence factors and neural mechanisms. Brain Imaging Behav 14(1):119–129. https://doi.org/10.1007/s11682-018-9975-0
Forster KI, Forster JC (2003) DMDX: a windows display program with millisecond accuracy. Behav Res Methods Instrum Comput 35(1):116–124. https://doi.org/10.3758/bf03195503
Ashburner J (2007) A fast diffeomorphic image registration algorithm. Neuroimage 38(1):95–113. https://doi.org/10.1016/j.neuroimage.2007.07.007
Haller S, Zaharchuk G, Thomas DL, Lovblad KO, Barkhof F, Golay X (2016) Arterial spin labeling perfusion of the brain: emerging clinical applications. Radiology 281(2):337–356. https://doi.org/10.1148/radiol.2016150789
Xu G, Rowley HA, Wu G, Alsop DC, Shankaranarayanan A, Dowling M, Christian BT, Oakes TR, Johnson SC (2010) Reliability and precision of pseudo-continuous arterial spin labeling perfusion MRI on 3.0 T and comparison with 15O-water PET in elderly subjects at risk for Alzheimer’s disease. NMR Biomed 23(3):286–293. https://doi.org/10.1002/nbm.1462
Aslan S, Lu H (2010) On the sensitivity of ASL MRI in detecting regional differences in cerebral blood flow. Magn Reson Imaging 28(7):928–935. https://doi.org/10.1016/j.mri.2010.03.037
Liu Y, Zeng X, Wang Z, Zhang N, Fan D, Yuan H (2015) Different post label delay cerebral blood flow measurements in patients with Alzheimer’s disease using 3D arterial spin labeling. Magn Reson Imaging 33(9):1019–1025. https://doi.org/10.1016/j.mri.2015.05.001
Preuss D, Schoofs D, Wolf OT (2009) Associations between endogenous cortisol levels and emotional memory in young women: influence of encoding instructions. Stress 12(5):379–387. https://doi.org/10.1080/10253890802524592
McGaugh JL, Roozendaal B (2002) Role of adrenal stress hormones in forming lasting memories in the brain. Curr Opin Neurobiol 12(2):205–210. https://doi.org/10.1016/s0959-4388(02)00306-9
Chao LL, Haxby JV, Martin A (1999) Attribute-based neural substrates in temporal cortex for perceiving and knowing about objects. Nat Neurosci 2(10):913–919. https://doi.org/10.1038/13217
Herath P, Kinomura S, Roland PE (2001) Visual recognition: evidence for two distinctive mechanisms from a PET study. Hum Brain Mapp 12(2):110–119. https://doi.org/10.1002/1097-0193(200102)12:2%3c110::aid-hbm1008%3e3.0.co;2-0
Kark SM, Kensinger EA (2015) Effect of emotional valence on retrieval-related recapitulation of encoding activity in the ventral visual stream. Neuropsychologia 78:221–230. https://doi.org/10.1016/j.neuropsychologia.2015.10.014
Li R, Zhang Y, Zhuo Z, Wang Y, Jia Z, Sun M, Zhang Y, Li W, Duan Y, Yao Z, Weng H, Wei J, Liu Y, Xu J (2021) Altered cerebral blood flow in Alzheimer’s disease with depression. Front Psychiatry 12:687739. https://doi.org/10.3389/fpsyt.2021.687739
Nomura T, Kirimoto H (2018) Anodal transcranial direct current stimulation over the supplementary motor area improves anticipatory postural adjustments in older adults. Front Hum Neurosci 12:317. https://doi.org/10.3389/fnhum.2018.00317
Herrero MT, Barcia C, Navarro JM (2002) Functional anatomy of thalamus and basal ganglia. Child’s Nerv Syst 18(8):386–404. https://doi.org/10.1007/s00381-002-0604-1
Cirak M, Yagmurlu K, Kearns KN, Ribas EC, Urgun K, Shaffrey ME, Kalani MYS (2020) The caudate nucleus: its connections, surgical implications, and related complications. World Neurosurg 139:e428–e438. https://doi.org/10.1016/j.wneu.2020.04.027
Wirth M, PichetBinette A, Brunecker P, Kobe T, Witte AV, Floel A (2017) Divergent regional patterns of cerebral hypoperfusion and gray matter atrophy in mild cognitive impairment patients. J Cereb Blood Flow Metab 37(3):814–824. https://doi.org/10.1177/0271678X16641128
Kensinger EA (2008) Age differences in memory for arousing and nonarousing emotional words. J Gerontol B Psychol Sci Soc Sci 63(1):P13-18. https://doi.org/10.1093/geronb/63.1.p13
Nieuwenhuis-Mark RE, Schalk K, de Graaf N (2009) Free recall and learning of emotional word lists in very elderly people with and without dementia. Am J Alzheimers Dis Other Demen 24(2):155–162. https://doi.org/10.1177/1533317508330561
Collignon O, Girard S, Gosselin F, Saint-Amour D, Lepore F, Lassonde M (2010) Women process multisensory emotion expressions more efficiently than men. Neuropsychologia 48(1):220–225. https://doi.org/10.1016/j.neuropsychologia.2009.09.007
Carstensen LL, Isaacowitz DM, Charles ST (1999) Taking time seriously. A theory of socioemotional selectivity. Am Psychol 54(3):165–181. https://doi.org/10.1037//0003-066x.54.3.165
Koran MEI, Wagener M, Hohman TJ, Alzheimer’s Neuroimaging I (2017) Sex differences in the association between AD biomarkers and cognitive decline. Brain Imaging Behav 11(1):205–213. https://doi.org/10.1007/s11682-016-9523-8
Small GW, Kuhl DE, Riege WH, Fujikawa DG, Ashford JW, Metter EJ, Mazziotta JC (1989) Cerebral glucose metabolic patterns in Alzheimer’s disease. Effect of gender and age at dementia onset. Arch Gen Psychiatry 46(6):527–532. https://doi.org/10.1001/archpsyc.1989.01810060047008
Jiang J, Duan H, Huang Z, Yu Z, Alzheimer’s Disease Neuroimaging I (2015) Study of amyloid-beta peptide functional brain networks in AD, MCI and HC. Biomed Mater Eng 26 Suppl 1:S2197-2205. https://doi.org/10.3233/BME-151525
Zhao Q, Sang X, Metmer H, Swati Z, Lu J, Alzheimer’s Disease NeuroImaging I (2019) Functional segregation of executive control network and frontoparietal network in Alzheimer’s disease. Cortex 120:36–48. https://doi.org/10.1016/j.cortex.2019.04.026
Shirayama Y, Takahashi M, Oda Y, Yoshino K, Sato K, Okubo T, Iyo M (2019) rCBF and cognitive impairment changes assessed by SPECT and ADAS-cog in late-onset Alzheimer’s disease after 18 months of treatment with the cholinesterase inhibitors donepezil or. Brain Imaging Behav 13(1):75–86. https://doi.org/10.1007/s11682-017-9803-y
Hein G, Knight RT (2008) Superior temporal sulcus–it’s my area: or is it? J Cogn Neurosci 20(12):2125–2136. https://doi.org/10.1162/jocn.2008.20148
Govindpani K, Turner C, Waldvogel HJ, Faull RLM, Kwakowsky A (2020) Impaired expression of GABA signaling components in the Alzheimer’s disease middle temporal gyrus. Int J Mol Sci 21(22):8704. https://doi.org/10.3390/ijms21228704
Schwab S, Afyouni S, Chen Y, Han Z, Guo Q, Dierks T, Wahlund LO, Grieder M (2020) Functional connectivity alterations of the temporal lobe and hippocampus in Semantic dementia and Alzheimer’s disease. J Alzheimers Dis 76(4):1461–1475. https://doi.org/10.3233/JAD-191113
Ferretti MT, Martinkova J, Biskup E, Benke T, Gialdini G, Nedelska Z, Rauen K, Mantua V, Religa D, Hort J, Santuccione Chadha A, Schmidt R (2020) Sex and gender differences in Alzheimer’s disease: current challenges and implications for clinical practice: position paper of the dementia and cognitive disorders panel of the european academy of neurology. Eur J Neurol 27(6):928–943. https://doi.org/10.1111/ene.14174
Li X, Zhou S, Zhu W, Li X, Gao Z, Li M, Luo S, Wu X, Tian Y, Yu Y (2021) Sex Difference in network topology and education correlated with sex difference in cognition during the disease process of Alzheimer. Front Aging Neurosci 13:ss639529. https://doi.org/10.3389/fnagi.2021.639529
Compton J, van Amelsvoort T, Murphy D (2002) Mood, cognition and Alzheimer’s disease. Best Pract Res Clin Obstet Gynaecol 16(3):357–370. https://doi.org/10.1053/beog.2002.0285
Hara Y, Waters EM, McEwen BS, Morrison JH (2015) estrogen effects on cognitive and synaptic health over the lifecourse. Physiol Rev 95(3):785–807. https://doi.org/10.1152/physrev.00036.2014
Greene RA (2000) Estrogen and cerebral blood flow: a mechanism to explain the impact of estrogen on the incidence and treatment of Alzheimer’s disease. Int J Fertil Womens Med 45(4):253–257
Rueda MR, Posner MI, Rothbart MK (2005) The development of executive attention: contributions to the emergence of self-regulation. Dev Neuropsychol 28(2):573–594. https://doi.org/10.1207/s15326942dn2802_2
Edland SD, Xu Y, Plevak M, O’Brien P, Tangalos EG, Petersen RC, Jack CR Jr (2002) Total intracranial volume: normative values and lack of association with Alzheimer’s disease. Neurology 59(2):272–274. https://doi.org/10.1212/wnl.59.2.272
Acknowledgements
The authors thank the patients and their families for the time and effort they dedicated to the research.
Funding
The study was financially supported by the National Natural Science Foundation of China (Fund number: 81901726, 81771817, 82071905).
Author information
Authors and Affiliations
Contributions
Yongqiang Yu and Xiaoshu Li conceptualized and designed the study. Ziwen Gao, Shanshan Zhou, and Wanqiu Zhu were responsible for conducting the analyses, preparing the first draft of the manuscript, and preparing the manuscript for submission. Hui Li, Ziang Huang, and Yang Ji were responsible for data collection and initial data preprocessing. All authors contributed to and approved the final manuscript. All authors declared that the work has not been published before nor is being considered for publication in another journal.
Corresponding authors
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
This study was approved by the Medical Research Ethics Committee of the First Affiliated Hospital of Anhui Medical University, China, according to the Declaration of Helsinki. Informed consent was provided by all subjects.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, Z., Zhou, S., Zhu, W. et al. Sex-dependent changes in emotional memory associated with cerebral blood flow alterations during Alzheimer’s disease progression. Neuroradiology 65, 751–763 (2023). https://doi.org/10.1007/s00234-022-03099-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-03099-1