Abstract
Purpose
To identify if specific findings on magnetic resonance imaging (MRI) cerebrospinal fluid (CSF) flow studies can be utilised to identify which patients with idiopathic normal pressure hydrocephalus (iNPH) will have improved gait following a CSF tap test (TT).
Methods
Prospective study of patients undergoing a CSF TT for iNPH. Functional gait was assessed using the timed up and go (TUG) test before and after the CSF TT. MRI CSF flow studies accompanied the CSF TT. The minimum clinically important difference for the TUG (3.63 s) was used as a cutoff value to categorise patients as responders to the CSF TT.
Results
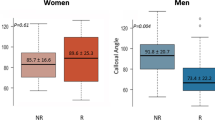
Fifty-three patients underwent CSF TT and MRI CSF flow studies. Significant differences were identified between groups for (non-responder vs responder) superior sagittal sinus flow (47.10% vs 40.41%), sagittal sinus stroke volume (274 vs 176.5 μl), sagittal sinus to arterial stroke volume ratio (0.203 vs 0.164), sagittal sinus area (42.2 mm2 vs 36.2 mm2) and circumference (27.7 mm vs 24.95 mm). No differences were present for aqueduct stroke volume, arterial stroke volume or aqueduct net flow.
Conclusion
A link between gait improvement resulting from CSF drainage and sagittal sinus measurements indicates that the sagittal sinus may play a role in the manifestation of symptoms in iNPH. This may have implications for the diagnosis of iNPH and potentially inform clinical decision making regarding surgical intervention.



Similar content being viewed by others
References
Hakim S, Adams R (1965) The special clinical problem of symptomatic hydrocephalus with normal cerebrospinal fluid pressure. Observations on cerebrospinal fluid hydrodynamics. J Neurol Sci 2(4):307–327
Klinge P, Marmarou A, Bergsneider M, Relkin N, Black PM (2005) Outcome of shunting in idiopathic normal-pressure hydrocephalus and the value of outcome assessment in shunted patients. Neurosurgery 57(3):S2–40–S42–52
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3):S2–4-S2-16
Khan F, Rehman A, Shamim MS, Bari ME (2015) Factors affecting ventriculoperitoneal shunt survival in adult patients. Surg Neurol Int 6:25. https://doi.org/10.4103/2152-7806.151388
Verres M, Selman W (2004) Management of normal pressure hydrocephalus. Am Fam Physician 70(6):1071–1078
Bergsneider M, Black PM, Klinge P, Marmarou A, Relkin N (2005) Surgical management of idiopathic normal-pressure hydrocephalus. Neurosurgery 57(3):S2–29–S22–39
Ravdin LD, Katzen HL, Jackson AE, Tsakanikas D, Assuras S, Relkin NR (2008) Features of gait most responsive to tap test in normal pressure hydrocephalus. Clin Neurol Neurosurg 110(5):455–461
Mirzayan M, Luetjens G, Borremans J, Regel J (2010) Extended long term (>5 years) outcome of cerebrospinal fluid shunting in idiopathic normal pressure hydrocephalus. Neurosurgery 67(2):295–301
Bateman G (2004) The role of altered impedance in the pathophysiology of normal pressure hydrocephalus, Alzheimer’s disease and syringomyelia. Med Hypotheses 63:980–985
Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM (2005) The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. In: Neurosurgery 57 (3):S2–17-S12–28, vol 57, pp S2-17–S2-28
Daroff R, Fenichel G, Jankovic J, Mazziotta J (2012) Brain edema and disorders of cerebrospinal fluid circulation. In: Rosenberg G (ed) Bradley’s neurology in clinical practice, vol 6. Elsevier, Philadelphia, pp 1393–1395
Czosnyka Z, Owler B, Keong N (2011) Impact of duration of symptoms on CSF dynamics in idiopathic normal pressure hydrocephalus. Acta Neurol Scand 123:414–418
Portnoy HD, Branch C, Castro ME (1994) The relationship of intracranial venous pressure to hydrocephalus. Childs Nerv Syst 10(1):29–35. https://doi.org/10.1007/bf00313582
Graff-Radford NR, Godersky JC (1987) Idiopathic normal pressure hydrocephalus and systemic hypertension. Neurology 37:868–871
Israelsson H, Carlberg B, Wikkelsö C, Laurell K, Kahlon B, Leijon G, Eklund A, Malm J (2017) Vascular risk factors in INPH. A prospective case-control study (the INPH-CRasH study). Neurology 88(6):577–585. https://doi.org/10.1212/wnl.0000000000003583
Krauss JK, Regel JP, Vach W, Droste DW, Borremans JJ, Mergner T (1996) Vascular risk factors and arteriosclerotic disease in idiopathic normal-pressure hydrocephalus of the elderly. Stroke 27:24–29
Silverberg G, Mayo M, Saul T, Rubenstien E, McGuire D (2003) Alzheimer's disease, normal pressure hydrocephalus, and senescent changes in CSF circulatory physiology: a hypothesis. Lancet Neurol 2:506–511
Bateman G (2010) Hyperemic hydrocephalus: a new form of childhood hydrocephalus analogous to hyperemic intracranial hypertension in adults. J Neurosurg: Paediatrics 5(1):20–26
Bateman G, Napier B (2011) External hydrocephalus in infants: six cases with MR venogram and flow quantification correlation. Childs Nerv Syst 27(12):2087–2096. https://doi.org/10.1007/s00381-011-1549-z
Shulmann K, Ransohoff J (1965) Sagittal sinus venous pressure in hydrocephalus. J Neurosurg 23(2):169–173
Bateman GA (2002) Vascular hydraulics associated with idiopathic and secondary intracranial hypertension. Am J Neuroradiol 23(7):1180–1186
Bateman G (2002) Pulse-wave encephalopathy: a comparative study of the hydrodynamics of leukoaraiosis and normal-pressure hydrocephalus. Neuroradiology 44(9):740–747
Al-Zain FT, Rademacher G, Lemcke J, Mutze J, Meier U (2007) Idiopathic normal-pressure hydrocephalus. Flow measurement of cerebrospinal fluid using phase contrast MRI and its diagnostics importance. Nervenarzt 78(2):181–187. https://doi.org/10.1007/s00115-006-2231-7
Bradley WG Jr, Scalzo D, Queralt J, Nitz WN, Atkinson DJ, Wong P (1996) Normal-pressure hydrocephalus: evaluation with cerebrospinal fluid flow measurements at MR imaging. Radiology 198(2):523–529. https://doi.org/10.1148/radiology.198.2.8596861
Halperin J, Kurlan R, Schwalb J, Cusimano M, Gronseth G, Gloss D (2015) Practice guideline: idiopathic normal pressure hydrocephalus: response to shunting and predictors of response. Neurology 85:2063–2071
Golomb J, Wisoff J, Miller DC, Boksay I, Kluger A, Weiner H, Salton J, Graves W (2000) Alzheimer’s disease comorbidity in normal pressure hydrocephalus: prevalence and shunt response. J Neurol Neurosurg Psychiatry 68(6):778–781. https://doi.org/10.1136/jnnp.68.6.778
Ogino A, Kazui H, Miyoshi N, Hashimoto M, Ohkawa S (2006) Cognitive impairment in patients with idiopathic normal pressure hydrocephalus. Dement Geriatr Cogn Disord 21:113–119
Feick D, Sickmond J, Liu L, Metellus P (2008) Sensitivity and predictive value of occupational and physical therapy assessments in the functional evaluation of patients with suspected normal pressure hydrocephalus. J Rehabil Med 40:715–720
Virhammar J, Cesarini KG, Laurell K (2012) The CSF tap test in normal pressure hydrocephalus: evaluation time, reliability and the influence of pain. Eur J Neurol 19(2):271–276
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52:775–809
Gallagher R, Marquez J, Osmotherly P (2018) Gait and balance measures can identify change from a cerebrospinal fluid tap test in idiopathic normal pressure hydrocephalus. Arch Phys Med Rehabil 99(11):2244–2250. https://doi.org/10.1016/j.apmr.2018.03.018
Gallagher R, Marquez J, Osmotherly P (2018) Clinimetric properties and minimally clinically important differences for a battery of mobility, balance and cognitive tests for normal pressure hydrocephalus. Neurosurgery Published ahead of print. https://doi.org/10.1093/neuros/nyy286
Ringstad G, Emblem KE, Geier O, Alperin N, Eide PK (2015) Aqueductal stroke volume: comparisons with intracranial pressure scores in idiopathic normal pressure hydrocephalus. AJNR Am J Neuroradiol 36(9):1623–1630. https://doi.org/10.3174/ajnr.A4340
El Sankari S, Fichten A, Gondry-Jouet C, Czosnyka M, Legars D, Deramond H, Baledent O (2012) Correlation between tap test and CSF aqueductal stroke volume in idiopathic normal pressure hydrocephalus. Acta Neurochir Suppl 113:43–46
Acknowledgements
John Hunter Hospital Physiotherapy, Neurosurgery, Neurology and Radiology Departments.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Hunter New England Human Research Ethics Committee approved this study. All participants gave written informed consent prior to data collection beginning. Reference: 13/06/19/4.02.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gallagher, R., Bateman, G., Marquez, J. et al. Are gait changes linked to CSF flow changes in the sagittal sinus?. Neuroradiology 61, 659–666 (2019). https://doi.org/10.1007/s00234-019-02192-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-019-02192-2