Abstract
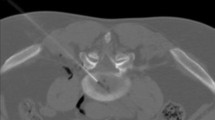
Spontaneous regression of lumbar disk herniation in patients who did not undergo surgery nor interventional therapy is reported in up to 70% of cases; however, no perspective study has clarified the possible predictive signs of a positive evolution. Aim of our study was to search for plan and contrast enhancement MRI signs able to define disk-herniation resolution. We enrolled 64 patients, affected by 72 lumbar disk herniations as per the classification proposed by the American Society of Neuroradiology (Nomenclature and Classification of Lumbar Disk Pathology 2001). MRI examinations were performed by 1.5-T magnet, using T1w SE sequences on sagittal and axial planes, before and after contrast, and T2w FSE ones on the same planes. The following parameters were considered: age, sex, level and size of disk herniation, its relationship to the spinal canal, clinical onset interval, type of disk herniation, herniated-material signal intensity on T2w sequences and its pattern of contrast enhancement. All the patients, conservatively treated, underwent clinical and MRI follow-up examination after 6 months. At MRI follow-up exams spontaneous regression of disk herniation was observed in 34.72% of cases. Among these, free fragments regressed in 100% of cases, herniations with high signal intensity on T2w sequences in 85.18%, herniations with peripheral contrast-enhancement in 83% of cases. Disk-herniation evolution did not show any relationship with location, size and level. Our study demonstrates that MRI, in addition to its high diagnostic value, offers predictive information about disk-herniation evolution.








Similar content being viewed by others
References
Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R (1992) Lumbar disk herniation: MR imaging assessment of natural history in patient treated without surgery. Radiology 185:135–141
Hsu K, Zucherman J, Shea W et al (1990) Lumbar disk degeneration. Incidence and etiology. Spine 15:679–682
Bangert BA, Modic MT, Ross JS et al (1995) Hyperintense disks on T1-weighted MR images: correlation with calcification. Radiology 195:437–443
Kawaji Y, Uchiyama S, Yagi E (2001) Three-dimensional evaluation of lumbar disc hernia and prediction of absorption by enhanced MRI. J Orthop Sci 6:498–502
Jevtic V (2001) MRI appearance of different discovertebral lesions. Europ Radiol 11:1123–1135
Saal JA, Saal JS (1990) The natural history of lumbar intervertebral disk extrusion treated nonoperatively. Spine 15:683–686
Bush K, Cowan N, Katz DE, Gishen P (1992) The natural history of sciatica associated with disk pathology. A prospective study with clinical and independent radiologic follow-up. Spine 17:1205–1212
Gallucci M, Bozzao A, Orlandi B, Manetta R (1995) Follow-up of surgically treated and untreated disk pathology. Riv Neurorad 8:85–96
Davis AR (1994) A long-term outcome analysis of 984 surgically-treated herniated lumbar disks. J Neurosurg 80:415–421
Komori H, Okawa A, Haro H et al (1998) Contrast enhancement MRI in conservative management of lumbar disk herniation. Spine 23:67–73
Eerens I, Demaerel P, Haven F et al (2001) Imaging characteristics of non-contained migrating disk fragment and cyst. Eur Radiol 11:854–857
Fardon DF, Milette PC et al (2001) Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine 26:E93-E113
Anderson GBJ, Pope MH (eds) (1984) Occupational low back pain. Praeger, New York
Saifuddin A, Mitchel R, Taylor BA (1999) Extradural inflammation associated with annular tear: demonstration with gadolinium-enhancement lumbar spine MRI. Eur Spine J 8:34–39
Mc Carrow, Wimpee MW, Hudkins P (1987) The inflammatory effect of nucleus pulposus. A possible element in the pathogenesis of low back pain. Spine 12:760–764
Eysel P, Rompe JD, Schaub T, Meurer A (1994) Value of imaging techniques in the diagnosis of lumbar intervertebral disk prolapse. Z Orthop Ihre Grenzgeb 132:371–376
Pevsner PH, Ondra S, Radcliff W, George El McDonnell D, Furlow T, Dagi T (1986) Magnetic resonance imaging of the lumbar spine. A comparison with computed tomography and myelography. Acta Radiol Suppl 369:706–707
Howe JF, Leser JD, Calvin W (1997) Mechanosensitivity of dorsal root ganglia and chronically-injured axon: a physiological basis for the radicular pain of nerve root compression. Pain 3:25–41
Axel S, Max W, Jurgen S (1996) Degenerative disk vascularization on MRI: correlation with clinical and histopathologic findings. Skeletal Radiol 25:119–126
Yasuma T, Arai K, Yamauchi Y (1993) The histology of intervertebral disk herniation. Spine 18:1761–1765
Gallucci M, Bozzao A, Orlandi B, Manetta R, Brughitta G, Lupattelli L (1995) Does postcontrast MR enhancement in lumbar disk herniation have a prognostic value? J Comput Assist Tomogr 19:34–38
Glickstein MF, Sussman SK (1991) Time-dependent scar enhancement in magnetic resonance imaging of the postoperative lumbar spine. Skeletal Radiol 20:333–337
Tertti M, Paajanen H, Laato M, Aho H, Komu M, Kormanc M (1991) Disk degeneration in magnetic resonance imaging. A comparative biochemical, histologic and radiologic study in cadaver spines. Spine 16:629–634
LeBlanc AD, Schonfeld E, Schneider VS, Evans HJ, Taber KH (1988) The spine: changes in T2 relaxation times from disuse. Radiology 169:105–107
Matsubara Y, Kato F, Mimatsu K et al (1995) Serial changes on MRI in lumbar disk herniations treated conservatively. Neuroradiol 37:378–383
Jinkins JR, Whittemore AR, Bradley WG (1989) The anatomic basis of vertebrogenic pain and the autonomic syndrome associated with lumbar disk extrusion. AJR Am J Roentgenol 152:1277–1289
Lenz GP, Assheuer J, Lenz W, Gottschlich KW (1990) New aspects of lumbar disk disease. MR imaging and histological findings. Arch Orthop Trauma Surg 109:75–82
Acknowledgement
The authors thank Angela Martella for her help in manuscript translation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Splendiani, A., Puglielli, E., De Amicis, R. et al. Spontaneous resolution of lumbar disk herniation: predictive signs for prognostic evaluation. Neuroradiology 46, 916–922 (2004). https://doi.org/10.1007/s00234-004-1232-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-004-1232-0