Abstract
Purpose
Despite, currently, “state-of-the-art” magnetic resonance imaging (MRI) protocols for head and neck (H&N) lesion assessment incorporate perfusion sequences, these acquisitions require the intravenous injection of exogenous gadolinium-based contrast agents (GBCAs), which may have potential risks. Alternative techniques such as arterial spin labeling (ASL) can provide quantitative microvascular information similar to conventional perfusion sequences for H&N lesions evaluation, as a potential alternative without GBCA administration.
Methods
We review the existing literature and analyze the latest evidence regarding ASL in H&N area highlighting the technical adjustments needed for a proper ASL acquisition in this challenging region for lesion characterization, treatment monitoring, and tumor recurrence detection.
Results
ASL techniques, widely used for central nervous system lesions evaluation, can be also applied to the H&N region. Technical adjustments, especially regarding post-labeling delay, are mandatory to obtain robust and reproducible results. Several studies have demonstrated the feasibility of ASL in the H&N area including the orbits, skull base, paranasal sinuses, upper airway, salivary glands, and thyroid.
Conclusion
ASL is a feasible technique for the assessment of H&N lesions without the need of GBCAs. This manuscript reviews ASL’s physical basis, emphasizing the technical adjustments necessary for proper ASL acquisition in this unique and challenging anatomical region, and the main applications in evaluating H&N lesions.












Similar content being viewed by others
References
Sham M, Nishat S (2012) Imaging modalities in head-and-neck cancer patients. Indian J Dent Res 23:819–821
Tshering Vogel DW, Thoeny HC (2016) Cross-sectional imaging in cancers of the head and neck: how we review and report. Cancer Imaging 16:20
Chandak R, Degwekar S, Bhowte R et al (2011) An evaluation of efficacy of ultrasonography in the diagnosis of head and neck swellings. Dentomaxillofacial Radiol 40:213. https://doi.org/10.1259/DMFR/68658286
Vogl TJ (2010) Different imaging techniques in the head and neck: assets and drawbacks. World J Radiol 2:224. https://doi.org/10.4329/wjr.v2.i6.224
Wippold FJ (2007) Head and neck imaging: the role of CT and MRI. J Magn Reson Imaging 25:453–465
Jansen JFA, Parra C, Lu Y, Shukla-Dave A (2016) Evaluation of head and neck tumors with functional MR imaging. Magn Reson Imaging Clin N Am 24:123–133. https://doi.org/10.1016/j.mric.2015.08.011
Ger RB, Mohamed ASR, Awan MJ et al (2017) A multi-institutional comparison of dynamic contrast-enhanced magnetic resonance imaging parameter calculations. Sci Rep 7:11185. https://doi.org/10.1038/s41598-017-11554-w
Choi YJ, Lee JH, Sung YS et al (2016) Value of dynamic contrast-enhanced MRI to detect local tumor recurrence in primary head and neck cancer patients. Medicine (Baltimore) 95:e3698. https://doi.org/10.1097/MD.0000000000003698
Khawaja AZ, Cassidy DB, Al Shakarchi J et al (2015) Revisiting the risks of MRI with gadolinium based contrast agents—review of literature and guidelines. Insights Imaging 6:553–558
Kanda T, Nakai Y, Oba H et al (2016) Gadolinium deposition in the brain. Magn Reson Imaging 34:1346–1350. https://doi.org/10.1016/j.mri.2016.08.024
Do C, DeAguero J, Brearley A et al (2020) Gadolinium-based contrast agent use, their safety, and practice evolution. Kidney 360(1):561–568. https://doi.org/10.34067/kid.0000272019
Costelloe CM, Amini B, Madewell JE (2020) Risks and benefits of gadolinium-based contrast enhanced MRI. Semin Ultrasound CT MR 41:170–182. https://doi.org/10.1053/j.sult.2019.12.005
Lersy F, Boulouis G, Clément O et al (2020) Consensus guidelines of the French Society of Neuroradiology (SFNR) on the use of gadolinium-based contrast agents (GBCAs) and related MRI protocols in neuroradiology. J Neuroradiol 47:441–449. https://doi.org/10.1016/j.neurad.2020.05.008
Lancelot E, Raynaud JS, Desché P (2020) Current and future MR contrast agents: seeking a better chemical stability and relaxivity for optimal safety and efficacy. Invest Radiol 55:578–588. https://doi.org/10.1097/RLI.0000000000000684
Lanzman B, Heit JJ (2017) Advanced MRI measures of cerebral perfusion and their clinical applications. Top Magn Reson Imaging 26:83–90
Griffith B, Jain R (2016) Perfusion imaging in neuro-oncology: basic techniques and clinical applications. Magn Reson Imaging Clin N Am 24:765–779
Schraml C, Schwenzer NF, Claussen CD, Martirosian P (2013) Examination of tissue perfusion by arterial spin labeling (ASL). Curr Radiol Rep 1:93–101. https://doi.org/10.1007/s40134-013-0009-9
Odudu A, Nery F, Harteveld AA et al (2018) Arterial spin labelling MRI to measure renal perfusion: a systematic review and statement paper. Nephrol Dial Transplant 33:ii15–ii21. https://doi.org/10.1093/ndt/gfy180
Schawkat K, Ith M, Christe A et al (2018) Dynamic non-invasive asl perfusion imaging of a normal pancreas with secretin augmented mr imaging. Eur Radiol 28:2389–2396. https://doi.org/10.1007/s00330-017-5227-8
Xiao B, Wang P, Zhao Y et al (2020) Nasopharyngeal carcinoma perfusion MRI: comparison of arterial spin labeling and dynamic contrast-enhanced MRI. Medicine (Baltimore) 99:e20503. https://doi.org/10.1097/MD.0000000000020503
Abdel Razek AAK, Talaat M, El-Serougy L et al (2019) Clinical applications of arterial spin labeling in brain tumors. J Comput Assist Tomogr 43:525–532
Alsop DC, Detre JA, Golay X et al (2015) Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med 73:102–116. https://doi.org/10.1002/mrm.25197
Grade M, Hernandez Tamames JA, Pizzini FB et al (2015) A neuroradiologist’s guide to arterial spin labeling MRI in clinical practice. Neuroradiology 57:1181–1202. https://doi.org/10.1007/s00234-015-1571-z
Petcharunpaisan S (2010) Arterial spin labeling in neuroimaging. World J Radiol 2:384. https://doi.org/10.4329/wjr.v2.i10.384
Vidorreta M, Wang Z, Rodriguez I et al (2013) Comparison of 2D and 3D single-shot ASL perfusion fMRI sequences. Neuroimage 66:662–671. https://doi.org/10.1016/j.neuroimage.2012.10.087
Fernández-Seara MA, Wang Z, Wang J et al (2005) Continuous arterial spin labeling perfusion measurements using single shot 3D GRASE at 3 T. Magn Reson Med 54:1241–1247. https://doi.org/10.1002/mrm.20674
Gai ND, Butman JA (2019) Determining the optimal postlabeling delay for arterial spin labeling using subject-specific estimates of blood velocity in the carotid artery. J Magn Reson Imaging 50:951–960. https://doi.org/10.1002/jmri.26670
Fujima N, Kudo K, Tsukahara A et al (2015) Measurement of tumor blood flow in head and neck squamous cell carcinoma by pseudo-continuous arterial spin labeling: comparison with dynamic contrast-enhanced MRI. J Magn Reson Imaging 41:983–991. https://doi.org/10.1002/jmri.24637
Hirasawa S, Tsushima Y, Takei H et al (2007) Inverse correlation between tumor perfusion and glucose uptake in human head and neck tumors. Acad Radiol 14:312–318. https://doi.org/10.1016/j.acra.2006.12.017
Lin M, Yu X, Ouyang H et al (2015) Consistency of T2WI-FS/ASL fusion images in delineating the volume of nasopharyngeal carcinoma. Sci Rep 5:1–8. https://doi.org/10.1038/srep18431
Sato Y, Matsumoto M (2017) Clinical usefulness of multiphase arterial spin labeling imaging for evaluating cerebral hemodynamic status in a patient with symptomatic carotid stenosis by comparison with single-photon emission computed tomography: a case study. Radiol Case Reports 12:824–826. https://doi.org/10.1016/j.radcr.2017.08.012
Mezue M, Segerdahl AR, Okell TW et al (2014) Optimization and reliability of multiple postlabeling delay pseudo-continuous arterial spin labeling during rest and stimulus-induced functional task activation. J Cereb Blood Flow Metab 34:1919–1927. https://doi.org/10.1038/jcbfm.2014.163
Geerts B, Leclercq D, Tezenas du Montcel S, et al (2017) Characterization of skull base lesions using pseudo-continuous arterial spin labeling. Clin Neuroradiol 1–12. https://doi.org/10.1007/s00062-017-0623-7
Fujima N, Nakamaru Y, Sakashita T et al (2015) Differentiation of squamous cell carcinoma and inverted papilloma using non-invasive MR perfusion imaging. Dentomaxillofacial Radiol 44:20150074. https://doi.org/10.1259/dmfr.20150074
Mamlouk MD, Hess CP (2016) Arterial spin-labeled perfusion for vascular anomalies in the pediatric head and neck. Clin Imaging 40:1040–1046. https://doi.org/10.1016/j.clinimag.2016.06.009
Eissa L, Abdel Razek AAK, Helmy E (2021) Arterial spin labeling and diffusion-weighted MR imaging: utility in differentiating idiopathic orbital inflammatory pseudotumor from orbital lymphoma. Clin Imaging 71:63–68. https://doi.org/10.1016/j.clinimag.2020.10.057
Razek AAKA (2019) Multi-parametric MR imaging using pseudo-continuous arterial-spin labeling and diffusion-weighted MR imaging in differentiating subtypes of parotid tumors. Magn Reson Imaging 63:55–59. https://doi.org/10.1016/j.mri.2019.08.005
Fujima N, Yoshida D, Sakashita T et al (2016) Usefulness of pseudocontinuous arterial spin-labeling for the assessment of patients with head and neck squamous cell carcinoma by measuring tumor blood flow in the pretreatment and early treatment period. Am J Neuroradiol 37:342–348. https://doi.org/10.3174/ajnr.A4513
Yamamoto T, Kimura H, Hayashi K et al (2018) Pseudo-continuous arterial spin labeling MR images in Warthin tumors and pleomorphic adenomas of the parotid gland: qualitative and quantitative analyses and their correlation with histopathologic and DWI and dynamic contrast enhanced MRI findings. Neuroradiology 60:803–812. https://doi.org/10.1007/s00234-018-2046-9
Abdel Razek AAK (2018) Arterial spin labelling and diffusion-weighted magnetic resonance imaging in differentiation of recurrent head and neck cancer from post-radiation changes. J Laryngol Otol 132:923–928. https://doi.org/10.1017/S0022215118001743
Razek AAKA, Helmy E (2020) Multi-parametric arterial spin labeling and diffusion-weighted imaging in differentiation of metastatic from reactive lymph nodes in head and neck squamous cell carcinoma. Eur Arch Oto-Rhino-Laryngology. https://doi.org/10.1007/s00405-020-06390-0
Sokolska M, Bainbridge A, Rojas-Villabona A et al (2019) Effect of labelling plane angulation and position on labelling efficiency and cerebral blood flow quantification in pseudo-continuous arterial spin labelling. Magn Reson Imaging 59:61–67. https://doi.org/10.1016/j.mri.2019.02.007
Xu G, Rowley HA, Wu G et al (2010) Reliability and precision of pseudo-continuous arterial spin labeling perfusion MRI on 3.0 T and comparison with 15O-water PET in elderly subjects at risk for Alzheimer’s disease. NMR Biomed 23:286–293. https://doi.org/10.1002/nbm.1462
Fallatah SM, Pizzini FB, Gomez-Anson B, et al (2018) A visual quality control scale for clinical arterial spin labeling images. Eur Radiol Exp 2. https://doi.org/10.1186/s41747-018-0073-2
Ma G, Xu X-Q, Zhu L-N, et al (2020) Intravoxel incoherent motion magnetic resonance imaging for assessing parotid gland tumors: correlation and comparison with arterial spin labeling imaging. Korean J Radiol 21. https://doi.org/10.3348/kjr.2020.0290
Kato H, Kanematsu M, Watanabe H et al (2015) Perfusion imaging of parotid gland tumours: usefulness of arterial spin labeling for differentiating Warthin’s tumours. Eur Radiol 25:3247–3254. https://doi.org/10.1007/s00330-015-3755-7
Buxton RB (2005) Quantifying CBF with arterial spin labeling. In: Journal of Magnetic Resonance Imaging, pp 723–726
Wu WC, St Lawrence KS, Licht DJ, Wang DJJ (2010) Quantification issues in arterial spin labeling perfusion magnetic resonance imaging. Top Magn Reson Imaging 21:65–73. https://doi.org/10.1097/RMR.0b013e31821e570a
Abdel Razek AAK, Nada N (2018) Arterial spin labeling perfusion-weighted MR imaging: correlation of tumor blood flow with pathological degree of tumor differentiation, clinical stage and nodal metastasis of head and neck squamous cell carcinoma. Eur Arch Oto-Rhino-Laryngology 275:1301–1307. https://doi.org/10.1007/s00405-018-4950-3
Kabadi SJ, Fatterpekar GM, Anzai Y et al (2018) Dynamic contrast-enhanced MR imaging in head and neck cancer. Magn Reson Imaging Clin N Am 26:135–149
Sourbron S (2010) Technical aspects of MR perfusion. Eur J Radiol 76:304–313. https://doi.org/10.1016/j.ejrad.2010.02.017
Kim HS, Kim SY (2007) A prospective study on the added value of pulsed arterial spin-labeling and apparent diffusion coefficients in the grading of gliomas. Am J Neuroradiol 28:1693–1699. https://doi.org/10.3174/ajnr.A0674
Bogin L, Margalit R, Mispelter J, Degani H (2002) Parametric imaging of tumor perfusion using flow- and permeability-limited tracers. J Magn Reson Imaging 16:289–299. https://doi.org/10.1002/jmri.10159
Fujima N, Nakamaru Y, Sakashita T et al (2015) Differentiation of squamous cell carcinoma and inverted papilloma using non-invasive MR perfusion imaging. Dentomaxillofacial Radiol 44:1–8. https://doi.org/10.1259/dmfr.20150074
Fujima N, Kameda H, Tsukahara A et al (2015) Diagnostic value of tumor blood flow and its histogram analysis obtained with pCASL to differentiate sinonasal malignant lymphoma from squamous cell carcinoma. Eur J Radiol 84:2187–2193. https://doi.org/10.1016/j.ejrad.2015.07.026
Ahn Y, Choi YJ, Sung YS et al (2021) Histogram analysis of arterial spin labeling perfusion data to determine the human papillomavirus status of oropharyngeal squamous cell carcinomas. Neuroradiology. https://doi.org/10.1007/s00234-021-02751-6
Iida E, Wiggins RH, Anzai Y (2016) Bilateral parotid oncocytoma with spontaneous intratumoral hemorrhage: a rare hypervascular parotid tumor with ASL perfusion. Clin Imaging 40:357–360. https://doi.org/10.1016/j.clinimag.2016.02.003
Fujima N, Kudo K, Yoshida D et al (2013) Arterial spin labeling to determine tumor viability in head and neck cancer before and after treatment. J Magn Reson Imaging 40:920–928. https://doi.org/10.1002/jmri.24421
Sakai M, Illies T, Jerusel N et al (2016) Feasibility of non-contrast-enhanced four dimensional (4D) MRA in head and neck tumors, comparison with contrast-enhanced 4D MRA. Springerplus 5:1–9. https://doi.org/10.1186/s40064-016-2953-3
Schraml C, Müssig K, Martirosian P et al (2009) Autoimmune thyroid disease: arterial spin-labeling perfusion MR imaging. Radiology 253:435–442. https://doi.org/10.1148/radiol.2533090166
Müssig K, Schraml C, Gallwitz B et al (2007) A novel MR-imaging technique using arterial spin labeling for thyroid gland perfusion in thyrotoxicosis. Thyroid 17:1155–1156. https://doi.org/10.1089/thy.2007.0019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare conflict of interest.
Claudia Kirsch is a consultant of Primal Pictures 3D Anatomy-Informa and receives royalties. Paula Montesinos, PhD, is a clinical scientist of Philips Iberia. Antonio Luna, MD, PhD, is an occasional lecturer of Philips, Siemens Healthineers, Bracco, and Canon and receives royalties as book editor from Springer-Verlag.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
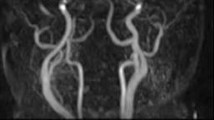
Video 1 Scheme with necessary steps for ASL acquisition. Labeling plane is usually located at CCA and encompass an inversion pulse that conditions a change in blood water molecules spin magnetization. After spins are labeled, a time labeling delay must be waited till tagged blood reaches the anatomical region of interest. The readout sequence, acquired after the PLD time, can detect and read the changes in local tissue magnetization that labeled blood induces. (MP4 1333 KB)
Video 2 Scheme with different types of ASL acquisitions. CASL uses a large duration narrow labeling plane with a large readout FOV. PCASL uses a train of short RF and gradient pulses with a reduced readout FOV. PASL uses a single large label plane for a short time with a reduced FOV. (MP4 1326 KB)
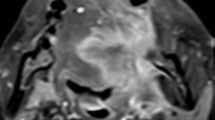
Video 3 Invasive orbital melanoma. 90 y–o female with a large mass on the left globe underwent an MRI study. (a) Axial STIR image confirms the presence of a large ill-defined mass that invades the left globe. (b) Overlay of axial T1 FFE and TBF map from pCASL shows a severe increase of TBF within the globe mass. (c) Axial contrast-enhanced water only T1 Dixon shows patchy enhancement of the lesion (arrows). (d) Relative enhancement map from DCE-MRI sequence demonstrates a marked increase of perfusion within the lesions. Notice the comparable results regarding the degree of perfusion increase within the mass on both pCASL and DCE-MRI sequences. (MP4 961 KB)
Video 4 Autoimmune Thyroiditis. 20 y–o female with neck pain. Diffuse increase of thyroid gland is identified on axial STIR image (upper left corner of the video). Using a PLD of 1000 ms (right scheme), a better identification of patchy areas of blood flow increase within the thyroid is achieved (arrows), as the thyroid gland is near to labeling and readout planes so labeled blood can be detected in comparison to 1800 ms acquisition (left scheme) whereas labeling effect disappears if large PLD is waited. (MP4 3334 KB)
Rights and permissions
About this article
Cite this article
Martín-Noguerol, T., Kirsch, C.F.E., Montesinos, P. et al. Arterial spin labeling for head and neck lesion assessment: technical adjustments and clinical applications. Neuroradiology 63, 1969–1983 (2021). https://doi.org/10.1007/s00234-021-02772-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02772-1