Abstract
Purpose
Inappropriate prescribing (IP) is common among the elderly and is associated with adverse health outcomes. The role of different patterns of IP in clinical practice remains unclear. The aim of this study is to analyse the characteristics of different patterns of IP in hospitalized older adults.
Methods
This is a prospective observational study conducted in the acute care of elderly (ACE) unit of an acute hospital in Barcelona between June and August 2021. Epidemiological and demographic data were collected, and a comprehensive geriatric assessment (CGA) was performed on admitted patients. Four patterns of inappropriate prescribing were identified: extreme polypharmacy (10 or more drugs), potentially inappropriate medications (PIMs), potential prescribing omissions (PPOs) and anticholinergic burden.
Results
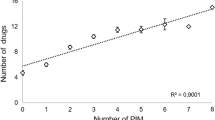
Among 93 admitted patients (51.6% male, mean age of 82.83), the main diagnosis was heart failure (36.6%). Overprescribing patterns (extreme polypharmacy, PIMs, PPOs and anticholinergic burden) were associated with higher comorbidity, increased dependence on instrumental activities of daily living (IADL) and greater prevalence of dementia. Underprescribing (omissions) was associated with important comorbidity, residence in nursing homes, an increased risk of malnutrition, higher social risk and greater frailty. Comparing different patterns of IP, patients with high anticholinergic burden exhibited more extreme polypharmacy and PIMs. In the case of omissions, no association was identified with other IP patterns.
Conclusions
We found statistically significant association between patterns of inappropriate prescribing and clinical and CGA variables such as comorbidity, dependency, dementia or frailty. There is a statistically significant association between patterns of overprescribing among patients admitted to the ACE unit.
Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are available upon reasonable request from the corresponding author.
References
Palmer K, Villani ER, Vetrano DL et al (2019) Association of polypharmacy and hyperpolypharmacy with frailty states: a systematic review and meta-analysis. Eur Geriatr Med 10(1):9–36. https://doi.org/10.1007/s41999-018-0124-5
Martinot P, Landré B, Zins M, Goldberg M, Ankri J, Herr M (2018) Association between potentially inappropriate medications and frailty in the early old age: a longitudinal study in the GAZEL cohort. J Am Med Dir Assoc 19(11):967–973.e3. https://doi.org/10.1016/j.jamda.2018.07.008. Epub 2018 Aug 30. PMID: 30172683.
Gutiérrez-Valencia M, Izquierdo M, Malafarina V et al (2017) Impact of hospitalization in an acute geriatric unit on polypharmacy and potentially inappropriate prescriptions: a retrospective study. Geriatr Gerontol Int 17(12):2354–2360. https://doi.org/10.1111/ggi.13073
Wallace E, McDowell R, Bennett K, Fahey T, Smith SM (2017) Impact of potentially inappropriate prescribing on adverse drug events, health related quality of life and emergency hospital attendance in older people attending general practice: a prospective cohort study. J Gerontol A Biol Sci Med Sci 72(2):271–277. https://doi.org/10.1093/gerona/glw140
Hamilton H, Gallagher P, Ryan C, Byrne S, O’Mahony D (2011) Potentially inappropriate medications defined by STOPP criteria and the risk of adverse drug events in older hospitalized patients. Arch Intern Med 171(11):1013–1019. https://doi.org/10.1001/archinternmed.2011.215
San-José A, Pérez-Bocanegra C, Agustí A et al (2021) Integrated health intervention on polypharmacy and inappropriate prescribing in elderly people with multimorbidity: results at the end of the intervention and at 6 months after the intervention. Med Clin (Barc) 156(6):263–269
Salahudeen MS, Duffull SB, Nishtala PS (2015) Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr 25;15:31. https://doi.org/10.1186/s12877-015-0029-9
Welsh TJ, van der Wardt V, Ojo G, Gordon AL, Gladman JRF (2018) Anticholinergic drug burden tools/scales and adverse outcomes in different clinical settings: a systematic review of reviews. Drugs Aging 35(6):523–538. https://doi.org/10.1007/s40266-018-0549-z
Wouters H, Hilmer SN, Gnjidic D et al (2020) Long-term exposure to anticholinergic and sedative medications and cognitive and physical function in later life. J Gerontol A Biol Sci Med Sci 75(2):357–365. https://doi.org/10.1093/gerona/glz019
Martínez Arrechea S, Ferro Uriguen A, Beobide Telleria I, González Bueno J, Alaba Trueba J, Sevilla SD (2021) Prevalence of prescription of anticholinergic/sedative burden drugs among older people with dementia living in nursing homes. Rev Esp Geriatr Gerontol 56(1):11–17
Hsu HF, Chen KM, Belcastro F, Chen YF (2021) Polypharmacy and pattern of medication use in community-dwelling older adults: a systematic review. J Clin Nurs 30(7–8):918–928. https://doi.org/10.1111/jocn.15595
Bruin-Huisman L, Abu-Hanna A, van Weert HCPM, Beers E (2017) Potentially inappropriate prescribing to older patients in primary care in the Netherlands: a retrospective longitudinal study. Age Ageing 46(4):614–619. https://doi.org/10.1093/ageing/afw243
Cruz-Esteve I, Marsal-Mora JR, Galindo-Ortego G et al (2017) Análisis poblacional de la prescripción potencialmente inadecuada en ancianos según criterios STOPP/START (estudio STARTREC) [Potentially inappropriate prescribing in older Spanish population according to STOPP/START criteria (STARTREC study)]. Aten Primaria 49(3):166–176. https://doi.org/10.1016/j.aprim.2016.02.013
Ryan C, O’Mahony D, Kennedy J et al (2013) Potentially inappropriate prescribing in older residents in Irish nursing homes. Age Ageing 42(1):116–120. https://doi.org/10.1093/ageing/afs068
McMahon CG, Cahir CA, Kenny RA, Bennett K (2014) Inappropriate prescribing in older fallers presenting to an Irish emergency department. Age Ageing 43(1):44–50. https://doi.org/10.1093/ageing/aft114
Gallagher P, Lang PO, Cherubini A et al (2011) Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol 67(11):1175–1188. https://doi.org/10.1007/s00228-011-1061-0
Dalleur O, Spinewine A, Henrard S, Losseau C, Speybroeck N, Boland B (2012) Inappropriate prescribing and related hospital admissions in frail older persons according to the STOPP and START criteria. Drugs Aging 29(10):829–837. https://doi.org/10.1007/s40266-012-0016-1
San-José A, Agustí A, Vidal X et al (2014) Inappropriate prescribing to older patients admitted to hospital: a comparison of different tools of misprescribing and underprescribing. Eur J Intern Med 25(8):710–716. https://doi.org/10.1016/j.ejim.2014.07.011
San-José A, Agustí A, Vidal X et al (2015) Inappropriate prescribing to the oldest old patients admitted to hospital: prevalence, most frequently used medicines, and associated factors. BMC Geriatr 15:42. https://doi.org/10.1186/s12877-015-0038-8
Molist-Brunet N, Sevilla-Sánchez D, González-Bueno J et al (2021) Therapeutic optimization through goal-oriented prescription in nursing homes. Int J Clin Pharm 43(4):990–997. https://doi.org/10.1007/s11096-020-01206-x
Lu WH, Wen YW, Chen LK, Hsiao FY (2015) Effect of polypharmacy, potentially inappropriate medications and anticholinergic burden on clinical outcomes: a retrospective cohort study. CMAJ 187(4):E130–E137. https://doi.org/10.1503/cmaj.141219
Okudur SK, Dokuzlar O, Aydin AE, Kocyigit SE, Soysal P, Isik AT (2021) The evaluation of relationship between polypharmacy and anticholinergic burden scales. North Clin Istanb 11;8(2):139–144. https://doi.org/10.14744/nci.2020.17136. PMID: 33851077; PMCID: PMC8039107.
O'Mahony D (2020) STOPP/START criteria for potentially inappropriate medications/potential prescribing omissions in older people: origin and progress. Expert Rev Clin Pharmacol 13(1):15–22. https://doi.org/10.1080/17512433.2020.1697676. Epub 2019 Nov 30. PMID: 31790317.
Hilmer SN, Mager DE, Simonsick EM et al (2007) A drug burden index to define the functional burden of medications in older people. Arch Intern Med 167(8):781–787 (PubMed PMID: 17452540)
Morley JE, Malmstrom TK, Miller DK (2012) A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging 16(7):601–608. https://doi.org/10.1007/s12603-012-0084-2
Sainsbury A, Seebass G, Bansal A, Young JB (2005) Reliability of the Barthel Index when used with older people. Age Ageing 34(3):228–232. https://doi.org/10.1093/ageing/afi063
Graf C (2008) The Lawton instrumental activities of daily living scale. Am J Nurs 108(4):52–63. https://doi.org/10.1097/01.NAJ.0000314810.46029.74
Reisberg B, Ferris SH, de Leon MJ, Crook T (1988) Global deterioration scale (GDS). Psychopharmacol Bull 24(4):661–663
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Wilson MM, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A, Diebold MR, Morley JE (2005) Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr 82(5):1074–81 https://doi.org/10.1093/ajcn/82.5.1074. PMID: 16280441.
Park SH, Lee HS (2016) Assessing predictive validity of pressure ulcer risk scales-a systematic review and meta-analysis. Iran J Public Health 45(2):122–133
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23(10):433–441. https://doi.org/10.1111/j.1532-5415.1975.tb00927.x
Bellelli G, Morandi A, Davis DH, Mazzola P, Turco R, Gentile S, Ryan T, Cash H, Guerini F, Torpilliesi T, Del Santo F, Trabucchi M, Annoni G, MacLullich AM (2014) Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing 43(4):496–502. https://doi.org/10.1093/ageing/afu021. Epub 2014 Mar 2. Erratum in: Age Ageing. 2015 Jan;44(1):175. PMID: 24590568; PMCID: PMC4066613.
Alshammari H, Al-Saeed E, Ahmed Z, Aslanpour Z (2022) Prevalence and predictors of potentially inappropriate medications among patients aged ≥65 years on hospital admissions in Kuwait. Clin Interv Aging. 6;17:1025–1036. https://doi.org/10.2147/CIA.S328693. PMID: 35822127; PMCID: PMC9271279.
Meid AD, Quinzler R, Freigofas J, et al (2015) Medication underuse in aging outpatients with cardiovascular disease: prevalence, determinants, and outcomes in a prospective cohort study. PLoS One 10(8):e0136339. https://doi.org/10.1371/journal.pone.0136339
Gutiérrez-Valencia M, Izquierdo M, Lacalle-Fabo E et al (2018) Relationship between frailty, polypharmacy, and underprescription in older adults living in nursing homes. Eur J Clin Pharmacol 74(7):961–970. https://doi.org/10.1007/s00228-018-2452-2
de Groote P, Isnard R, Assyag P, Clerson P, Ducardonnet A, Galinier M, Jondeau G, Leurs I, Thébaut, J.-.-F. and Komajda, M. (2007) Is the gap between guidelines and clinical practice in heart failure treatment being filled? Insights from the IMPACT RECO survey. Eur J Heart Fail 9:1205–1211. https://doi.org/10.1016/j.ejheart.2007.09.008
Manias E, Maier A, Krishnamurthy G (2019) Inappropriate medication use in hospitalised oldest old patients across transitions of care. Aging Clin Exp Res 31(11):1661–1673. https://doi.org/10.1007/s40520-018-01114-1
Wong HL, Weaver C, Marsh L, Mon KO, Dapito JM, Amin FR et al (2023) Polypharmacy and cumulative anticholinergic burden in older adults hospitalized with fall. Aging Medicine
Sevilla-Sánchez D, Molist-Brunet N, González-Bueno J, Solà-Bonada N, Espaulella-Panicot J, Codina-Jané C (2018) Prevalence, risk factors and adverse outcomes of anticholinergic burden in patients with advanced chronic conditions at hospital admission. Geriatr Gerontol Int 18(8):1159–1165
Mortsiefer A, Löscher S, Pashutina Y et al (2023) Family conferences to facilitate deprescribing in older outpatients with frailty and with polypharmacy: the COFRAIL cluster randomized trial. JAMA Netw Open 6(3):e234723. https://doi.org/10.1001/jamanetworkopen.2023.4723
Blum M R, Sallevelt B T G M, Spinewine A, O’Mahony D, Moutzouri E, Feller M et al (2021) Optimizing therapy to prevent avoidable hospital admissions in multimorbid older adults (OPERAM): cluster randomised controlled trial BMJ 374 :n1585. https://doi.org/10.1136/bmj.n1585
Pazan F, Petrovic M, Cherubini A et al (2021) Current evidence on the impact of medication optimization or pharmacological interventions on frailty or aspects of frailty: a systematic review of randomized controlled trials [published correction appears in Eur J Clin Pharmacol. Oct;77(10):1593–1594. Eur J Clin Pharmacol 77(1):1–12. https://doi.org/10.1007/s00228-020-02951-8
- Ibrahim K, Cox NJ, Stevenson JM, Lim S, Fraser SDS, Roberts HC (2021) A systematic review of the evidence for deprescribing interventions among older people living with frailty. BMC Geriatr 21(1):258. Published. https://doi.org/10.1186/s12877-021-02208-8
Mucalo I, Hadžiabdić MO, Brajković A et al (2017) Potentially inappropriate medicines in elderly hospitalised patients according to the EU(7)-PIM list, STOPP version 2 criteria and comprehensive protocol. Eur J Clin Pharmacol 73(8):991–999. https://doi.org/10.1007/s00228-017-2246-y
Grischott T, Rachamin Y, Senn O, Hug P, Rosemann T, Neuner-Jehle S (2023) Medication review and enhanced information transfer at discharge of older patients with polypharmacy: a cluster-randomized controlled trial in swiss hospitals. J Gen Intern Med 38(3):610–618. https://doi.org/10.1007/s11606-022-07728-6
Vasilevskis EE, Shah AS, Hollingsworth EK et al (2023) Deprescribing medications among older adults from end of hospitalization through postacute care: a Shed-MEDS randomized clinical trial. JAMA Intern Med 183(3):223–231. https://doi.org/10.1001/jamainternmed.2022.6545
Lunghi C, Trevisan C, Fusaroli M et al (2022) Strategies and tools for supporting the appropriateness of drug use in older people. Pharmaceuticals (Basel) 15(8):977. https://doi.org/10.3390/ph15080977
Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B (2020) Adverse outcomes of polypharmacy in older people: systematic review of reviews. Vol. 21, JAMDA Elsevier Inc p. 181–7.
Author information
Authors and Affiliations
Contributions
M.Z. wrote the entire manuscript and all the authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
This is a prospective observational study that has the approval of the Ethics Committee of Vall d’Hebron Hospital and adheres to the Declaration of Helsinki (1964) and its later amendments (current version dating from 2013).
Consent to participate
All patients provided informed consent to participate in this study.
Consent for publication
All patients provided informed consent that their patient-related data may be used for publications.
Competing interests
All authors declare that they have no financial conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zuleta, M., San-José, A., Gozalo, I. et al. Patterns of inappropriate prescribing and clinical characteristics in patients at admission to an acute care of the elderly unit. Eur J Clin Pharmacol 80, 553–561 (2024). https://doi.org/10.1007/s00228-024-03627-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-024-03627-3