Abstract
Background
Computational fluid dynamics (CFD) are important in evaluating the hemodynamics of intracranial aneurysm rupture, and the setting of inflow boundary conditions is critical. We evaluated intracranial aneurysm hemodynamics based on generalized versus patient-specific inflow boundary conditions to examine the effect of different hemodynamic results on the discrimination of intracranial aneurysm rupture status.
Methods
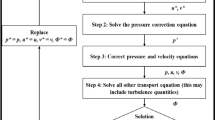
We enrolled 148 patients with 156 intracranial aneurysms. For each included aneurysm, we performed CFD simulation once based on patient-specific and once based on generalized inflow boundary conditions. First, we compared the hemodynamics of intracranial aneurysms based on different inflow boundary conditions. Then, we divided the included aneurysms into a ruptured and unruptured group and compared the hemodynamics between the two groups under patient-specific and generalized inflow boundary conditions.
Results
For the hemodynamic parameters using specific inflow boundary conditions, more complex flow (p = 0.002), larger minimum WSS (p = 0.024), lower maximum low WSS area (LSA) (p = 0.038), and oscillatory shear index (p = 0.002) were found. Furthermore, we compared the hemodynamics between ruptured and unruptured groups based on different inflow boundary conditions. We found that the significant hemodynamic parameters associated with rupture status were the same, including the proportion of aneurysms with flow complex and unstable flow and the minimum and maximum of LSA (p = 0.011, p = 0.003, p = 0.001 and p = 0.004, respectively).
Conclusion
Patient-specific and generalized inflow boundary conditions of aneurysmal hemodynamics resulted in significant differences. However, the significant parameters associated with rupture status were the same in both conditions, indicating that patient-specific inflow boundary conditions may not be necessary for predicting rupture risk.




Similar content being viewed by others
Abbreviations
- WSS:
-
Wall shear stress
- CFD:
-
Computational fluid dynamics
- TCD:
-
Transcranial Doppler sonography
- TAWSS:
-
Time-averaged WSS
- OSI:
-
Oscillatory shear index
- LSA:
-
Low WSS area
References
Etminan N, Rinkel GJ (2016) Unruptured intracranial aneurysms: development, rupture and preventive management. Nat Rev Neurol 12(12):699–713
Xiang J, Natarajan SK, Tremmel M, Ma D, Mocco J, Hopkins LN, Siddiqui AH, Levy EI, Meng H (2011) Hemodynamic-morphologic discriminants for intracranial aneurysm rupture. Stroke. 42(1):144–152
Shojima M, Oshima M, Takagi K, Torii R, Hayakawa M, Katada K, Morita A, Kirino T (2004) Magnitude and role of wall shear stress on cerebral aneurysm: computational fluid dynamic study of 20 middle cerebral artery aneurysms. Stroke. 35(11):2500–2505
Can A, Du R (2016) Association of hemodynamic factors with intracranial aneurysm formation and rupture: systematic review and meta-analysis. Neurosurgery. 78(4):510–520
Meng H, Wang Z, Hoi Y, Gao L, Metaxa E, Swartz DD, Kolega J (2007) Complex hemodynamics at the apex of an arterial bifurcation induces vascular remodeling resembling cerebral aneurysm initiation. Stroke. 38(6):1924–1931
Luo B, Yang X, Wang S, Li H, Chen J, Yu H, Zhang Y, Zhang Y, Mu S, Liu Z, Ding G (2011) High shear stress and flow velocity in partially occluded aneurysms prone to recanalization. Stroke. 42(3):745–753
Boussel L, Rayz V, McCulloch C, Martin A, Acevedo-Bolton G, Lawton M, Higashida R, Smith WS, Young WL, Saloner D (2008) Aneurysm growth occurs at region of low wall shear stress: patient-specific correlation of hemodynamics and growth in a longitudinal study. Stroke. 39(11):2997–3002
Liu J, Fan J, Xiang J, Zhang Y, Yang X (2016) Hemodynamic characteristics of large unruptured internal carotid artery aneurysms prior to rupture: a case control study. J Neurointerv Surg 8(4):367–372
Zhang Y, Jing L, Liu J, Li C, Fan J, Wang S, Li H, Yang X (2016) Clinical, morphological, and hemodynamic independent characteristic factors for rupture of posterior communicating artery aneurysms. J Neurointerv Surg. 8(8):808–812
Tian Z, Zhang Y, Jing L, Liu J, Zhang Y, Yang X (2016) Rupture risk assessment for mirror aneurysms with different outcomes in the same patient. Front Neurol 7:219
Xiang J, Siddiqui AH, Meng H (2014) The effect of inlet waveforms on computational hemodynamics of patient-specific intracranial aneurysms. J Biomech 47(16):3882–3890
Jansen IG, Schneiders JJ, Potters WV et al (2014) Generalized versus patient-specific inflow boundary conditions in computational fluid dynamics simulations of cerebral aneurysmal hemodynamics. AJNR Am J Neuroradiol 35(8):1543–1548
Liu J, Zhang Y, Wang A, Zhang Y, Li Y, Yang X (2017) Haemodynamic analysis for recanalisation of intracranial aneurysms after endovascular treatment: an observational registry study in China. BMJ Open 7(5):e014261
Li W, Liu J, Zhang Y, Wang K, Tian Z, Zhang Q, Jiang C, Yang X, Wang Y (2017) Flow diversion and outcomes of vertebral fusiform aneurysms after stent-only treatment: a hemodynamic study. World Neurosurg 107:202–210
Cebral JR, Mut F, Weir J, Putman CM (2011) Association of hemodynamic characteristics and cerebral aneurysm rupture. AJNR Am J Neuroradiol 32(2):264–270
He X, Ku DN (1996) Pulsatile flow in the human left coronary artery bifurcation: average conditions. J Biomech Eng 118(1):74–82
Cancelliere NM, Najafi M, Brina O et al (2020) 4D-CT angiography versus 3D-rotational angiography as the imaging modality for computational fluid dynamics of cerebral aneurysms. J Neurointerv Surg 12(6):626–630
Pereira VM, Brina O, Marcos GA et al (2013) Evaluation of the influence of inlet boundary conditions on computational fluid dynamics for intracranial aneurysms: a virtual experiment. J Biomech 46(9):1531–1539
Castro MA, Putman CM, Cebral JR (2006) Patient-specific computational fluid dynamics modeling of anterior communicating artery aneurysms: a study of the sensitivity of intra-aneurysmal flow patterns to flow conditions in the carotid arteries. AJNR Am J Neuroradiol 27(10):2061–2068
Hassan T, Ezura M, Timofeev EV, Tominaga T, Saito T, Takahashi A, Takayama K, Yoshimoto T (2004) Computational simulation of therapeutic parent artery occlusion to treat giant vertebrobasilar aneurysm. AJNR Am J Neuroradiol 25(1):63–68
Karmonik C, Yen C, Diaz O, Klucznik R, Grossman RG, Benndorf G (2010) Temporal variations of wall shear stress parameters in intracranial aneurysms--importance of patient-specific inflow waveforms for CFD calculations. Acta Neurochir 152(8):1391–1398 discussion 1398
Karmonik C, Yen C, Grossman RG, Klucznik R, Benndorf G (2009) Intra-aneurysmal flow patterns and wall shear stresses calculated with computational flow dynamics in an anterior communicating artery aneurysm depend on knowledge of patient-specific inflow rates. Acta Neurochir 151(5):479–485 discussion 485
Marzo A, Singh P, Larrabide I, Radaelli A, Coley S, Gwilliam M, Wilkinson ID, Lawford P, Reymond P, Patel U, Frangi A, Hose DR (2011) Computational hemodynamics in cerebral aneurysms: the effects of modeled versus measured boundary conditions. Ann Biomed Eng 39(2):884–896
Valen-Sendstad K, Steinman DA (2014 Mar 1) Mind the gap: impact of computational fluid dynamics solution strategy on prediction of intracranial aneurysm hemodynamics and rupture status indicators. Am J Neuroradiol 35(3):536–543
Durka MJ, Wong IH, Kallmes DF, Pasalic D, Mut F, Jagani M, Blanco PJ, Cebral JR, Robertson AM (2018) A data-driven approach for addressing the lack of flow waveform data in studies of cerebral arterial flow in older adults. Physiol Meas 39(1):015006
Berg P, Saalfeld S, Voß S, Beuing O, Janiga G (2019) A review on the reliability of hemodynamic modeling in intracranial aneurysms: why computational fluid dynamics alone cannot solve the equation. Neurosurg Focus 47(1):E15
Evju Ø, Pozo JM, Frangi AF, Mardal KA (2017) Robustness of common hemodynamic indicators with respect to numerical resolution in 38 middle cerebral artery aneurysms. PLoS One 12(6):e0177566
Geers AJ, Larrabide I, Morales HG, Frangi AF (2014) Approximating hemodynamics of cerebral aneurysms with steady flow simulations. J Biomech 47(1):178–185
Castro MA, Putman CM, Sheridan MJ, Cebral JR (2009) Hemodynamic patterns of anterior communicating artery aneurysms: a possible association with rupture. AJNR Am J Neuroradiol 30(2):297–302
Doddasomayajula R, Chung B, Hamzei-Sichani F, Putman CM, Cebral JR (2017) Differences in hemodynamics and rupture rate of aneurysms at the bifurcation of the basilar and internal carotid arteries. AJNR Am J Neuroradiol 38(3):570–576
Rashad S, Sugiyama SI, Niizuma K et al (2018) Impact of bifurcation angle and inflow coefficient on the rupture risk of bifurcation type basilar artery tip aneurysms. J Neurosurg 128(3):723–730
Cebral JR, Mut F, Raschi M, Scrivano E, Ceratto R, Lylyk P, Putman CM (2011) Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol 32(1):27–33
Yu H, Li H, Liu J, Yang X (2016) An approach to quantitative assessment of hemodynamic differences between unruptured and ruptured ophthalmic artery aneurysms. Comput Methods Biomech Biomed Engin 19(13):1456–1461
Cebral JR, Castro MA, Burgess JE, Pergolizzi RS, Sheridan MJ, Putman CM (2005) Characterization of cerebral aneurysms for assessing risk of rupture by using patient-specific computational hemodynamics models. AJNR Am J Neuroradiol 26(10):2550–2559
Funding
This work was supported by National Key Research and Development Plan of China (grant number: 2016YFC1300800), the National Natural Science Foundation of China (grant numbers: 81801156, 81801158, 81471167, and 81671139), the Special Research Project for Capital Health Development (grant number: 2018-4-1077), Beijing Hospitals Authority Youth Programme (code: QML20190503), the Innovation Fund of Nanchang University for Graduate Students (No. cx2016312).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethics committee of Beijing Tiantan Hospital. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Li, W., Wang, S., Tian, Z. et al. Discrimination of intracranial aneurysm rupture status: patient-specific inflow boundary may not be a must-have condition in hemodynamic simulations. Neuroradiology 62, 1485–1495 (2020). https://doi.org/10.1007/s00234-020-02473-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02473-1