Abstract
Background
To investigate the effect of timing of statin administration on lipid-lowering efficacy.
Methods
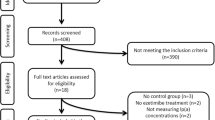
Computer searches of Pubmed, Embase, Cochrane Library, and Web of Science databases from 1986 to 2023. The impact of administration time on the lipid-lowering efficacy of statin drugs was investigated. Following a series of screenings, a funnel plot was constructed to assess its symmetry, and Egger and Beggar tests were conducted using StataMP-64 to evaluate publication bias. Meta-analysis was performed using RevMan 5.3 to combine MD values.
Results
Fifteen papers (1352 participants) met and included the criteria. The results of the meta-analysis showed that the effect of morning and evening administration time on plasma triglycerides (TG) (P > 0.05) and plasma high-density lipoprotein cholesterol (HDL-C) (P > 0.05) was not statistically significant. There were significant reductions in total cholesterol (TC) (MD: 0.15 mmol/L, 95% CI: 0.06–0.23, P < 0.01) and low-density lipoprotein cholesterol (LDL-C) (MD: 0.10 mmol/L, 95% CI: − 0.00–0.20, P < 0.01) in the night group. According to the analysis results of the half-life of statins, only short half-life statins showed that nocturnal administration reduced LDL-C (MD: 0.21 mmol/L, 95% CI: 0.09–0.33, P < 0.01) and TC (MD: 0.32 mmol/L, 95% CI: 0.18–0.46, P < 0.01) levels and was better than morning administration. Long half-life statins did not show significant differences. In addition, the administration time of short half-life statins also showed that night administration tended to reduce TG (MD: 0.16 mmol/L, 95% CI: 0.02–0.30, P < 0.05) levels. In subgroup analysis according to clinical factors in patients aged < 55 years, there was no significant difference in the timing of administration between the two groups; the efficacy of statins in lowering lipids in patients aged ≥ 55 years was significantly different in the TC group (P < 0.01) and LDL-C group (P < 0.01). The administration time of the TC group (P < 0.05) and LDL-C group (P < 0.05) in the Americas, Europe, and Asian groups was significantly different for statins. In addition, the American group also showed that the administration time of the two groups was significantly different from the TG group (P < 0.05).
Conclusion
The efficacy of administering short half-life statin drugs at night in reducing plasma levels of TC, LDL-C, and TG surpasses that of morning administration. However, this study did not determine the impact of timing of statin administration in patients taking long half-life statins on the efficacy of the medication. Therefore, it is recommended to consider patient adherence when. The study was registered on PROSPERO (International Prospective Register of Systematic Reviews) as CRD42022372105 (available at https://www.crd.york.ac.uk/prospero/).






Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- TG:
-
Triglycerides
- HDL-C:
-
High-density lipoprotein cholesterol
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- MD:
-
Mean difference
- SE:
-
Standard error
- SD:
-
Standard deviation
- CI:
-
Confidence interval
- I2 :
-
Statistic of inconsistency
- RCTs:
-
Randomized controlled trials
- HMG-CoA reductase inhibitors:
-
3-Hydroxy-3-methyl glutaryl coenzyme A reductase inhibitor
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- NOS:
-
Newcastle-Ottawa Scale
References
Gu JK, Charles LE, Fekedulegn D, Allison P, Ma CC, Violanti JM, Andrew ME (2021) Temporal trends in prevalence of cardiovascular disease (CVD) and CVD risk factors among U.S. older workers: NHIS 2004–2018. Ann Epidemiol 55:78–82. https://doi.org/10.1016/j.annepidem.2020.10.002
Escudero-Sánchez G, Rico-Martín S, Sánchez-Bacaicoa C, Costo C, Galán-González J, Calderón-García JF, Pedrera-Zamorano JD, Sánchez Muñoz-Torrero JF (2023) Optimal control of all modifiable vascular risk factors among patients with atherosclerotic disease. A real-life study. Curr Probl Cardiol 48:101530. https://doi.org/10.1016/j.cpcardiol.2022.101530
Ye Z, Lu H, Su Q, Guo W, Dai W, Li H, Yang H, Li L (2017) Effect of high-dose rosuvastatin loading before percutaneous coronary intervention in Chinese patients with acute coronary syndrome: a systematic review and meta-analysis. PLoS One 12:e0171682. https://doi.org/10.1371/journal.pone.0171682
Fonseca FAH, Izar MC, Maugeri IML, Berwanger O, Damiani LP, Pinto IM, Szarf G, França CN, Bianco HT, Moreira FT, Caixeta A, Alves CMR, Soriano Lopes A, Klassen A, Tavares MFM, Fonseca HA, Carvalho ACC (2017) Effects of four antiplatelet/statin combined strategies on immune and inflammatory responses in patients with acute myocardial infarction undergoing pharmacoinvasive strategy: design and rationale of the B and T Types of Lymphocytes Evaluation in Acute Myocardial Infarction (BATTLE-AMI) study: study protocol for a randomized controlled trial. Trials 18:601. https://doi.org/10.1186/s13063-017-2361-1
Schroor MM, Sennels HP, Fahrenkrug J, Jørgensen HL, Plat J, Mensink RP (2019) Diurnal variation of markers for cholesterol synthesis, cholesterol absorption, and bile acid synthesis: a systematic review and the Bispebjerg study of diurnal variations. nutrients 11. https://doi.org/10.3390/nu11071439
Laufs U, Weingärtner O, Kassner U, Schatz U (2022) [State of the art: statin therapy]. Dtsch Med Wochenschr 147:62–68. https://doi.org/10.1055/a-1516-2471
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, Koffel JB (2021) PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev 10:39. https://doi.org/10.1186/s13643-020-01542-z
Illingworth DR (1986) Comparative efficacy of once versus twice daily mevinolin in the therapy of familial hypercholesterolemia. Clin Pharmacol Ther 40:338–43. https://doi.org/10.1038/clpt.1986.185
Hunninghake DB, Mellies MJ, Goldberg AC, Kuo PT, Kostis JB, Schrott HG, Insull W, Jr., Pan HY (1990) Efficacy and safety of pravastatin in patients with primary hypercholesterolemia. II. Once-daily versus twice-daily dosing. Atherosclerosis 85:219–27. https://doi.org/10.1016/0021-9150(90)90114-x
Martin PD, Mitchell PD, Schneck DW (2002) Pharmacodynamic effects and pharmacokinetics of a new HMG-CoA reductase inhibitor, rosuvastatin, after morning or evening administration in healthy volunteers. Br J Clin Pharmacol 54:472–7. https://doi.org/10.1046/j.1365-2125.2002.01688.x
Plakogiannis R, Cohen H, Taft D (2005) Effects of morning versus evening administration of atorvastatin in patients with hyperlipidemia. Am J Health Syst Pharm 62:2491–4. https://doi.org/10.2146/ajhp050072
Lafeber M, Grobbee DE, Schrover IM, Thom S, Webster R, Rodgers A, Visseren FL, Bots ML, Spiering W (2015) Comparison of a morning polypill, evening polypill and individual pills on LDL-cholesterol, ambulatory blood pressure and adherence in high-risk patients; a randomized crossover trial. Int J Cardiol 181:193–9. https://doi.org/10.1016/j.ijcard.2014.11.176
Wallace A, Chinn D, Rubin G (2003) Taking simvastatin in the morning compared with in the evening: randomised controlled trial. Bmj 327:788. https://doi.org/10.1136/bmj.327.7418.788
Scharnagl H, Vogel M, Abletshauser C, Freisinger F, Stojakovic T, März W (2006) Efficacy and safety of fluvastatin-extended release in hypercholesterolemic patients: morning administration is equivalent to evening administration. Cardiology 106:241–8. https://doi.org/10.1159/000093200
Kruse W, Nikolaus T, Rampmaier J, Weber E, Schlierf G (1993) Actual versus prescribed timing of lovastatin doses assessed by electronic compliance monitoring. Eur J Clin Pharmacol 45:211–5. https://doi.org/10.1007/bf00315385
Lund TM, Torsvik H, Falch D, Christophersen B, Skårdal R, Gullestad L (2002) Effect of morning versus evening intake of simvastatin on the serum cholesterol level in patients with coronary artery disease. Am J Cardiol 90:784–6. https://doi.org/10.1016/s0002-9149(02)02614-0
Yoon HS, Kim SH, Kim JK, Ko SH, Ko JE, Park SJ, Park MG, Lee JH, Hyon MS (2011) Comparison of effects of morning versus evening administration of ezetimibe/simvastatin on serum cholesterol in patients with primary hypercholesterolemia. Ann Pharmacother 45:841–9. https://doi.org/10.1345/aph.1P511
Yi YJ, Kim HJ, Jo SK, Kim SG, Song YR, Chung W, Han KH, Lee CH, Hwang YH, Oh KH (2014) Comparison of the efficacy and safety profile of morning administration of controlled-release simvastatin versus evening administration of immediate-release simvastatin in chronic kidney disease patients with dyslipidemia. Clin Ther 36:1182–90. https://doi.org/10.1016/j.clinthera.2014.06.005
Kim SH, Kim MK, Seo HS, Hyun MS, Han KR, Cho SW, Kim YK, Hoon Park S (2013) Efficacy and safety of morning versus evening dose of controlled-release simvastatin tablets in patients with hyperlipidemia: a randomized, double-blind, multicenter phase III trial. Clin Ther 35:1350–60.e1. https://doi.org/10.1016/j.clinthera.2013.06.020
Saito Y, Yoshida S, Nakaya N, Hata Y, Goto Y (1991) Comparison between morning and evening doses of simvastatin in hyperlipidemic subjects. A double-blind comparative study. Arterioscler Thromb 11:816–26. https://doi.org/10.1161/01.atv.11.4.816
Ozaydin M, Dede O, Dogan A, Aslan SM, Altinbas A, Ozturk M, Varol E, Turker Y (2006) Effects of morning versus evening intake of atorvastatin on major cardiac event and restenosis rates in patients undergoing first elective percutaneous coronary intervention. Am J Cardiol 97:44–7. https://doi.org/10.1016/j.amjcard.2005.07.107
Heng WK, Ng YP, Ooi GS, Habshoh J, Nurazlin J, Nor Azah MN, Hasniza H, Noriza W (2019) Comparison of the efficacy and level of adherence for morning versus evening versus before bedtime administration of simvastatin in hypercholesterolemic patients. Med J Malaysia 74:477–482
Grant LK, St Hilaire MA, Brainard GC, Czeisler CA, Lockley SW, Rahman SA (2021) Endogenous circadian regulation and phase resetting of clinical metabolic biomarkers. J Pineal Res 71:e12752. https://doi.org/10.1111/jpi.12752
Toledo-Corral CM, Ding L, Morales JC, Chapman TM, Romero MB, Weigensberg MJ (2023) Morning serum cortisol is uniquely associated with cardiometabolic risk independent of body composition in Latino adolescents. Metab Syndr Relat Disord 21:214–221. https://doi.org/10.1089/met.2022.0091
Awad K, Banach M (2018) The optimal time of day for statin administration: a review of current evidence. Curr Opin Lipidol 29:340–345. https://doi.org/10.1097/mol.0000000000000524
Xie Z, Zhang J, Wang C, Yan X (2021) Chronotherapy for morning blood pressure surge in hypertensive patients: a systematic review and meta-analysis. BMC Cardiovasc Disord 21:274. https://doi.org/10.1186/s12872-021-02081-8
Dai J, Hou J, Xing L, Jia H, Hu S, Soeda T, Minami Y, Ong D, Vergallo R, Zhang S, Lee H, Yu B, Jang IK (2017) Is age an important factor for vascular response to statin therapy? A serial optical coherence tomography and intravascular ultrasound study. Coron Artery Dis 28:209–217. https://doi.org/10.1097/mca.0000000000000465
Robinson JG, Booth B (2010) Statin use and lipid levels in older adults: National Health and Nutrition Examination Survey, 2001 to 2006. J Clin Lipidol 4:483–90. https://doi.org/10.1016/j.jacl.2010.10.002
Fallahzadeh MK, Ku E, Chu CD, McCulloch CE, Tuot DS (2022) Racial differences in medication utilization for secondary prevention of cardiovascular disease in kidney transplant recipients: a post hoc analysis of the FAVORIT trial cohort. Kidney Med 4:100438. https://doi.org/10.1016/j.xkme.2022.100438
Zanchin C, Koskinas KC, Ueki Y, Losdat S, Häner JD, Bär S, Otsuka T, Inderkum A, Jensen MRJ, Lonborg J, Fahrni G, Ondracek AS, Daemen J, van Geuns RJ, Iglesias JF, Matter CM, Spirk D, Juni P, Mach F, Heg D, Engstrom T, Lang I, Windecker S, Räber L (2021) Effects of the PCSK9 antibody alirocumab on coronary atherosclerosis in patients with acute myocardial infarction: a serial, multivessel, intravascular ultrasound, near-infrared spectroscopy and optical coherence tomography imaging study-rationale and design of the PACMAN-AMI trial. Am Heart J 238:33–44. https://doi.org/10.1016/j.ahj.2021.04.006
Kofink D, Eppinga RN, van Gilst WH, Bakker SJL, Dullaart RPF, van der Harst P, Asselbergs FW (2017) Statin effects on metabolic profiles: data from the PREVEND IT (Prevention of Renal and Vascular End-stage Disease Intervention Trial). Circ Cardiovasc Genet 10. https://doi.org/10.1161/circgenetics.117.001759
Amarenco P, Kim JS, Labreuche J, Charles H, Giroud M, Lee BC, Mahagne MH, Nighoghossian N, Gabriel Steg P, Vicaut É, Bruckert E (2020) Benefit of targeting a LDL (low-density lipoprotein) cholesterol <70 mg/dL during 5 years after ischemic stroke. Stroke 51:1231–1239. https://doi.org/10.1161/strokeaha.119.028718
Peterson GG, Pu J, Magid DJ, Barterian L, Kranker K, Barna M, Conwell L, Rose A, Blue L, Markovitz A, McCall N, Markovich P (2021) Effect of the million hearts cardiovascular disease risk reduction model on initiating and intensifying medications: a prespecified secondary analysis of a randomized clinical trial. JAMA Cardiol 6:1050–1059. https://doi.org/10.1001/jamacardio.2021.1565
Funding
This work was supported by National Natural Science Foundation of China (81370316).
Author information
Authors and Affiliations
Contributions
Chang Wang is responsible for literature screening, study design, and manuscript writing; Yawen Quan and Linfeng Wang are responsible for data collection and participant management; Gang Li is responsible for providing ideas and manuscript proofreading. All authors reviewed the manuscript and had no different opinions.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, C., Quan, Y., Wang, L. et al. Effect of timing of administration on lipid-lowering efficacy of statins-meta-analysis. Eur J Clin Pharmacol 79, 1641–1656 (2023). https://doi.org/10.1007/s00228-023-03575-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03575-4