Abstract
Background
Triple antithrombotic therapy (TAT), a combination of an oral anticoagulant and dual antiplatelet therapy (DAPT), is a key treatment for prevention of ischemic events in patients with atrial fibrillation (AF) undergoing percutaneous coronary intervention (PCI). However, TAT is not extensively used because of the risk of bleeding. This study aimed to determine the utilization and influencing factors of TAT using real-world data in the non-vitamin K antagonist oral anticoagulants (NOACs) era.
Methods
We analyzed National Inpatient Sample data compiled by the Health Insurance Review & Assessment Service (HIRA-NIS) from 2011 to 2020. Patients with AF who underwent PCI with stent implantation and with an increased stroke risk were selected as candidates for TAT therapy. Demographic and clinical factors associated with TAT use were investigated using the chi-squared test and the Student t-test, and influencing factors were identified using multiple logistic regression.
Results
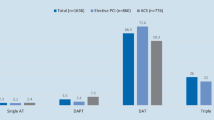
The TAT utilization rate steadily increased from 30.3% in 2011 to 65.4% in 2020 (Cochran-Armitage trend test: p < 0.001) with an average of 45.9%. Positive influencing factors for TAT use were identified as congestive heart failure, history of previous stroke/transient ischemic attack/thromboembolism, valvular heart disease, and year. Negative influencing factors included insurance type (medical aid or Patriots & Veterans Insurance), type of medical institution (general hospitals or primary medical institutions), and comorbidities such as renal disease, liver disease, and history of the previous hemorrhage.
Conclusions
The utilization of TAT following PCI among high-stroke risk AF patients steadily increased from 2011 to 2020, reaching 65.4% by the end of the study period. However, in 2020, a significant proportion of 29.4% of patients still received DAPT, indicating that many AF patients undergoing PCI did not receive adequate antithrombotic therapy.


Similar content being viewed by others
Data availability
The authors used the HIRA-NIS data for this study and do not have permission to share these data. Raw data can be accessed with permission from Health Insurance Review and Assessment Service in Korea (http://opendata.hira.or.kr).
References
Lippi G, Sanchis-Gomar F, Cervellin G (2021) Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. Int J Stroke 16(2):217–221
Kornej J, Börschel CS, Benjamin EJ, Schnabel RB (2020) Epidemiology of atrial fibrillation in the 21st century: novel methods and new insights. Circ Res 127(1):4–20
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan G-A, Dilaveris PE (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS) The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 42(5):373–498
Angiolillo DJ, Bhatt DL, Cannon CP, Eikelboom JW, Gibson CM, Goodman SG, Granger CB, Holmes DR, Lopes RD, Mehran R, Moliterno DJ, Price MJ, Saw J, Tanguay JF, Faxon DP (2021) Antithrombotic therapy in patients with atrial fibrillation treated with oral anticoagulation undergoing percutaneous coronary intervention: a North American perspective: 2021 update. Circulation 143(6):583–596. https://doi.org/10.1161/circulationaha.120.050438
El-Shetry M, Mahfouz R, Frere A-F, Abdeldayem M (2021) The interplay between atrial fibrillation and acute myocardial infarction. Br J Hosp Med 82(2):1–9
Michniewicz E, Mlodawska E, Lopatowska P, Tomaszuk-Kazberuk A, Malyszko J (2018) Patients with atrial fibrillation and coronary artery disease–double trouble. Adv Med Sci 63(1):30–35
Lee HY, Yang P-S, Kim T-H, Uhm J-S, Pak H-N, Lee M-H, Joung B (2017) Atrial fibrillation and the risk of myocardial infarction: a nation-wide propensity-matched study. Sci Rep 7(1):1–8
Soliman EZ, Lopez F, O’Neal WT, Chen LY, Bengtson L, Zhang Z-M, Loehr L, Cushman M, Alonso A (2015) Atrial fibrillation and risk of ST-segment–elevation versus non–ST-segment–elevation myocardial infarction: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 131(21):1843–1850
Soliman EZ, Safford MM, Muntner P, Khodneva Y, Dawood FZ, Zakai NA, Thacker EL, Judd S, Howard VJ, Howard G (2014) Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med 174(1):107–114
Chao T-F, Huang Y-C, Liu C-J, Chen S-J, Wang K-L, Lin Y-J, Chang S-L, Lo L-W, Hu Y-F, Tuan T-C (2014) Acute myocardial infarction in patients with atrial fibrillation with a CHA2DS2-VASc score of 0 or 1: a nationwide cohort study. Heart Rhythm 11(11):1941–1947
Kralev S, Schneider K, Lang S, Suselbeck T, Borggrefe M (2011) Incidence and severity of coronary artery disease in patients with atrial fibrillation undergoing first-time coronary angiography. PLoS ONE 6(9):e24964. https://doi.org/10.1371/journal.pone.0024964
Lip GY, Banerjee A, Boriani G, en Chiang C, Fargo R, Freedman B, Lane DA, Ruff CT, Turakhia M, Werring D, (2018) Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest 154(5):1121–1201
Collet J-P, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, Gale CP, Gilard M, Jobs A, Jüni P, Lambrinou E, Lewis BS, Mehilli J, Meliga E, Merkely B, Mueller C, Roffi M, Rutten FH, Sibbing D, Siontis GCM, Chettibi M, Hayrapetyan HG, Metzler B, Najafov R, Stelmashok VI, Claeys M, Kušljugić Z, Gatzov PM, Skoric B, Panayi G, Mates M, Sorensen R, Shokry K, Marandi T, Kajander OA, Commeau P, Aladashvili A, Massberg S, Nikas D, Becker D, Guðmundsdóttir IJ, Peace AJ, Beigel R, Indolfi C, Aidargaliyeva N, Elezi S, Beishenkulov M, Maca A, Gustiene O, Degrell P, Cassar Maempel A, Ivanov V, Damman P, Kedev S, Steigen TK, Legutko J, Morais J, Vinereanu D, Duplyakov D, Zavatta M, Pavlović M, Orban M, Bunc M, Ibañez B, Hofmann R, Gaemperli O, Marjeh YB, Addad F, Tutar E, Parkhomenko A, Karia N, Group ESD (2020) 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 42(14):1289–1367. https://doi.org/10.1093/eurheartj/ehaa575
Wolf PA, Abbott RD, Kannel WB (1991) Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 22(8):983–988
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, Ellinor PT, Ezekowitz MD, Field ME, Furie KL (2019) 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 74(1):104–132
Park J, Choi EK, Han KD, Choi YJ, Lee E, Choe W, Lee SR, Cha MJ, Lim WH, Kang J, Park KW, Oh S, Lip GYH (2019) Temporal trends in prevalence and antithrombotic treatment among Asians with atrial fibrillation undergoing percutaneous coronary intervention: a nationwide Korean population-based study. PLoS ONE 14(1):e0209593. https://doi.org/10.1371/journal.pone.0209593
Boivin-Proulx LA, Deneault-Marchand A, Matteau A, Mansour S, Gobeil F, Camm JA, Fox KAA, Potter BJ (2020) Time-trends and treatment gaps in the antithrombotic management of patients with atrial fibrillation after percutaneous coronary intervention: insights from the CHUM AF-STENT Registry. Clin Cardiol 43(3):216–221. https://doi.org/10.1002/clc.23316
Lamberts M, Olesen JB, Ruwald MH, Hansen CM, Karasoy D, Kristensen SL, Køber L, Torp-Pedersen C, Gislason GH, Hansen ML (2012) Bleeding after initiation of multiple antithrombotic drugs, including triple therapy, in atrial fibrillation patients following myocardial infarction and coronary intervention: a nationwide cohort study. Circulation 126(10):1185–1193
Limbruno U, De Sensi F, Cresti A, Picchi A, Lena F, De Caterina R (2020) Optimal antithrombotic treatment of patients with atrial fibrillation early after an acute coronary syndrome—triple therapy, dual antithrombotic therapy with an anticoagulant… or, rather, temporary dual antiplatelet therapy? J Clin Med 9(8):2673
Kim HK, Tantry US, Smith SC, Jeong MH, Park S-J, Kim MH, Lim D-S, Shin E-S, Park D-W, Huo Y, Chen S-L, Bo Z, Goto S, Kimura T, Yasuda S, Chen W-J, Chan M, Aradi D, Geisler T, Gorog DA, Sibbing D, Lip GYH, Angiolillo DJ, Gurbel PA, Jeong Y-H (2020) The East Asian paradox: an updated position statement on the challenges to the current antithrombotic strategy in patients with cardiovascular disease. Thromb Haemost 121(04):422–432
Park J, Jung JH, Choi EK, Lee SW, Kwon S, Lee SR, Kang J, Han KD, Park KW, Oh S, Lip GYH (2022) Comparison of early clinical outcomes between dual antiplatelet therapy and triple antithrombotic therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention. PLoS ONE 17(2):e0264538. https://doi.org/10.1371/journal.pone.0264538
Lamberts M, Gislason GH, Olesen JB, Kristensen SL, Schjerning Olsen A-M, Mikkelsen A, Christensen CB, Lip GY, Køber L, Torp-Pedersen C (2013) Oral anticoagulation and antiplatelets in atrial fibrillation patients after myocardial infarction and coronary intervention. J Am Coll Cardiol 62(11):981–989
Fosbol EL, Wang TY, Li S, Piccini J, Lopes RD, Mills RM, Klaskala W, Thomas L, Roe MT, Peterson ED (2013) Warfarin use among older atrial fibrillation patients with non–ST-segment elevation myocardial infarction managed with coronary stenting and dual antiplatelet therapy. Am Heart J 166(5):864–870
Park S, Je NK (2022) Underutilization of anticoagulants in patients with nonvalvular atrial fibrillation in the era of non-vitamin K antagonist oral anticoagulants. Int J Arrhyth 23(1):1–8
Kim L, Kim JA, Kim S (2014) A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health 36:e2014008. https://doi.org/10.4178/epih/e2014008
Service NHI (2015) National health insurance system of Korea. https://www.kobia.kr/skin/bbs/downloads_e2/download.php?tbl=policy_report&no=401
Horiguchi A, Fukaya H, Oikawa J, Shirakawa Y, Kobayashi S, Arakawa Y, Nishinarita R, Nakamura H, Ishizue N, Igarashi G, Satoh A, Kishihara J, Niwano S, Ako J (2019) Real-world antithrombotic therapy in atrial fibrillation patients with a history of percutaneous coronary intervention. Int Heart J 60(6):1321–1327. https://doi.org/10.1536/ihj.19-127
Potter BJ, Andò G, Cimmino G, Ladeiras-Lopes R, Frikah Z, Chen XY, Virga V, Goncalves-Almeida J, Camm AJ, Fox KAA (2018) Time trends in antithrombotic management of patients with atrial fibrillation treated with coronary stents: results from TALENT-AF (The internAtionaL stENT - Atrial Fibrillation study) multicenter registry. Clin Cardiol 41(4):470–475. https://doi.org/10.1002/clc.22898
Investigators TAWGobotA, (2006) Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet 367(9526):1903–1912. https://doi.org/10.1016/S0140-6736(06)68845-4
Başaran Ö, Dogan V, Beton O, Tekinalp M, Aykan AÇ, Kalaycıoğlu E, Bolat I, Taşar O, Şafak Ö, Kalçık M (2017) Impact of valvular heart disease on oral anticoagulant therapy in non-valvular atrial fibrillation: results from the RAMSES study. J Thromb Thrombolysis 43(2):157–165
Hsu JC, Maddox TM, Kennedy K, Katz DF, Marzec LN, Lubitz SA, Gehi AK, Turakhia MP, Marcus GM (2016) Aspirin instead of oral anticoagulant prescription in atrial fibrillation patients at risk for stroke. J Am Coll Cardiol 67(25):2913–2923
Zulkifly H, Lip GY, Lane DA (2017) Bleeding risk scores in atrial fibrillation and venous thromboembolism. Am J Cardiol 120(7):1139–1145
Bocchino PP, Angelini F, Toso E (2021) Atrial fibrillation and coronary artery disease: a review on the optimal use of oral anticoagulants. Rev Cardiovasc Med 22(3):635–648. https://doi.org/10.31083/j.rcm2203074
Wang T-F, Shi L, Nie X, Zhu J (2013) Race/ethnicity, insurance, income and access to care: the influence of health status. Int J Equity Health 12(1):1–7
Kim J, Park S, Kim H, Je NK (2019) National trends in metformin-based combination therapy of oral hypoglycaemic agents for type 2 diabetes mellitus. Eur J Clin Pharmacol 75(12):1723–1730
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener H-C, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, Group ESD (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37(38):2893–2962. https://doi.org/10.1093/eurheartj/ehw210
Kim L, Kim J-A, Kim S (2014) A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health 36:e2014008. https://doi.org/10.4178/epih/e2014008
Kim S, Kim M-S, You S-H, Jung S-Y (2020) Conducting and reporting a clinical research using Korean healthcare claims database. Korean J Fam Med 41(3):146–152. https://doi.org/10.4082/kjfm.20.0062
Acknowledgements
We used the Health Insurance Review & Assessment Service National Inpatient Sample (HIRA-NIS) from 2011 to 2020 (S20220802002) for this study; however, the results have no concern with the Ministry of Health and Welfare or HIRA.
Author information
Authors and Affiliations
Contributions
SP and NKJ conceived and designed the study; HC and YL performed the analysis; HC first drafted the manuscript; All authors participated in drafting the article and approved the final version to be submitted for publication.
Corresponding authors
Ethics declarations
Ethics approval
The study protocol was approved by the Institutional Review Board (IRB) of Pusan National University, Busan, Korea (PNU IRB/2022_116_HR).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choi, HJ., Lee, Y., Park, S. et al. Utilization of triple antithrombotic therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention. Eur J Clin Pharmacol 79, 541–551 (2023). https://doi.org/10.1007/s00228-023-03468-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03468-6