Abstract
Purpose
Posterior spinal epidural space (PSES) is a fat-containing space. We noted numerous spinal MRIs demonstrating T2-hyperintense thickening of the cervical/thoracic PSES in early newborns, resembling epidural edema. Our aim is to describe the appearance/frequency of this finding and explore any associations with delivery.
Methods
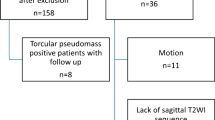
Retrospectively, 202 spinal/cranial MRIs, belonging to newborns within the first 2 weeks of life, were evaluated using sagittal fat-suppressed T2, T1-FLAIR, and STIR. Exclusion criteria were motion, incomplete spine imaging, lack of sagittal T2/STIR, and inadequate clinical data. Ninety-three patients were included in the final analysis. We reviewed all cases for T2 hyperintense thickened PSES and, if present, accompanying abnormal T1 signal. The spinal canal and PSES thickness were measured. Clinical and demographic data were collected. Follow-up exams were evaluated, if available. Cases with thickened PSES and without were compared.
Results
T2-hyperintense thickened PSES was present in 60/93 (64.5%). Mean PSES thickness was 2.3 mm (0.7–4.6). The mean PSES thickness/spinal canal diameter ratio was 0.2 (0.1–0.5). No cord compression was identified. One had a hyperintense T1 PSES signal, compatible with epidural hemorrhage. No difference was found between those with thickened PSES and without, regarding sex, gestational age, birth weight, birth method, difficult delivery, fetal position, or neurologic status (p>0.05). Follow-up imaging was available in 10, with complete resolution of T2 hyperintense PSES thickening.
Conclusion
T2 hyperintense PSES thickening is common in imaged newborns and reversible at follow-up. No significant neurologic outcomes were found related to its presence; thus, follow-up does not appear necessary.






Similar content being viewed by others
Abbreviations
- ES:
-
Epidural space
- PSES:
-
Posterior spinal epidural space
- ASES:
-
Anterior spinal epidural space
- PLL:
-
Posterior longitudinal ligament
- NST:
-
Non-stress test
- C/S:
-
Cesarean section
- NSVD:
-
Normal spontaneous vaginal delivery
References
Bromage PR (1978) Epidural analgesia. WB Saunders Company, Philadelphia
Gala FB, Aswani Y (2016) Imaging in spinal posterior epidural space lesions: a pictorial essay. Indian J Radiol. Imaging 26:299. https://doi.org/10.4103/0971-3026.190406
Boezaart AP, Prats-Galino A, Nin OC, Carrera A, Barberán J, Escobar JM et al (2019) The posterior lumbar epidural space: three-dimensional reconstruction of high-resolution MRI: Real and potential epidural spaces and their content in vivo. Pain Med 20:1687–1696. https://doi.org/10.1093/pm/pnz016
Wiltse LL, Fonseca AS, Amster J, Dimartino P, Ravessoud FA (1993) Relationship of the dura, Hofmann’s ligaments, Batson’s plexus, and a fibrovascular membrane lying on the posterior surface of the vertebral bodies and attaching to the deep layer of the posterior longitudinal ligament. An anatomical, radiologic, and clinical study. Spine 18:1030–1043. https://doi.org/10.1097/00007632-199306150-00013
Batson OV (1940) The function of the vertebral veins and their role in the spread of metastases. Ann Surg 112:138. https://doi.org/10.1097/00000658-194007000-00016
Paksoy Y, Gormus N (2004) Epidural venous plexus enlargements presenting with radiculopathy and back pain in patients with inferior vena cava obstruction or occlusion. Spine 29:2419–2424. https://doi.org/10.1097/01.brs.0000144354.36449.2f
Westbrook JL (2012) Anatomy of the epidural space. Anaesth Intensive Care Med 13:551–554. https://doi.org/10.1016/j.mpaic.2012.08.020
Romano N, Castaldi A (2020) What’s around the spinal cord? Imaging features of extramedullary diseases. Clin Imaging 60:109–122. https://doi.org/10.1016/j.clinimag.2019.12.004
Nickalls RWD, Kokri MS (1986) The width of the posterior epidural space in obstetric patients. Anaesth 41:432–433. https://doi.org/10.1111/j.1365-2044.1986.tb13240.x
Shim E, Lee JW, Lee E, Ahn JM, Kang Y, Kang HS (2017) Fluoroscopically guided epidural injections of the cervical and lumbar spine. Radiographics 37:537–561. https://doi.org/10.1148/rg.2017160043
Schijman E (1989) Comparative anatomy of the spine in the newborn, infant, and toddler. In: Raimondi AJ (ed) The Pediatric Spine I. Springer, New York, pp 1–19
Rodionov AA (2008) Variants in the structure and topography of the superior margin of the epidural space of the human spinal cord. Neurosci Behav Physiol 38:861–866. https://doi.org/10.1007/s11055-008-9057-7
Goldenberg RL (2002) The management of preterm labor. Obstet Gynecol 100:1020–1037. https://doi.org/10.1016/s0029-7844(02)02212-3
Heuchan AM, Evans N, Smart DH, Simpson JM (2002) Perinatal risk factors for major intraventricular haemorrhage in the Australian and New Zealand Neonatal Network, 1995–97. Arch Dis Child Fetal Neonatal Ed 86:86–90. https://doi.org/10.1136/fn.86.2.f86
von Beckerath AK, Kollmann M, Rotky-Fast C, Karpf E, Lang U, Klaritsch P (2013) Perinatal complications and long-term neurodevelopmental outcome of infants with intrauterine growth restriction. Am J Obstet Gynecol 208:130. https://doi.org/10.1016/j.ajog.2012.11.014
Funding
The authors declare that no funding was needed for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the University of Minnesota Institutional Review Board (IRB #: STUDY00001646). For this type of study, formal consent is not required.
Conflict of interest
Dr. David Nascene is a consultant for Biogen and World Care Clinical. The rest of the authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ceylan, A.H., Özütemiz, C., Huang, H. et al. A common yet undescribed MRI finding in newborns: posterior epidural space edema of the cervical and upper thoracic spine. Neuroradiology 64, 371–379 (2022). https://doi.org/10.1007/s00234-021-02786-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02786-9