Abstract
Introduction
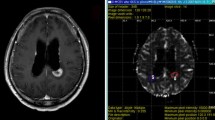
High spatial resolution of dynamic contrast-enhanced (DCE) MR imaging allows characterization of heterogenous tumor microenvironment. Our purpose was to determine which is the best advanced MR imaging protocol, focused on additional MR perfusion method, for predicting recurrent metastatic brain tumor following gamma-knife radiosurgery (GKRS).
Methods
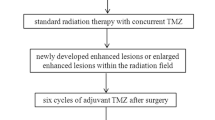
Seventy-two consecutive patients with post-GKRS metastatic brain tumor were enrolled. Two readers independently calculated the percentile histogram cutoffs for normalized cerebral blood volume (nCBV) from dynamic susceptibility contrast (DSC) imaging and initial area under the time signal-intensity curve (IAUC) from DCE imaging, respectively. Area under the receiver operating characteristic curve (AUC) and interreader agreement were assessed.
Results
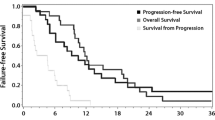
For differentiating tumor recurrence from therapy effect, adding DCE imaging to diffusion-weighted imaging (DWI) significantly improved AUC from 0.79 to 0.95 for reader 1 and from 0.80 to 0.96 for reader 2, respectively. There was no significant difference of AUC between the combination of DWI with DSC imaging and the combination of DWI with DCE imaging for both readers. With the combination of DWI and DCE imaging, the sensitivity and specificity were 86.7 and 88.1 % for reader 1 and 90.0 and 85.7 % for reader 2, respectively. The intraclass correlation coefficient (ICC) between readers was highest for calculation of the 90th percentile histogram cutoffs for IAUC (ICC, 0.87).
Conclusion
Adding perfusion MR imaging to DWI significantly improves the prediction of recurrent metastatic tumor; however, the diagnostic performance is not affected by selection of either DSC or DCE MR perfusion method.






Similar content being viewed by others
References
Mintz A, Perry J, Spithoff K, Chambers A, Laperriere N (2007) Management of single brain metastasis: a practice guideline. Curr Oncol 14:131–143
Dooms GC, Hecht S, Brant-Zawadzki M, Berthiaume Y, Norman D, Newton TH (1986) Brain radiation lesions: MR imaging. Radiology 158:149–155
Barajas RF, Chang JS, Sneed PK, Segal MR, McDermott MW, Cha S (2009) Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 30:367–372
Essig M, Waschkies M, Wenz F, Debus J, Hentrich HR, Knopp MV (2003) Assessment of brain metastases with dynamic susceptibility-weighted contrast-enhanced MR imaging: initial results. Radiology 228:193–199
Gasparetto EL, Pawlak MA, Patel SH et al (2009) Posttreatment recurrence of malignant brain neoplasm: accuracy of relative cerebral blood volume fraction in discriminating low from high malignant histologic volume fraction. Radiology 250:887–896
Huang J, Wang AM, Shetty A et al (2011) Differentiation between intra-axial metastatic tumor progression and radiation injury following fractionated radiation therapy or stereotactic radiosurgery using MR spectroscopy, perfusion MR imaging or volume progression modeling. Magn Reson Imaging 29:993–1001
Mitsuya K, Nakasu Y, Horiguchi S et al (2010) Perfusion weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. J Neurooncol 99:81–88
Roberts C, Issa B, Stone A, Jackson A, Waterton JC, Parker GJ (2006) Comparative study into the robustness of compartmental modeling and model-free analysis in DCE-MRI studies. J Magn Reson Imaging 23:554–563
Hawighorst H, Weikel W, Knapstein PG et al (1998) Angiogenic activity of cervical carcinoma: assessment by functional magnetic resonance imaging-based parameters and a histomorphological approach in correlation with disease outcome. Clin Cancer Res 4:2305–2312
Mayr NA, Yuh WT, Zheng J et al (1998) Prediction of tumor control in patients with cervical cancer: analysis of combined volume and dynamic enhancement pattern by MR imaging. AJR Am J Roentgenol 170:177–182
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Gossmann A, Helbich TH, Kuriyama N et al (2002) Dynamic contrast-enhanced magnetic resonance imaging as a surrogate marker of tumor response to anti-angiogenic therapy in a xenograft model of glioblastoma multiforme. J Magn Reson Imaging 15:233–240
Aronen HJ, Gazit IE, Louis DN et al (1994) Cerebral blood volume maps of gliomas: comparison with tumor grade and histologic findings. Radiology 191:41–51
Narang J, Jain R, Arbab AS et al (2011) Differentiating treatment-induced necrosis from recurrent/progressive brain tumor using nonmodel-based semiquantitative indices derived from dynamic contrast-enhanced T1-weighted MR perfusion. Neuro Oncol 13:1037–1046
Bisdas S, Naegele T, Ritz R et al (2011) Distinguishing recurrent high-grade gliomas from radiation injury: a pilot study using dynamic contrast-enhanced MR imaging. Acad Radiol 18:575–583
Boxerman JL, Schmainda KM, Weisskoff RM (2006) Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 27:859–867
Johnson G, Wetzel SG, Cha S, Babb J, Tofts PS (2004) Measuring blood volume and vascular transfer constant from dynamic, T (2)*-weighted contrast-enhanced MRI. Magn Reson Med 51:961–968
Donahue KM, Krouwer HG, Rand SD et al (2000) Utility of simultaneously acquired gradient-echo and spin-echo cerebral blood volume and morphology maps in brain tumor patients. Magn Reson Med 43:845–853
Quarles CC, Gore JC, Xu L, Yankeelov TE (2012) Comparison of dual-echo DSC-MRI- and DCE-MRI-derived contrast agent kinetic parameters. Magn Reson Imaging 30:944–953
Paulson ES, Schmainda KM (2008) Comparison of dynamic susceptibility-weighted contrast-enhanced MR methods: recommendations for measuring relative cerebral blood volume in brain tumors. Radiology 249:601–613
Kim HS, Ju Goh M, Kim N, Choi CG, Kim SJ, Kim JH (2014) Which combination of MR imaging modalities is best for predicting recurrent glioblastoma? Study of diagnostic accuracy and reproducibility. Radiology 30:1328–1268
Chung WJ, Kim HS, Kim N, Choi CG, Kim SJ (2013) Recurrent glioblastoma: optimum area under the curve method derived from dynamic contrast-enhanced T1-weighted perfusion MR imaging. Radiology 269:561–568
Suh CH, Kim HS, Choi YJ, Kim N, Kim SJ (2013) Prediction of pseudoprogression in patients with glioblastomas using the initial and final area under the curves ratio derived from dynamic contrast-enhanced T1-weighted perfusion MR imaging. AJNR Am J Neuroradiol 34:2278–2286
Evelhoch JL, LoRusso PM, He Z et al (2004) Magnetic resonance imaging measurements of the response of murine and human tumors to the vascular-targeting agent ZD6126. Clin Cancer Res 10:3650–3657
Boxerman JL, Schmainda KM, Weisskoff RM (2006) Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 27:859–867
Acknowledgments
This study was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (grant number: 2011-0002629).
Ethical standards and patient consent
We declare that all human studies have been approved by the local Institutional Review Board and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Patient consent was waived due to the retrospective nature of the study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koh, M.J., Kim, H.S., Choi, C.G. et al. Which is the best advanced MR imaging protocol for predicting recurrent metastatic brain tumor following gamma-knife radiosurgery: focused on perfusion method. Neuroradiology 57, 367–376 (2015). https://doi.org/10.1007/s00234-015-1485-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-015-1485-9