Abstract
Objective
Several population pharmacokinetic models of tacrolimus in liver transplant patients were built, and their predictability was evaluated in their settings. However, the extrapolation in the prediction was unclear. This study aimed to evaluate the predictive performance of published tacrolimus models in adult liver transplant recipients using data from the Thai population as an external dataset.
Methods
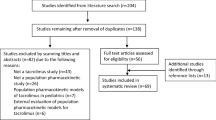
The selected published models were systematically searched and evaluated for their quality. The external dataset of patients who underwent the first liver transplant and received immediate-release tacrolimus was used to assess the predictive performance of each selected model. Trough concentrations between 3 and 6 months were retrospectively collected to evaluate the predictability of each model using prediction-based diagnostics, simulation-based diagnostics, and Bayesian forecasting.
Results
Sixty-seven patients with 360 trough concentrations and eight selected published models were included in this study. None of the models met the predictive precision criteria in prediction-based diagnostics. Meanwhile, four published population pharmacokinetic models showed a normal distribution in NPDE testing. Regarding Bayesian forecasting, all models improved their forecasts with at least one prior information data point.
Conclusion
Bayesian forecasting is more accurate and precise than other testing methods for predicting drug concentrations. However, none of the evaluated models provides satisfactory predictive performance for generalization to Thai liver transplant patients. This underscores the need for future research to develop population PK models tailored to the Thai population. Such efforts should consider the inclusion of nonlinear pharmacokinetics and region-specific factors, including genetic variability, to improve model accuracy and applicability.




Similar content being viewed by others
Data availability
All datasets collected and analyzed are available at reasonable request from the corresponding author.
Code availability
Not applicable.
References
Brunet M, van Gelder T, Åsberg A, Haufroid V, Hesselink DA, Langman L, Lemaitre F, Marquet P, Seger C, Shipkova M, Vinks A, Wallemacq P, Wieland E, Woillard JB, Barten MJ, Budde K, Colom H, Dieterlen MT, Elens L, Johnson-Davis KL, Kunicki PK, MacPhee I, Masuda S, Mathew BS, Millán O, Mizuno T, Moes DAR, Monchaud C, Noceti O, Pawinski T, Picard N, van Schaik R, Sommerer C, Vethe NT, de Winter B, Christians U, Bergan S (2019) Therapeutic drug monitoring of tacrolimus-personalized therapy: second consensus report. Ther Drug Monit 41(3):261–307. https://doi.org/10.1097/ftd.0000000000000640
Venkataramanan R, Jain A, Warty VS, Abu-Elmagd K, Alessiani M, Lever J, Krajak A, Flowers J, Mehta S, Zuckerman S et al (1991) Pharmacokinetics of FK 506 in transplant patients. Transplant Proc 23(6):2736–2740
Venkataramanan R, Swaminathan A, Prasad T, Jain A, Zuckerman S, Warty V, McMichael J, Lever J, Burckart G, Starzl T (1995) Clinical pharmacokinetics of tacrolimus. Clin Pharmacokinet 29(6):404–430. https://doi.org/10.2165/00003088-199529060-00003
Beringer P (2018) Winter’s basic clinical pharmacokinetics. Wolters Kluwer Health, Philadelphia, p 2018
Ette EI, Williams PJ (2004) Population pharmacokinetics I: background, concepts, and models. Ann Pharmacother 38(10):1702–1706. https://doi.org/10.1345/aph.1D374
Antignac M, Hulot JS, Boleslawski E, Hannoun L, Touitou Y, Farinotti R, Lechat P, Urien S (2005) Population pharmacokinetics of tacrolimus in full liver transplant patients: modelling of the post-operative clearance. Eur J Clin Pharmacol 61(5–6):409–416. https://doi.org/10.1007/s00228-005-0933-6
Fukatsu S, Yano I, Igarashi T, Hashida T, Takayanagi K, Saito H, Uemoto S, Kiuchi T, Tanaka K, Inui K, Tanaka K, Inui K (2001) Population pharmacokinetics of tacrolimus in adult recipients receiving living-donor liver transplantation. Eur J Clin Pharmacol 57(6–7):479–484. https://doi.org/10.1007/s002280100331
Sam WJ, Tham LS, Holmes MJ, Aw M, Quak SH, Lee KH, Lim SG, Prabhakaran K, Chan SY, Ho PC (2006) Population pharmacokinetics of tacrolimus in whole blood and plasma in asian liver transplant patients. Clin Pharmacokinet 45(1):59–75. https://doi.org/10.2165/00003088-200645010-00004
Undre NA, Schäfer A (1998) Factors affecting the pharmacokinetics of tacrolimus in the first year after renal transplantation. European Tacrolimus Multicentre Renal Study Group. Transplant Proc 30(4):1261–1263. https://doi.org/10.1016/s0041-1345(98)00234-6
Blanchet B, Duvoux C, Costentin CE, Barrault C, Ghaleh B, Salvat A, Jouault H, Astier A, Tod M, Hulin A (2008) Pharmacokinetic-pharmacodynamic assessment of tacrolimus in liver-transplant recipients during the early post-transplantation period. Ther Drug Monit 30(4):412–418. https://doi.org/10.1097/FTD.0b013e318178e31b
Chen B, Shi HQ, Liu XX, Zhang WX, Lu JQ, Xu BM, Chen H (2017) Population pharmacokinetics and Bayesian estimation of tacrolimus exposure in Chinese liver transplant patients. J Clin Pharm Ther 42(6):679–688. https://doi.org/10.1111/jcpt.12599
Fukudo M, Yano I, Masuda S, Goto M, Uesugi M, Katsura T, Ogura Y, Oike F, Takada Y, Egawa H, Uemoto S, Ki I (2006) Population pharmacokinetic and pharmacogenomic analysis of tacrolimus in pediatric living-donor liver transplant recipients. Clin Pharmacol Ther 80(4):331–345. https://doi.org/10.1016/j.clpt.2006.06.008
Li Z, Fan Q, Zhang N, Zhang C (2007) Population pharmacokinetic estimation of tacrolimus apparent clearance through multiple-linear regression. J Dalian Med Univ 29(6):535–538
Lu Y, Xu L, Cui J, Shen S, Li X (2021) Effects of postoperative day and NR1I2 on tacrolimus clearance in Chinese liver transplant recipients-a population model approach. Clin Pharmacol Drug Dev 10(11):1385–1394. https://doi.org/10.1002/cpdd.971
Lu YX, Su QH, Wu KH, Ren YP, Li L, Zhou TY, Lu W (2015) A population pharmacokinetic study of tacrolimus in healthy Chinese volunteers and liver transplant patients. Acta Pharmacol Sin 36(2):281–288. https://doi.org/10.1038/aps.2014.110
Martial LC, Biewenga M, Ruijter BN, Keizer R, Swen JJ, van Hoek B, Moes D (2021) Population pharmacokinetics and genetics of oral meltdose tacrolimus (Envarsus) in stable adult liver transplant recipients. Br J Clin Pharmacol 87(11):4262–4272. https://doi.org/10.1111/bcp.14842
Oteo I, Lukas JC, Leal N, Suarez E, Valdivieso A, Gastaca M, Ortiz de Urbina J, Calvo R (2013) Tacrolimus pharmacokinetics in the early post-liver transplantation period and clinical applicability via Bayesian prediction. Eur J Clin Pharmacol 69(1):65–74. https://doi.org/10.1007/s00228-012-1300-z
Shao J, Wang C, Fu P, Chen F, Zhang Y, Wei J (2020) Impact of donor and recipient CYP3A5*3 genotype on tacrolimus population pharmacokinetics in Chinese adult liver transplant recipients. Ann Pharmacother 54(7):652–661. https://doi.org/10.1177/1060028019897050
Staatz CE, Willis C, Taylor PJ, Lynch SV, Tett SE (2003) Toward better outcomes with tacrolimus therapy: population pharmacokinetics and individualized dosage prediction in adult liver transplantation. Liver Transpl 9(2):130–137. https://doi.org/10.1053/jlts.2003.50023
Tharanon VSA, Intaraprasong P, Sra-ium S, Sakulchairungrueng B, Gesprasert G, Arpornsujaritkun N (2021) Population pharmacokinetics of tacrolimus in Thai liver transplant patients. Thai Bull Pharm Sci 16(1):17–30
Zhang XQ, Wang ZW, Fan JW, Li YP, Jiao Z, Gao JW, Peng ZH, Liu GL (2012) The impact of sulfonylureas on tacrolimus apparent clearance revealed by a population pharmacokinetics analysis in Chinese adult liver-transplant patients. Ther Drug Monit 34(2):126–133. https://doi.org/10.1097/FTD.0b013e31824a67eb
Zhu L, Wang H, Sun X, Rao W, Qu W, Zhang Y, Sun L (2014) The population pharmacokinetic models of tacrolimus in Chinese adult liver transplantation patients. J Pharm (Cairo) 2014:713650. https://doi.org/10.1155/2014/713650
Cai X, Li R, Sheng C, Tao Y, Zhang Q, Zhang X, Li J, Shen C, Qiu X, Wang Z, Jiao Z (2020) Systematic external evaluation of published population pharmacokinetic models for tacrolimus in adult liver transplant recipients. Eur J Pharm Sci 145:105237. https://doi.org/10.1016/j.ejps.2020.105237
Cheng Y, Wang CY, Li ZR, Pan Y, Liu MB, Jiao Z (2021) Can population pharmacokinetics of antibiotics be extrapolated? Implications of external evaluations Clin Pharmacokinet 60(1):53–68. https://doi.org/10.1007/s40262-020-00937-4
Wang DD, Chen X, Fu M, Zheng QS, Xu H, Li ZP (2020) Model extrapolation to a real-world dataset: evaluation of tacrolimus population pharmacokinetics and drug interaction in pediatric liver transplantation patients. Xenobiotica 50(4):371–379. https://doi.org/10.1080/00498254.2019.1631505
Yoon JL, Cho JJ, Park KM, Noh HM, Park YS (2015) Diagnostic performance of body mass index using the Western Pacific Regional Office of World Health Organization reference standards for body fat percentage. J Korean Med Sci 30(2):162–166. https://doi.org/10.3346/jkms.2015.30.2.162
Mao JJ, Jiao Z, Yun HY, Zhao CY, Chen HC, Qiu XY, Zhong MK (2018) External evaluation of population pharmacokinetic models for ciclosporin in adult renal transplant recipients. Br J Clin Pharmacol 84(1):153–171. https://doi.org/10.1111/bcp.13431
Zahir H, McLachlan AJ, Nelson A, McCaughan G, Gleeson M, Akhlaghi F (2005) Population pharmacokinetic estimation of tacrolimus apparent clearance in adult liver transplant recipients. Ther Drug Monit 27(4):422–430. https://doi.org/10.1097/01.ftd.0000170029.36573.a0
Dansirikul C, Staatz CE, Duffull SB, Taylor PJ, Lynch SV, Tett SE (2004) Sampling times for monitoring tacrolimus in stable adult liver transplant recipients. Ther Drug Monit 26(6):593–599. https://doi.org/10.1097/00007691-200412000-00003
Kourkoumpetis T, Levitsky J (2019) Immunosuppressive drug levels in liver transplant recipients: Impact in decision making. Semin Liver Dis 39(4):414–421. https://doi.org/10.1055/s-0039-1688443
Karlsson MO, Savic RM (2007) Diagnosing model diagnostics. Clin Pharmacol Ther 82(1):17–20. https://doi.org/10.1038/sj.clpt.6100241
Mould DR, D’Haens G, Upton RN (2016) Clinical decision support tools: the evolution of a revolution. Clin Pharmacol Ther 99(4):405–418. https://doi.org/10.1002/cpt.334
Guo T, van Hest RM, Zwep LB, Roggeveen LF, Fleuren LM, Bosman RJ, van der Voort PHJ, Girbes ARJ, Mathot RAA, Elbers PWG, van Hasselt JGC (2020) Optimizing predictive performance of Bayesian forecasting for vancomycin concentration in intensive care patients. Pharm Res 37(9):171. https://doi.org/10.1007/s11095-020-02908-7
Abrantes JA, Jönsson S, Karlsson MO, Nielsen EI (2019) Handling interoccasion variability in model-based dose individualization using therapeutic drug monitoring data. Br J Clin Pharmacol 85(6):1326–1336. https://doi.org/10.1111/bcp.13901
Cai X, Song H, Jiao Z, Yang H, Zhu M, Wang C, Wei D, Shi L, Wu B, Chen J (2020) Population pharmacokinetics and dosing regimen optimization of tacrolimus in Chinese lung transplant recipients. Eur J Pharm Sci. https://doi.org/10.1016/j.ejps.2020.105448
Cai XJ, Li RD, Li JH, Tao YF, Zhang QB, Shen CH, Zhang XF, Wang ZX, Jiao Z (2022) Prospective population pharmacokinetic study of tacrolimus in adult recipients early after liver transplantation: a comparison of Michaelis-Menten and theory-based pharmacokinetic models. Front Pharmacol 13:1031969. https://doi.org/10.3389/fphar.2022.1031969
Zhao CY, Jiao Z, Mao JJ, Qiu XY (2016) External evaluation of published population pharmacokinetic models of tacrolimus in adult renal transplant recipients. Br J Clin Pharmacol 81(5):891–907. https://doi.org/10.1111/bcp.12830
van Schaik RH, van der Heiden IP, van den Anker JN, Lindemans J (2002) CYP3A5 variant allele frequencies in Dutch Caucasians. Clin Chem 48(10):1668–1671
Balram C, Zhou Q, Cheung YB, Lee EJ (2003) CYP3A5*3 and *6 single nucleotide polymorphisms in three distinct Asian populations. Eur J Clin Pharmacol 59(2):123–126. https://doi.org/10.1007/s00228-003-0594-2
Fukuen S, Fukuda T, Maune H, Ikenaga Y, Yamamoto I, Inaba T, Azuma J (2002) Novel detection assay by PCR-RFLP and frequency of the CYP3A5 SNPs, CYP3A5*3 and *6, in a Japanese population. Pharmacogenetics 12(4):331–334. https://doi.org/10.1097/00008571-200206000-00009
Vannaprasaht S, Reungjui S, Supanya D, Sirivongs D, Pongskul C, Avihingsanon Y, Tassaneeyakul W (2013) Personalized tacrolimus doses determined by CYP3A5 Genotype for induction and maintenance phases of kidney transplantation. Clin Ther 35(11):1762–1769. https://doi.org/10.1016/j.clinthera.2013.08.019
Funding
This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Virunya Komenkul, Piyawat Komolmit, and Thitima Wattanavijitkul conducted the study design. Piyawat Komolmit supported the acquisition of the external dataset. Virunya Komenkul and Waroonrat Sukarnjanaset collected and analyzed the data. All authors revised the manuscript independently.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was conducted according to an ethical standard and approved by the Institutional Review Board of the Faculty of Medicine of Chulalongkorn University, Bangkok (IRB No. 0382/65). This study did not involve direct patient contact as it was conducted retrospectively. All data were collected exclusively from medical records.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Virunya Komenkul is the principal investigator.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Komenkul, V., Sukarnjanaset, W., Komolmit, P. et al. External validation of population pharmacokinetic models of tacrolimus in Thai adult liver transplant recipients. Eur J Clin Pharmacol (2024). https://doi.org/10.1007/s00228-024-03692-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00228-024-03692-8