Abstract
Purpose
The aim of this study is to demonstrate the diagnostic effect of VWI in differentiating PACNS from other vasculopathies and its role in post-treatment follow-up in PACNS patients in this study.
Methods
In this prospective study, we included patients with clinical suspicion of PACNS who presented with new-onset ischemic events and had significant intracranial large vessel stenosis on DSA or MRA. VWI was performed on all patients. The imaging findings and final diagnoses were recorded. Control VWI was performed on patients with PACNS diagnosis after at least 3 months of treatment, and the change in findings was also evaluated.
Results
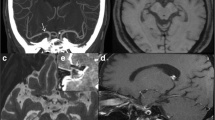
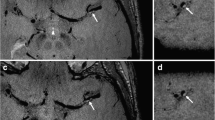
Twenty-three patients were included in the study had a median age of 40 (range 12–58). The most common clinical manifestations were focal neurologic deficits. According to the initial clinical evaluation, 10 patients (43.5%) were classified as PACNS and 13 patients (56.5%) as indeterminate for PACNS. After incorporating the VWI findings, the diagnosis of PACNS was confirmed in all clinically diagnosed PACNS patients. Concentric wall thickening and contrast enhancement were statistically significant in the PACNS group (p <0.001). According to concentric thickening and VWE features, sensitivity and specificity in distinguishing PACNS and other vasculopathies were 95.2%, 75% and 95.2%, 68.8%, respectively. Vessel wall enhancement regressed in 7 of 9 patients during a median follow-up period of 8 months (range 5.5–11.5) in PACNS patients who followed up.
Conclusion
VWI seems a new and useful imaging method in the differential diagnosis of PACNS and might be a useful adjunct for post-treatment follow-up.



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- VW-MRI:
-
Vessel wall magnetic resonance imaging
- PACNS:
-
Primary angiitis of the central nervous system
- RCVS:
-
Reversible cerebral vasoconstriction syndrome
- MMD:
-
Moya Moya disease
- VWE:
-
Vessel wall enhancement
- VWT:
-
Vessel wall thickening
- VWI:
-
Vessel wall imaging
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- TIA:
-
Transient ischemic attack
- DSA:
-
Digital subtraction angiography
- DWI:
-
Diffusion-weighted imaging
- SWI:
-
Susceptibility-weighted imaging
- TOF-MRA:
-
Time of flight MR angiography
- MIP:
-
Maximum intensity projection
- ACA:
-
Anterior cerebral artery
- MCA:
-
Middle cerebral artery
- PCA:
-
Posterior cerebral artery
- ICA:
-
Internal carotid artery
- CSF:
-
Cerebrospinal fluid
- F/U:
-
Follow-up
- S:
-
Steroid
- MTX:
-
Methotrexate
- Aza:
-
Azathioprine
- Cfc:
-
Cyclophosphamide
References
Lie JT (1997) Classification and histopathologic spectrum of central nervous system vasculitis. Neurol Clin 15(4):805–819. https://doi.org/10.1016/s0733-8619(05)70348-0
Calabrese LH, Mallek JA (1988) Primary angiitis of the central nervous system. Report of 8 new cases, review of the literature, and proposal for diagnostic criteria. Medicine (Baltimore) 67(1):20–39. https://doi.org/10.1097/00005792-198801000-00002
Berlit P, Kraemer M (2014) Cerebral vasculitis in adults: what are the steps in order to establish the diagnosis? Red flags and pitfalls. Clin Exp Immunol 175(3):419–424. https://doi.org/10.1111/cei.12221
Salvarani C, Brown RDJ, Christianson T et al (2015) An update of the Mayo Clinic cohort of patients with adult primary central nervous system vasculitis: description of 163 patients. Medicine (Baltimore) 94(21):e738. https://doi.org/10.1097/MD.0000000000000738
Hajj-Ali RA, Singhal AB, Benseler S, Molloy E, Calabrese LH (2011) Primary angiitis of the CNS. Lancet Neurol 10(6):561–572. https://doi.org/10.1016/S1474-4422(11)70081-3
Birnbaum J, Hellmann DB (2009) Primary angiitis of the central nervous system. JAMA Neurol 66(6):704–709. https://doi.org/10.1001/archneurol.2009.76
Duna GF, Calabrese LH (1995) Limitations of invasive modalities in the diagnosis of primary angiitis of the central nervous system. J Rheumatol 22(4):662–667
Salvarani C, Brown RD Jr, Calamia KT et al (2007) Primary central nervous system vasculitis: analysis of 101 patients. Ann Neurol 62(5):442–451. https://doi.org/10.1002/ana.21226
Kesav P, Krishnavadana B, Kesavadas C, Sreedharan SE, Rajendran A, Sukumaran S, Sylaja PN (2019) Utility of intracranial high-resolution vessel wall magnetic resonance imaging in differentiating intracranial vasculopathic diseases causing ischemic stroke. Neuroradiology. 61(4):389–396. https://doi.org/10.1007/s00234-019-02157-5
Mahmud M-B, K. SD, K. (2017) HD, et al. Added value of vessel wall magnetic resonance imaging for differentiation of nonocclusive intracranial vasculopathies. Stroke. 48(11):3026–3033. https://doi.org/10.1161/STROKEAHA.117.018227
Schaafsma JD, Rawal S, Coutinho JM, Rasheedi J, Mikulis DJ, Jaigobin C, Silver FL, Mandell DM (2019) Diagnostic impact of intracranial vessel wall MRI in 205 patients with ischemic stroke or TIA. Am J Neuroradiol. https://doi.org/10.3174/ajnr.A6202
Mandell DM, Mossa-Basha M, Qiao Y et al (2017) Intracranial vessel wall MRI: principles and expert consensus recommendations of the American Society of Neuroradiology. Am J Neuroradiol 38(2):218 LP–218229. https://doi.org/10.3174/ajnr.A4893
Küker W, Gaertner S, Nägele T et al (2008) Vessel wall contrast enhancement: a diagnostic sign of cerebral vasculitis. Cerebrovasc Dis 26(1):23–29. https://doi.org/10.1159/000135649
Obusez EC, Hui F, Hajj-Ali RA, Cerejo R, Calabrese LH, Hammad T, Jones SE (2014 Aug) High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitis. AJNR Am J Neuroradiol 35(8):1527–1532. https://doi.org/10.3174/ajnr.A3909
Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI (2000) A standardized method for measuring intracranial arterial stenosis. Am J Neuroradiol 21(4):643 LP–643646
Lindenholz A, van der Kolk AG, Zwanenburg JJM, Hendrikse J (2018) The use and pitfalls of intracranial vessel wall imaging: how we do it. Radiology 286(1):12–28. https://doi.org/10.1148/radiol.2017162096
Turan TN, Bonilha L, Morgan PS, Adams RJ, Chimowitz MI (2011) Intraplaque hemorrhage in symptomatic intracranial atherosclerotic disease. J Neuroimaging 21(2):e159–e161. https://doi.org/10.1111/j.1552-6569.2009.00442.x
Salvarani C, Brown RDJ, Hunder GG (2012) Adult primary central nervous system vasculitis. Lancet (London, England) 380(9843):767–777. https://doi.org/10.1016/S0140-6736(12)60069-5
Mossa-Basha M, Hwang WD, De Havenon A et al (2015) Multicontrast high-resolution vessel wall magnetic resonance imaging and its value in differentiating intracranial vasculopathic processes. Stroke. 46(6):1567–1573. https://doi.org/10.1161/STROKEAHA.115.009037
Obusez EC, Hui F, Hajj-ali RA et al (2014) High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitis. Am J Neuroradiol 35(8):1527 LP–1521532. https://doi.org/10.3174/ajnr.A3909
Pfefferkorn T, Linn J, Habs M, Opherk C, Cyran C, Ottomeyer C, Straube A, Dichgans M, Nikolaou K, Saam T (2013) Black blood MRI in suspected large artery primary angiitis of the central nervous system. J Neuroimaging 23(3):379–383. https://doi.org/10.1111/j.1552-6569.2012.00743.x
Mossa-basha M, Alexander M, Gaddikeri S, Yuan C (2016) Vessel wall imaging for intracranial vascular disease evaluation:1154–1159. https://doi.org/10.1136/neurintsurg-2015-012127
Bang OY, Toyoda K, Arenillas JF, Liu L, Kim JS (2018) Intracranial large artery disease of non-atherosclerotic origin: recent progress and clinical implications. J stroke 20(2):208–217. https://doi.org/10.5853/jos.2018.00150
Ryu C-W, Jahng G-H, Shin HS (2014) Gadolinium enhancement of atherosclerotic plaque in the middle cerebral artery: relation to symptoms and degree of stenosis. Am J Neuroradiol 35(12):2306 LP–2302310. https://doi.org/10.3174/ajnr.A4038
Portanova A, Hakakian N, Mikulis DJ, Virmani R, Abdalla WMA, Wasserman BA (2013) Intracranial vasa vasorum: insights and implications for imaging. Radiology. 267(3):667–679. https://doi.org/10.1148/radiol.13112310
Wang J, Yarnykh VL, Hatsukami T, Chu B, Balu N, Yuan C (2007) Improved suppression of plaque-mimicking artifacts in black-blood carotid atherosclerosis imaging using a Turbo Spin-Echo ( TSE ) Sequence 981:973-981. https://doi.org/10.1002/mrm.21385
Wang M, Yang Y, Zhou F, Li M, Liu R, Guan M, Li R, He L, Xu Y, Zhang B, Zhu B, Zhao X (2017) The contrast enhancement of intracranial arterial wall on high-resolution MRI and its clinical relevance in patients with moyamoya vasculopathy. Sci Rep 7(1):44264. https://doi.org/10.1038/srep44264
Harteveld AA, van der Kolk AG, van der Worp HB, Dieleman N, Zwanenburg JJM, Luijten PR, Hendrikse J (2017) Detecting intracranial vessel wall lesions with 7 T-magnetic resonance imaging. Stroke. 48(9):2601–2604. https://doi.org/10.1161/STROKEAHA.117.017868
Song JW, Shou H, Obusez EC, Raymond SB, Rafla SD, Kharal GA, Schaefer PW, Romero JM (2019) Spatial distribution of intracranial vessel wall enhancement in hypertension and primary angiitis of the CNS. Sci Rep 9(1):19270. https://doi.org/10.1038/s41598-019-55634-5
Kalsoum E, Chabernaud Negrier A, Tuilier T et al (2018) Blood Flow Mimicking aneurysmal wall enhancement: a diagnostic pitfall of vessel wall mri using the postcontrast 3D turbo spin-echo MR imaging sequence. Am J Neuroradiol 39(6):1065 LP–1061067. https://doi.org/10.3174/ajnr.A5616
Cornelissen BMW, Leemans EL, Slump CH, Marquering HA, Majoie CBLM, van den Berg R (2019) Vessel wall enhancement of intracranial aneurysms: fact or artifact? Neurosurg Focus FOC 47(1):E18. https://doi.org/10.3171/2019.4.FOCUS19236
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conception and design: Civan Islak, Naci Kocer, and Ahmet Kursat Karaman. Data collection, data analysis: Ahmet Kursat Karaman, Ugur Uygunoglu, Bora Korkmazer, and Ercan Karaarslan. Drafting the article: Ahmet Kursat Karaman, Bora Korkmazer, Serdar Arslan, Osman Kızılkılıc, and Ercan Karaarslan. Critical revision of the manuscript: Serdar Arslan, Ugur Uygunoglu, Osman Kızılkılıc, Naci Kocer, and Civan Islak. All listed authors have approved the manuscript before submission, including the names and order of authors; managing all communication between the Journal and all co-authors, before and after publication; * providing transparency on the re-use of material and mention any unpublished material included in the manuscript in a cover letter to the Editor; making sure disclosures, declarations, and transparency on data statements from all authors are included in the manuscript as appropriate.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no relevant conflicts of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karaman, A.K., Korkmazer, B., Arslan, S. et al. The diagnostic contribution of intracranial vessel wall imaging in the differentiation of primary angiitis of the central nervous system from other intracranial vasculopathies. Neuroradiology 63, 1635–1644 (2021). https://doi.org/10.1007/s00234-021-02686-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02686-y