Abstract
Introduction
Haemorrhagic transformation of acute ischemic stroke (AIS) and particularly parenchymal haemorrhage (PH) remains a feared complication of intravenous thrombolysis (IVT). We aimed to identify clinical and perfusion CT (PCT) variables which are independently associated with PHs.
Methods
In this observational cohort study, based on the Acute Stroke Registry Analysis of Lausanne (ASTRAL) from 2003 to December 2013, we selected patients with AIS involving the middle cerebral artery (MCA) territory who were thrombolysed within 4.5 h of symptoms’ onset and who had a good quality baseline PCT at the beginning of IVT. In addition to demographic, clinical, laboratory and non-contrast CT data, volumes of salvageable tissue and ischemic core on PCT, as well as absolute CBF and CBV values within the ischemic regions were compared in patients with and without PH in multivariate analysis.
Results
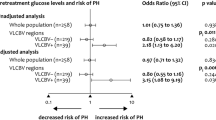
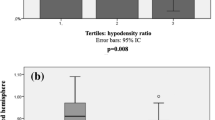
Of the 190 included patients, 24 (12.6%) presented a PH (11 had PH1 and 13 had PH2). In multivariate analysis of the clinical and radiological variables, the lowest CBV in the core and lower body weight was both significantly associated with PH (p = 0.009 and p = 0.024, respectively).
Conclusion
In thrombolysed MCA strokes, maximal hypoperfusion severity depicted by lowest CBV values in the core region and lower body weight are independently correlated with PH. This information, if confirmed in other case series, may add to the stratification of revascularisation decisions in patients with a perceived high PH risk.
Similar content being viewed by others
References
Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) N Engl J Med 333 (24):1581–1587. doi:10.1056/NEJM199512143332401
Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, Boysen G, Bluhmki E, Hoxter G, Mahagne MH et al (1995) Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA 274(13):1017–1025
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, Investigators E (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359(13):1317–1329. doi:10.1056/NEJMoa0804656
Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, Caso V, Micheli S, Bertolani L, Venti M, Palmerini F, Biagini S, Comi G, Previdi P, Silvestrelli G (2008) Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke 39(8):2249–2256. doi:10.1161/STROKEAHA.107.510321
Larrue V, von Kummer RR, Muller A, Bluhmki E (2001) Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke 32(2):438–441
Thomalla G, Sobesky J, Kohrmann M, Fiebach JB, Fiehler J, Zaro Weber O, Kruetzelmann A, Kucinski T, Rosenkranz M, Rother J, Schellinger PD (2007) Two tales: hemorrhagic transformation but not parenchymal hemorrhage after thrombolysis is related to severity and duration of ischemia: MRI study of acute stroke patients treated with intravenous tissue plasminogen activator within 6 hours. Stroke 38(2):313–318. doi:10.1161/01.STR.0000254565.51807.22
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, Grotta J, Howard G, Kaste M, Koga M, von Kummer R, Lansberg M, Lindley RI, Murray G, Olivot JM, Parsons M, Tilley B, Toni D, Toyoda K, Wahlgren N, Wardlaw J, Whiteley W, del Zoppo GJ, Baigent C, Sandercock P, Hacke W, Stroke Thrombolysis Trialists’ Collaborative G (2014) Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384(9958):1929–1935. doi:10.1016/S0140-6736(14)60584-5
Wardlaw JM, Murray V, Berge E, del Zoppo GJ (2014) Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 7:CD000213. doi:10.1002/14651858.CD000213.pub3
Wahlgren N, Ahmed N, Davalos A, Hacke W, Millan M, Muir K, Roine RO, Toni D, Lees KR, investigators S (2008) Thrombolysis with alteplase 3–4.5 h after acute ischaemic stroke (SITS-ISTR): an observational study. Lancet 372(9646):1303–1309. doi:10.1016/S0140-6736(08)61339-2
Anderson CS, Robinson T, Lindley RI, Arima H, Lavados PM, Lee TH, Broderick JP, Chen X, Chen G, Sharma VK, Kim JS, Thang NH, Cao Y, Parsons MW, Levi C, Huang Y, Olavarria VV, Demchuk AM, Bath PM, Donnan GA, Martins S, Pontes-Neto OM, Silva F, Ricci S, Roffe C, Pandian J, Billot L, Woodward M, Li Q, Wang X, Wang J, Chalmers J, Investigators E, Coordinators (2016) Low-dose versus standard-dose intravenous alteplase in acute ischemic stroke. N Engl J Med. doi:10.1056/NEJMoa1515510
Lou M, Safdar A, Mehdiratta M, Kumar S, Schlaug G, Caplan L, Searls D, Selim M (2008) The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology 71(18):1417–1423. doi:10.1212/01.wnl.0000330297.58334.dd
Strbian D, Engelter S, Michel P, Meretoja A, Sekoranja L, Ahlhelm FJ, Mustanoja S, Kuzmanovic I, Sairanen T, Forss N, Cordier M, Lyrer P, Kaste M, Tatlisumak T (2012) Symptomatic intracranial hemorrhage after stroke thrombolysis: the SEDAN score. Ann Neurol 71(5):634–641. doi:10.1002/ana.23546
Mazya M, Egido JA, Ford GA, Lees KR, Mikulik R, Toni D, Wahlgren N, Ahmed N, Investigators S (2012) Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: safe Implementation of Treatments in Stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke 43(6):1524–1531. doi:10.1161/STROKEAHA.111.644815
Asuzu D, Nystrom K, Amin H, Schindler J, Wira C, Greer D, Chi NF, Halliday J, Sheth KN (2015) TURN: a simple predictor of symptomatic intracerebral hemorrhage after IV thrombolysis. Neurocrit Care 23(2):166–171. doi:10.1007/s12028-015-0131-z
Strbian D, Michel P, Seiffge DJ, Saver JL, Numminen H, Meretoja A, Murao K, Weder B, Forss N, Parkkila AK, Eskandari A, Cordonnier C, Davis SM, Engelter ST, Tatlisumak T (2014) Symptomatic intracranial hemorrhage after stroke thrombolysis: comparison of prediction scores. Stroke 45(3):752–758. doi:10.1161/STROKEAHA.113.003806
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS study group. Alberta Stroke Programme Early CT Score. Lancet 355(9216):1670–1674
Demchuk AM, Hill MD, Barber PA, Silver B, Patel SC, Levine SR, Ninds rtPa Stroke Study Group NIH (2005) Importance of early ischemic computed tomography changes using ASPECTS in NINDS rtPA Stroke Study. Stroke 36(10):2110–2115. doi:10.1161/01.STR.0000181116.15426.58
Jain AR, Jain M, Kanthala AR, Damania D, Stead LG, Wang HZ, Jahromi BS (2013) Association of CT perfusion parameters with hemorrhagic transformation in acute ischemic stroke. AJNR Am J Neuroradiol 34(10):1895–1900. doi:10.3174/ajnr.A3502
Hermitte L, Cho TH, Ozenne B, Nighoghossian N, Mikkelsen IK, Ribe L, Baron JC, Ostergaard L, Derex L, Hjort N, Fiehler J, Pedraza S, Hermier M, Maucort-Boulch D, Berthezene Y (2013) Very low cerebral blood volume predicts parenchymal hematoma in acute ischemic stroke. Stroke 44(8):2318–2320. doi:10.1161/STROKEAHA.113.001751
Campbell BC, Christensen S, Parsons MW, Churilov L, Desmond PM, Barber PA, Butcher KS, Levi CR, De Silva DA, Lansberg MG, Mlynash M, Olivot JM, Straka M, Bammer R, Albers GW, Donnan GA, Davis SM, Epithet ID (2013) Advanced imaging improves prediction of hemorrhage after stroke thrombolysis. Ann Neurol 73(4):510–519. doi:10.1002/ana.23837
Mlynash M, Lansberg MG, De Silva DA, Lee J, Christensen S, Straka M, Campbell BC, Bammer R, Olivot JM, Desmond P, Donnan GA, Davis SM, Albers GW, Investigators D-E (2011) Refining the definition of the malignant profile: insights from the DEFUSE-EPITHET pooled data set. Stroke 42(5):1270–1275. doi:10.1161/STROKEAHA.110.601609
Albers GW, Thijs VN, Wechsler L, Kemp S, Schlaug G, Skalabrin E, Bammer R, Kakuda W, Lansberg MG, Shuaib A, Coplin W, Hamilton S, Moseley M, Marks MP, Investigators D (2006) Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol 60(5):508–517. doi:10.1002/ana.20976
Kim JH, Bang OY, Liebeskind DS, Ovbiagele B, Kim GM, Chung CS, Lee KH, Saver JL, Collaborators UC-SS (2010) Impact of baseline tissue status (diffusion-weighted imaging lesion) versus perfusion status (severity of hypoperfusion) on hemorrhagic transformation. Stroke 41(3):e135–e142. doi:10.1161/STROKEAHA.109.563122
Campbell BC, Christensen S, Butcher KS, Gordon I, Parsons MW, Desmond PM, Barber PA, Levi CR, Bladin CF, De Silva DA, Donnan GA, Davis SM, Investigators E (2010) Regional very low cerebral blood volume predicts hemorrhagic transformation better than diffusion-weighted imaging volume and thresholded apparent diffusion coefficient in acute ischemic stroke. Stroke 41(1):82–88. doi:10.1161/STROKEAHA.109.562116
Singer OC, Humpich MC, Fiehler J, Albers GW, Lansberg MG, Kastrup A, Rovira A, Liebeskind DS, Gass A, Rosso C, Derex L, Kim JS, Neumann-Haefelin T, Investigators MRSSG (2008) Risk for symptomatic intracerebral hemorrhage after thrombolysis assessed by diffusion-weighted magnetic resonance imaging. Ann Neurol 63(1):52–60. doi:10.1002/ana.21222
Yassi N, Parsons MW, Christensen S, Sharma G, Bivard A, Donnan GA, Levi CR, Desmond PM, Davis SM, Campbell BC (2013) Prediction of poststroke hemorrhagic transformation using computed tomography perfusion. Stroke 44(11):3039–3043. doi:10.1161/STROKEAHA.113.002396
Hom J, Dankbaar JW, Soares BP, Schneider T, Cheng SC, Bredno J, Lau BC, Smith W, Dillon WP, Wintermark M (2011) Blood-brain barrier permeability assessed by perfusion CT predicts symptomatic hemorrhagic transformation and malignant edema in acute ischemic stroke. AJNR Am J Neuroradiol 32(1):41–48. doi:10.3174/ajnr.A2244
Leigh R, Jen SS, Hillis AE, Krakauer JW, Barker PB, Stir IVI (2014) Pretreatment blood-brain barrier damage and post-treatment intracranial hemorrhage in patients receiving intravenous tissue-type plasminogen activator. Stroke 45(7):2030–2035. doi:10.1161/STROKEAHA.114.005249
Tanne D, Kasner SE, Demchuk AM, Koren-Morag N, Hanson S, Grond M, Levine SR (2002) Markers of increased risk of intracerebral hemorrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice: the Multicenter rt-PA Stroke Survey. Circulation 105(14):1679–1685
Rha JH, Saver JL (2007) The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38(3):967–973. doi:10.1161/01.STR.0000258112.14918.24
Nogueira RG, Gupta R, Jovin TG, Levy EI, Liebeskind DS, Zaidat OO, Rai A, Hirsch JA, Hsu DP, Rymer MM, Tayal AH, Lin R, Natarajan SK, Nanda A, Tian M, Hao Q, Kalia JS, Chen M, Abou-Chebl A, Nguyen TN, Yoo AJ (2015) Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: a multicenter retrospective analysis of 1122 patients. J Neurointerv Surg 7(1):16–21. doi:10.1136/neurintsurg-2013-010743
Michel P, Odier C, Rutgers M, Reichhart M, Maeder P, Meuli R, Wintermark M, Maghraoui A, Faouzi M, Croquelois A, Ntaios G (2010) The Acute Stroke Registry and Analysis of Lausanne (ASTRAL): design and baseline analysis of an ischemic stroke registry including acute multimodal imaging. Stroke 41(11):2491–2498. doi:10.1161/STROKEAHA.110.596189
Ringelstein EB, Chamorro A, Kaste M, Langhorne P, Leys D, Lyrer P, Thijs V, Thomassen L, Toni D, Committee ESOSUC (2013) European Stroke Organisation recommendations to establish a stroke unit and stroke center. Stroke 44(3):828–840. doi:10.1161/STROKEAHA.112.670430
European Stroke Organisation Executive C, Committee ESOW (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25(5):457–507. doi:10.1159/000131083
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24(1):35–41
Puetz V, Dzialowski I, Hill MD, Demchuk AM (2009) The Alberta Stroke Program Early CT Score in clinical practice: what have we learned? Int J Stroke 4(5):354–364. doi:10.1111/j.1747-4949.2009.00337.x
Wintermark M, Albers GW, Alexandrov AV, Alger JR, Bammer R, Baron JC, Davis S, Demaerschalk BM, Derdeyn CP, Donnan GA, Eastwood JD, Fiebach JB, Fisher M, Furie KL, Goldmakher GV, Hacke W, Kidwell CS, Kloska SP, Kohrmann M, Koroshetz W, Lee TY, Lees KR, Lev MH, Liebeskind DS, Ostergaard L, Powers WJ, Provenzale J, Schellinger P, Silbergleit R, Sorensen AG, Wardlaw J, Wu O, Warach S (2008) Acute stroke imaging research roadmap. Stroke 39(5):1621–1628. doi:10.1161/STROKEAHA.107.512319
Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M (2007) Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol 61(6):533–543. doi:10.1002/ana.21130
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, Larrue V, Bluhmki E, Davis S, Donnan G, Schneider D, Diez-Tejedor E, Trouillas P (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 352(9136):1245–1251
Vanacker P, Lambrou D, Eskandari A, Maeder P, Meuli R, Ntaios G, Michel P (2014) Improving prediction of recanalization in acute large-vessel occlusive stroke. J Thromb Haemost 12(6):814–821. doi:10.1111/jth.12561
Vanacker P, Heldner MR, Seiffge D, Mueller H, Eskandari A, Traenka C, Ntaios G, Mosimann PJ, Sztajzel R, Mendes Pereira V, Cras P, Engelter S, Lyrer P, Fischer U, Lambrou D, Arnold M, Michel P (2015) ASTRAL-R score predicts non-recanalisation after intravenous thrombolysis in acute ischaemic stroke. Thromb Haemost 113(5):1121–1126. doi:10.1160/TH14-06-0482
Blennow K, Wallin A, Uhlemann C, Gottfries CG (1991) White-matter lesions on CT in Alzheimer patients: relation to clinical symptomatology and vascular factors. Acta Neurol Scand 83(3):187–193
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Willer L, Havsteen I, Ovesen C, Christensen AF, Christensen H (2015) Computed tomography-verified leukoaraiosis is a risk factor for post-thrombolytic hemorrhage. J Stroke Cerebrovasc Dis 24(6):1126–1130. doi:10.1016/j.jstrokecerebrovasdis.2014.12.018
Shi ZS, Loh Y, Liebeskind DS, Saver JL, Gonzalez NR, Tateshima S, Jahan R, Feng L, Vespa PM, Starkman S, Salamon N, Villablance JP, Ali LK, Ovbiagele B, Kim D, Vinuela F, Duckwiler GR (2012) Leukoaraiosis predicts parenchymal hematoma after mechanical thrombectomy in acute ischemic stroke. Stroke 43(7):1806–1811. doi:10.1161/STROKEAHA.111.649152
Palumbo V, Boulanger JM, Hill MD, Inzitari D, Buchan AM, Investigators C (2007) Leukoaraiosis and intracerebral hemorrhage after thrombolysis in acute stroke. Neurology 68(13):1020–1024. doi:10.1212/01.wnl.0000257817.29883.48
Molina CA, Montaner J, Abilleira S, Ibarra B, Romero F, Arenillas JF, Alvarez-Sabin J (2001) Timing of spontaneous recanalization and risk of hemorrhagic transformation in acute cardioembolic stroke. Stroke 32(5):1079–1084
Fisher M, Adams RD (1951) Observations on brain embolism with special reference to the mechanism of hemorrhagic infarction. J Neuropathol Exp Neurol 10(1):92–94
Kim CK, Ryu WS, Kim BJ, Lee SH (2013) Paradoxical effect of obesity on hemorrhagic transformation after acute ischemic stroke. BMC Neurol 13:123. doi:10.1186/1471-2377-13-123
Sarikaya H, Arnold M, Engelter ST, Lyrer PA, Mattle HP, Michel P, Odier C, Weder B, Siebel P, Mueller F, Ballinari P, Georgiadis D, Baumgartner RW (2011) Outcome of intravenous thrombolysis in stroke patients weighing over 100 kg. Cerebrovasc Dis 32(3):201–206. doi:10.1159/000328813
Gensicke H, Wicht A, Bill O, Zini A, Costa P, Kagi G, Stark R, Seiffge DJ, Traenka C, Peters N, Bonati LH, Giovannini G, De Marchis GM, Poli L, Polymeris A, Vanacker P, Sarikaya H, Lyrer PA, Pezzini A, Vandelli L, Michel P, Engelter ST, Thrombolysis in Stroke Patients c (2016) Impact of body mass index on outcome in stroke patients treated with intravenous thrombolysis. Eur J Neurol. doi:10.1111/ene.13071
Acknowledgements
This study was supported in part by the Swiss Heart Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that the analysis of clinical and patient data retrieved from the Acute Stroke Registry Analysis of Lausanne (ASTRAL) has been approved by the Ethics Commission for Research on Humans of the Canton of Vaud (ECCV).
Conflict of interest
PM has received research grants from the Swiss Heart Foundation; speaker fees from Boehringer-Ingelheim, Bayer, Medtronic-Covidien and Stryker; honoraria from scientific advisory boards from Boehringer-Ingelheim, Bayer and Pfizer; consulting fees from Pierre-Fabre, Astra-Zeneca and Amgen; and travel support from Boehringer-Ingelheim and Bayer. All financial support is received by the institution (CHUV) and used for stroke education and research.
Rights and permissions
About this article
Cite this article
Tsetsou, S., Amiguet, M., Eskandari, A. et al. Severe cerebral hypovolemia on perfusion CT and lower body weight are associated with parenchymal haemorrhage after thrombolysis. Neuroradiology 59, 23–29 (2017). https://doi.org/10.1007/s00234-016-1775-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1775-x