Abstract
Background
Gastrointestinal endoscopic procedures (GEPs) are frequently employed for the diagnosis and treatment of various gastrointestinal ailments. While propofol sedation is widely used during these procedures, there is a concern regarding its potential negative effects. Intravenous (IV) lidocaine has been suggested as an add-on to propofol sedation for GEPs, but current evidence on its efficiency and safety is limited. This systematic review and meta-analysis aimed to assess the impact of IV lidocaine on outcomes in patients receiving propofol during GEPs.
Methods
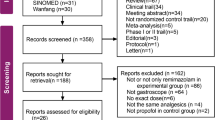
Electronic databases were screened for randomized controlled trials (RCTs), published up to 31 March 2023, investigating the effectiveness of intravenous lidocaine addition to propofol sedation during GEPs.
Results
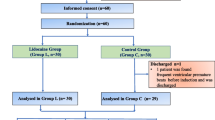
A total of 12 RCTs involving 712 patients that received IV lidocaine and propofol for GEF and 719 patients that received propofol were analyzed. Adding IV lidocaine to propofol sedation led to significant reduction in pain after the procedure (standardized mean difference (SMD) = − 0.91, 95% confidence interval [CI]; − 1.51 to − 0.32), decreased propofol usage (SMD = − 0.89; 95% CI, − 1.31 to − 0.48), lower recovery time (SMD = − 0.95 min; 95% CI, − 1.48 to − 0.43), and decreased pain score (SMD = − 0.91; 95% CI, − 1.51 to − 0.32). The overall rate of adverse events was markedly less in the lidocaine group than in the control group (RR = 0.74; 95% CI, 0.56 to 0.99).
Conclusion
Our results show that IV lidocaine improves patient outcomes by reducing post-procedural pain, decreasing propofol usage, shortening recovery time, and lowering pain scores. This study provides compelling evidence supporting the use of intravenous lidocaine as an adjunct to propofol sedation for gastrointestinal endoscopic procedures. However, further research is necessary to optimize the use of lidocaine and fully understand its long-term effects.






Similar content being viewed by others
Data availability
All data related to the manuscript are available as online supplementary material. Researchers interested in accessing and utilizing the data can find it in the supplementary files accompanying this article.
References
ASGE Standards of Practice Committee, Early DS, Lightdale JR et al (2018) Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc 87:327–337. https://doi.org/10.1016/j.gie.2017.07.018
Cohen LB, Hightower CD, Wood DA et al (2004) Moderate level sedation during endoscopy: a prospective study using low-dose propofol, meperidine/fentanyl, and midazolam. Gastrointest Endosc 59:795–803. https://doi.org/10.1016/s0016-5107(04)00349-9
Pao Y-Y, Chung K-C, Chen J-P et al (2014) The hemodynamic effect of an intravenous antispasmodic on propofol requirements during colonoscopy: a randomized clinical trial. Acta Anaesthesiol Taiwan 52:13–16. https://doi.org/10.1016/j.aat.2014.05.003
Dossa F, Medeiros B, Keng C et al (2020) Propofol versus midazolam with or without short-acting opioids for sedation in colonoscopy: a systematic review and meta-analysis of safety, satisfaction, and efficiency outcomes. Gastrointest Endosc 91:1015–1026.e7. https://doi.org/10.1016/j.gie.2019.12.047
Khoi C-S, Wong J-J, Wang H-C et al (2015) Age correlates with hypotension during propofol-based anesthesia for endoscopic retrograde cholangiopancreatography. Acta Anaesthesiol Taiwan 53:131–134. https://doi.org/10.1016/j.aat.2015.10.002
Luginbühl M, Vuilleumier P, Schumacher P, Stüber F (2009) Anesthesia or sedation for gastroenterologic endoscopies. Curr Opin Anaesthesiol 22:524–531. https://doi.org/10.1097/ACO.0b013e32832dbb7c
Zhang R, Lu Q, Wu Y (2018) The comparison of midazolam and propofol in gastrointestinal endoscopy: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech 28:153–158. https://doi.org/10.1097/SLE.0000000000000532
Barends CRM, Driesens MK, van Amsterdam K et al (2020) Moderate-to-deep sedation using target-controlled infusions of propofol and remifentanil: adverse events and risk factors: a retrospective cohort study of 2937 procedures. Anesth Analg 131:1173–1183. https://doi.org/10.1213/ANE.0000000000004593
Wang F, Shen S-R, Xiao D-H et al (2011) Sedation, analgesia, and cardiorespiratory function in colonoscopy using midazolam combined with fentanyl or propofol. Int J Colorectal Dis 26:703–708. https://doi.org/10.1007/s00384-011-1162-3
Watkins TJ, Bonds RL, Hodges K et al (2014) Evaluation of postprocedure cognitive function using 3 distinct standard sedation regimens for endoscopic procedures. AANA J 82:133–139
Thompson R, Seck V, Riordan S, Wong S (2019) Comparison of the effects of midazolam/fentanyl, midazolam/propofol, and midazolam/fentanyl/propofol on cognitive function after gastrointestinal endoscopy. Surg Laparosc Endosc Percutan Tech 29:441–446. https://doi.org/10.1097/SLE.0000000000000679
Hsu Y-H, Lin F-S, Yang C-C et al (2015) Evident cognitive impairments in seemingly recovered patients after midazolam-based light sedation during diagnostic endoscopy. J Formos Med Assoc 114:489–497. https://doi.org/10.1016/j.jfma.2013.07.018
Altermatt FR, Bugedo DA, Delfino AE et al (2012) Evaluation of the effect of intravenous lidocaine on propofol requirements during total intravenous anaesthesia as measured by bispectral index. Br J Anaesth 108:979–983. https://doi.org/10.1093/bja/aes097
Weibel S, Jokinen J, Pace NL et al (2016) Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth 116:770–783. https://doi.org/10.1093/bja/aew101
Hung K-C, Yew M, Lin Y-T et al (2022) Impact of intravenous and topical lidocaine on clinical outcomes in patients receiving propofol for gastrointestinal endoscopic procedures: a meta-analysis of randomised controlled trials. Br J Anaesth 128:644–654. https://doi.org/10.1016/j.bja.2021.08.036
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Brozek JL, Akl EA, Alonso-Coello P et al (2009) Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy 64:669–677. https://doi.org/10.1111/j.1398-9995.2009.01973.x
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Forster C, Vanhaudenhuyse A, Gast P et al (2018) Intravenous infusion of lidocaine significantly reduces propofol dose for colonoscopy: a randomised placebo-controlled study. Br J Anaesth 121:1059–1064. https://doi.org/10.1016/j.bja.2018.06.019
Ates I, Aydin ME, Albayrak B et al (2021) Pre-procedure intravenous lidocaine administration on propofol usage for endoscopic retrograde cholangiopancreatography: a prospective, randomized, double-blind study. J Gastroenterol Hepatol 36:1286–1290. https://doi.org/10.1111/jgh.15356
Kim JE, Choi JB, Koo B-N et al (2016) Efficacy of intravenous lidocaine during endoscopic submucosal dissection for gastric neoplasm: a randomized, double-blind, controlled study. Medicine (Baltimore) 95:e3593. https://doi.org/10.1097/MD.0000000000003593
Sun X, Xu Y, Zhang X et al (2018) Topical pharyngeal anesthesia provides no additional benefit to propofol sedation for esophagogastroduodenoscopy: a randomized controlled double-blinded clinical trial. Sci Rep 8:6682. https://doi.org/10.1038/s41598-018-25164-7
Liu H, Chen M, Lian C et al (2021) Effect of intravenous administration of lidocaine on the ED50 of propofol induction dose during gastroscopy in adult patients: a randomized, controlled study. J Clin Pharm Ther 46:711–716. https://doi.org/10.1111/jcpt.13335
Liu J, Liu X, Peng L-P et al (2020) Efficacy and safety of intravenous lidocaine in propofol-based sedation for ERCP procedures: a prospective, randomized, double-blinded, controlled trial. Gastrointest Endosc 92:293–300. https://doi.org/10.1016/j.gie.2020.02.050
Nongnuang K, Limprasert N, Munjupong S (2022) Can intravenous lidocaine definitely attenuate propofol requirement and improve outcomes among colonoscopic patients under intravenous sedation?: A double-blinded, randomized controlled trial. Medicine (Baltimore) 101:e30670. https://doi.org/10.1097/MD.0000000000030670
Arun N, Hussain M, Kumari P, Kumar A (2022) Evaluation of propofol-sparing effect of intravenous lignocaine in patients undergoing daycare upper gastrointestinal endoscopic procedures. Cureus 14:e32090. https://doi.org/10.7759/cureus.32090
Qi X-R, Sun J-Y, An L-X, Zhang K (2022) Effect of intravenous lidocaine on the ED50 of propofol for inserting gastroscope without body movement in adult patients: a randomized, controlled study. BMC Anesthesiol 22:319. https://doi.org/10.1186/s12871-022-01861-9
Li X, Lv X, Jiang Z et al (2020) Application of intravenous lidocaine in obese patients undergoing painless colonoscopy: a prospective, randomized, double-blind, controlled study. Drug Des Devel Ther 14:3509–3518. https://doi.org/10.2147/DDDT.S266062
Hu S, Wang M, Li S et al (2022) Intravenous lidocaine significantly reduces the propofol dose in elderly patients undergoing gastroscopy: a randomized controlled trial. Drug Des Devel Ther 16:2695–2705. https://doi.org/10.2147/DDDT.S377237
Chen M, Lu Y, Liu H et al (2020) The propofol-sparing effect of intravenous lidocaine in elderly patients undergoing colonoscopy: a randomized, double-blinded, controlled study. BMC Anesthesiol 20:132. https://doi.org/10.1186/s12871-020-01049-z
Balshem H, Helfand M, Schünemann HJ et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015
Martindale SJ (2006) Anaesthetic considerations during endoscopic retrograde cholangiopancreatography. Anaesth Intensive Care 34:475–480. https://doi.org/10.1177/0310057X0603400401
Liu Q, Li L, Wei J, Xie Y (2023) Correlation and influencing factors of preoperative anxiety, postoperative pain, and delirium in elderly patients undergoing gastrointestinal cancer surgery. BMC Anesthesiol 23:78. https://doi.org/10.1186/s12871-023-02036-w
Hans GA, Lauwick SM, Kaba A et al (2010) Intravenous lidocaine infusion reduces bispectral index-guided requirements of propofol only during surgical stimulation. Br J Anaesth 105:471–479. https://doi.org/10.1093/bja/aeq189
Gustafsson UO, Scott MJ, Schwenk W et al (2012) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr 31:783–800. https://doi.org/10.1016/j.clnu.2012.08.013
Feldheiser A, Aziz O, Baldini G et al (2016) Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 2: consensus statement for anaesthesia practice. Acta Anaesthesiol Scand 60:289–334. https://doi.org/10.1111/aas.12651
Xiang Y, Chen C, Chen H et al (2014) The effect of epidural lidocaine administration on sedation of propofol general anesthesia: a randomized trial. J Clin Anesth 26:523–529. https://doi.org/10.1016/j.jclinane.2014.03.016
Chanques G, Constantin J-M, Devlin JW et al (2020) Analgesia and sedation in patients with ARDS. Intensive Care Med 46:2342–2356. https://doi.org/10.1007/s00134-020-06307-9
Euasobhon P, Dej-Arkom S, Siriussawakul A et al (2016) Lidocaine for reducing propofol-induced pain on induction of anaesthesia in adults. Cochrane Database Syst Rev 2:CD007874. https://doi.org/10.1002/14651858.CD007874.pub2
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
FW, LZ, WX, and JB wrote the manuscript and made the figures. FW and JB conducted the literature search, study selection, and analysis. FW, LZ, and JB approved the final revisions of the manuscript submitted for publication. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
None.
Consent for publication
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, F., Zhan, L., Xu, W. et al. Effect of intravenous lidocaine on outcomes in patients receiving propofol for gastrointestinal endoscopic procedures: an updated systematic review and meta-analysis. Eur J Clin Pharmacol 80, 39–52 (2024). https://doi.org/10.1007/s00228-023-03589-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03589-y