Abstract
Purpose
To determine the impact of drug prescribing pattern, outpatient drug price of medicines, and level of adherence to evidence-based international guidelines on blood pressure (BP) control at selected hospitals in Southern Ethiopia.
Methods
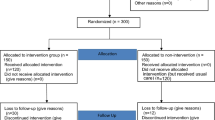
Hospital-based cross-sectional study was conducted. The data entry and analysis were done by using SPSS version 21.0.
Results
A mean age of participants was 55.87 ± 11.02 years. The rate of BP control was 17.5% based on International Society of Hypertension (ISH) guidelines 2020. In about two-thirds of patients, 270 (66.5%) were taking combination therapy. Mean annual cost of drugs for hypertension was 11.39 ± 3.98 US dollar (USD). Treatment was affordable for only 91 (22.4%) of patients. There was considerable variation on prescriber’s adherence to evidence-based guidelines. Body mass index (BMI) of 18–24.9 kg/m2, adjusted odds ratio (AOR) = 3.63 (95% confidence interval (C.I), 1.169–11.251, p = 0.026), physically activity, AOR = 12.69 (95% C.I, 1.424–113.17, p = 0.023), presence of no comorbidity, AOR = 12.82 (95% C.I, 4.128–39.816, p = 0.000), and taking affordable antihypertensive regimen, AOR = 3.493 (95% C.I, 1.4242–9.826, p = 0.018), were positively associated BP control.
Conclusion
The level of BP control, affordability of drugs for the management of hypertension and related comorbidities, and the prescriber’s adherence to evidence-based guidelines were inadequate. Therefore, addressing factors associated with good BP control including affordability and clinician adherence to evidence-based guidelines by responsible stakeholders could improve BP control and reduce associated complications.


Similar content being viewed by others
Availability of data and materials
All the data reported in the manuscript are publicly available upon acceptance of the manuscript.
References
Collaborators GRF (2018) Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1923–94
Cappuccio FP, Miller MA (2016) Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med 11(3):299–305
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D et al (2020) 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 75(00):1–25
Geldsetzer P, Manne-Goehler J, Marcus ME, Ebert C, Zhumadilov Z, Wesseh CS, Tsabedze L, Supiyev A, Sturua L, Bahendeka SK, Sibai AM (2019) The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1·1 million adults. Lancet 6736(19):30955–9
Institute EPH (2016) Ethiopia steps report on risk factors for chronic non-communicable diseases and prevalence of selected NCDs
Gerba H, Yegezu Y, Ejigu E, Giorgis A (2017) Pharmaceutical sector assessment in Ethiopia: food medicine and health care administration and control authority. 1–64
Sorato MM, Davari M, Kebriaeezadeh A (2019) Health care system response to cardiovascular diseases, trends from 2010–2018: can Ethiopia achieve 2025 global voluntary targets for non-communicable diseases from cardiovascular diseases perspective? Explanatory review of available literatures. Research & Reviews: J Med Health Sci 9(1):1–13
Health FDRoEMo (2015) Health sector transformation plan (2015/16–2019/20). Ministry of Health Addis Ababa
Health FDRoEMo (2010) Health sector development program IV, 2010/11—2014/15. Ministry of Health Addis Ababa; 2010.
Agency TfdroEcs (2018) The 2015/16 Ethiopian household consumption expenditure (HCE) survey results for country level statistical report January 2018 Addis Ababa. Stat Bulletin 585:1-272
Shiferaw F, Letebo M, Misganaw A, Feleke Y, Gelibo T, Getachew T et al (2018) Non-communicable diseases in Ethiopia: disease burden, gaps in health care delivery and strategic directions. Ethiop J Health Dev 32(3)
Elzinga G, Jerene D, Mesfin G, Negussie S (2010) Human resources for health implications of scaling up for universal access to HIV/AIDS prevention, treatment, and care: Ethiopia rapid situational analysis. Group GHWATW, editor Addis Ababa, Ethiopia
Getachew T, Bekele A, Amenu K, Defar A, Teklie H, Taye G et al (2017) Service availability and readiness for major non-communicable diseases at health facilities in Ethiopia. Ethiopian Journal of Health Development 31(1):384–390
Whelton PK CR, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension (Dallas, Tex : 1979) 71:e13-e115
Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS et al (2019) Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 393(10184):1958–1972
Yazdanshenas H, Bazargan M, Orum G, Loni L, Mahabadi N, Husaini B (2014) Prescribing patterns in the treatment of hypertension among underserved African American elderly. Ethn Dis 24(4):431–437
Adler AJ, Prabhakaran D, Bovet P, Kazi DS, Mancia G, Mungal-Singh V, Poulter N (2015) Reducing cardiovascular mortality through prevention and management of raised blood pressure. A world heart federation road map. Global Heart 10(2):111–22
Arshad V, Samad Z, Das J, Almas A, Rashid N, Virani SS et al (2020) Prescribing patterns of antihypertensive medications in low- and middle-income countries: a systematic review. Asia Pacific Journal of Public Health 33(1):14–22
World Health Organization (2003) Introduction to drug utilization research: World Health Organization
Shalini S, Ravichandran V, Mohanty B, Dhanaraj S, Saraswathi R (2010) Drug utilization studies-an overview. Inter J Pharmaceut Sci Nanotechnol 31:803–810
Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, Brock D et al (2014) Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Eff Resour Alloc 12:18
World Health Organization (2019) It’s time to walk the talk: WHO independent high-level commission on noncommunicable diseases final report. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO
Ruhil R (2018) The changing wealth of nations 2018. Building a sustainable future. By Glenn-Marie Lange, Quentin Wodon and Kevin Carey; Washington DC: World Bank Group.© World Bank. IASSI-Quarterly 37(1):135–7
World Health Organization (2009) WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2010. Oslo [cited 2010 Sep 10]
Xu H, He Y, Xu L, Yan X, Dai H (2015) Trends and patterns of five antihypertensive drug classes between 2007 and 2012 in China using hospital prescription data. Int J Clin Pharmacol Ther 53(6):430–437
Statistics ABo (2013) Australian health survey: health service usage and health related actions, 2011–12. ABS Canberra
Health AIo, Welfare (2017) Medicines for cardiovascular disease. Canberra: AIHW
Jarari N, Rao N, Peela JR, Ellafi KA, Shakila S, Said AR et al (2016) A review on prescribing patterns of antihypertensive drugs. Clinical Hypertension 22(1):7
Beaglehole R, Bonita R, Ezzati M, Alleyne G, Dain K, Kishore SP et al (2014) NCD Countdown 2025: accountability for the 25× 25 NCD mortality reduction target. The Lancet 384(9938):105–107
Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, Tafatatha T et al (2018) Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol 6(3):208–222
Goverwa TP, Masuka N, Tshimanga M, Gombe NT, Takundwa L, Bangure D et al (2014) Uncontrolled hypertension among hypertensive patients on treatment in Lupane District, Zimbabwe, 2012. BMC Res Notes 7(1):703
Muleta S, Melaku T, Chelkeba L, Assefa D (2017) Blood pressure control and its determinants among diabetes mellitus comorbid hypertensive patients at Jimma University Medical Center, South West Ethiopia. . Clin Hypertension 3(29)
Gebremichael GB, Berhe KK, Zemichael TM (2019) Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Cardiovascular Disorders 19(121)
Yazie DSW, Alebachew M, Berha AB (2018) Assessment of blood pressure control among hypertensive patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia: a cross-sectional study. J Bioanal Biomed 10:80–87
Berhe DF, Taxis K, Haaijer-Ruskamp FM, Mulugeta A, Mengistu YT, Mol PGM (2017) Hypertension treatment practices and its determinants among ambulatory patients: retrospective cohort study in Ethiopia. BMJ Open 7(8):e015743
Rachlis B, Naanyu V, Wachira J, Genberg B, Koech B, Kamene R et al (2016) Community perceptions of community health workers (CHWs) and their roles in management for HIV, tuberculosis and hypertension in Western Kenya. PLoS ONE 11(2):e0149412
Woldegebriel AS, Gudina EK, Alemu DT (2016) Assessment of blood pressurecontrol among hypertensive patients in Southwest Ethiopia. PLoS ONE 11(11)
Muleta S, Melaku T, Chelkeba L, Assefa D (2017) Blood pressure control and its determinants among diabetes mellitus co-morbid hypertensive patients at Jimma University Medical Center. South West Ethiopia Clin Hypertens 23:29
World Health Organization (2013) Global action plan for the prevention and control of non-communicable diseases 2013–2020
Teshome DFDA, Zeleke BM (2018) Determinants of blood pressure control amongst hypertensive patients in Northwest Ethiopia. PLoS ONE 13(5)
World Health Organization (2016) Final report of the Commission on Ending Childhood Obesity
Gareth Beevers GYHL, Eoin O'Brien (2014) ABC of hypertension. Sixth edition ed. Series A, editor
Arnett DKBR, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd-Jones D, McEvoy JW, Michos ED, Miedema MD, Muñoz D, Smith SC Jr, Virani SS, Williams KA Sr, Yeboah J, Ziaeian B (2019) ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140:e563–e595
Shrestha PL, Shrestha PA, Vivo RP (2016) Epidemiology of comorbidities in patients with hypertension. Curr Opin Cardiol 31(4):376–380
Noh J, Kim HC, Shin A, Yeom H, Jang S-Y, Lee JH et al (2016) Prevalence of comorbidity among people with hypertension: the Korea National Health and Nutrition Examination Survey 2007–2013. kcj 46(5):672–80
Noh J, Kim HC, Shin A, Yeom H, Jang S-Y, Lee JH et al (2016) Prevalence of comorbidity among people with hypertension: the Korea National Health and Nutrition Examination Survey 2007–2013. Korean Circ J 46(5):672–680
Wang J, Ma JJ, Liu J, Zeng DD, Song C, Cao Z (2017) Prevalence and risk factors of comorbidities among hypertensive patients in China. Int J Med Sci 14(3):201
Shukrala F, Gabriel T (2015) Assessment of prescribing, dispensing, and patient use pattern of antihypertensive drugs for patients attending outpatient department of Hiwot Fana Specialized University Hospital, Harar. Eastern Ethiopia Drug Des Devel Ther 9:519–523
Kim SH, Shin DW, Kim S, Han K, Park S-h, Kim Y-H et al (2019) Prescribing patterns of antihypertensives for treatment-naïve patients in South Korea: from Korean NHISS claim data. Int J Hypertension 2019.
Busser D, Yarlagadda R, Ahmed SM (2016) Assessment of antihypertensive drugs utilization pattern in Butajira Zonal Hospital, Butajira Town, South Ethiopia. Int J Pharm Sci Res 7(10):4028
Fufa F, Mirkano D, Tipathi R (2015) Prescription pattern and potential drug-drug interactions of antihypertensive drugs in a general hospital, South Ethiopia. Cukurova Med J 40:698–706
Abegaz TM, Tefera YG, Abebe TB (2017) Antihypertensive drug prescription patterns and their impact on outcome of blood pressure in Ethiopia: a hospital-based cross-sectional study. Integr Pharm Res Pract 6:29–35
Eslampanah Z (2016) Drug utilization evaluation of anti-hypertensive agents in a medical care hospital. Int J Pharm Sci Res 7(2):862
Catić T, Begović B (2011) Outpatient antihypertensive drug utilization in Canton Sarajevo during five years period (2004–2008) and adherence to treatment guidelines assessment. Bosn J Basic Med Sci 11(2):97–102
Ishida T, Oh A, Hiroi S, Shimasaki Y, Tsuchihashi T (2019) Current prescription status of antihypertensive drugs in Japanese patients with hypertension: analysis by type of comorbidities. Clin Exp Hypertens 41(3):203–210
Ahmed A, Saqlain M, Tanveer M, Nawaz MS, Rehman K, Safdar A et al (2021) Prescribing patterns of antihypertensive drugs in patients attending tertiary care hospitals in Pakistan. SN Comprehensive Clinical Medicine 3(1):176–182
Ng J-M, Kua KP, Lee SWH (2020) Prescribing patterns of antihypertensive medications and blood pressure control among hypertensive patients in a primary care setting in Malaysia. Prog Drug Discov Biomed Sci 3(1)
Paradkar SG, Sinha SR (2018) Drug utilization among hypertensive patients in the outpatient department of medicine in a tertiary care hospital: a cross-sectional study. Clin Exp Hypertens 40(2):150–154
Grimmsmann T, Himmel W (2011) Discrepancies between prescribed and defined daily doses: a matter of patients or drug classes? Eur J Clin Pharmacol 67(8):847–854
Attaei MW, Khatib R, McKee M, Lear S, Dagenais G, Igumbor EU et al (2017) Availability and affordability of blood pressure-lowering medicines and the effect on blood pressure control in high-income, middle-income, and low-income countries: an analysis of the PURE study data. The Lancet Public Health 2(9):e411–e419
Rachana P, Anuradha H (2014) Anti hypertensive prescribing patterns and cost analysis for primary hypertension: a retrospective study. Journal of clinical and diagnostic research: JCDR 8(9):HC19
Umegbolu EI (2017) Prescribing patterns in systemic hypertension and pharmaco-economics (cost effectiveness and cost minimisation analyses) of the commonly prescribed antihypertensives in a district hospital in Enugu State, Southeast Nigeria. 2017;6(1):7
Mensa Sorato M, Davari M, Abdollahi Asl A, Soleymani F, Kebriaeezadeh A (2020) Why healthcare market needs government intervention to improve access to essential medicines and healthcare efficiency: a scoping review from pharmaceutical price regulation perspective. J Pharm Health Serv Res 11(4):321–333
Sorato MM, Davari M, AbdollahiAsl A (2020) Descriptive evaluation of national and international hypertension treatment guidelines: the guideline quality and comprehensiveness to provide care to adult with hypertension. Clinical Medical Reviews and Case Reports 7(5):1–14
Pittrow D, Kirch W, Bramlage P, Lehnert H, Höfler M, Unger T et al (2004) Patterns of antihypertensive drug utilization in primary care. Eur J Clin Pharmacol 60(2):135–142
Elliott WJ (2008) What factors contribute to the inadequate control of elevated blood pressure? The Journal of Clinical Hypertension 10:20–26
Hyman DJ, Pavlik VN, Greisinger AJ, Chan W, Bayona J, Mansyur C et al (2012) Effect of a physician uncertainty reduction intervention on blood pressure in uncontrolled hypertensives–a cluster randomized trial. J Gen Intern Med 27(4):413–419
Neutel JM (2008) Prescribing patterns in hypertension: the emerging role of fixed-dose combinations for attaining BP goals in hypertensive patients. Curr Med Res Opin 24(8):2389–2401
Fretheim A, Oxman AD (2005) International variation in prescribing antihypertensive drugs: Its extent and possible explanations. BMC Health Serv Res 5(1):21
Acknowledgements
We would like to thank all patients who participated in this study for their valuable dedication to providing information. We would also like to thank Arba Minch University College of Medicine and Health Sciences and Tehran University Medical Sciences, Department of Pharmacoeconomics and Pharmaceutical Administration staff for their technical and material support during this manuscript development.
Author information
Authors and Affiliations
Contributions
All authors read and approved the manuscript. MM conceived the study, conducted the study, and developed the manuscript; MD participated in data analysis and reviewed the manuscript and AK reviewed the manuscript and write-up process; NS and TS participated in literature review and polished the language of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Tehran University of Medical Sciences, Faculty of Pharmacy, Department of Pharmacoeconomics, and Pharmaceutical Administration ethical review board with approval ID: IR.TUMS.MEDICINE.REC.1399.674 and Arba Minch University College of Medicine and Health Sciences Institutional review board with reference number: IRB/T10/2012. After clarifying the study objective and confidentiality of the information, verbal informed consent was obtained from each respective hospital before data collection.
Consent for publication
All authors read the full version of this manuscript and agreed to publish.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sorato, M.M., Davari, M., Kebriaeezadeh, A. et al. Antihypertensive prescribing pattern, prescriber adherence to ISH 2020 guidelines, and implication of outpatient drug price on blood pressure control at selected hospitals in Southern Ethiopia. Eur J Clin Pharmacol 78, 1487–1502 (2022). https://doi.org/10.1007/s00228-022-03352-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-022-03352-9