Abstract
Purpose
The purpose of this study was to evaluate the impact of tacrolimus drug monitoring parameters on the incidence of acute cellular rejection (ACR) in lung transplant recipients (LTRs).
Methods
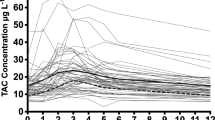
This was a retrospective study of patients who underwent lung transplantation at a single center. LTRs who were given tacrolimus during the first 6 months after transplantation and who underwent at least one bronchoscopy with biopsy were included. Tacrolimus time in therapeutic range (TTR) was calculated using Rosendaal’s method. Time to therapeutic level, coefficient of variance (CoV), and median trough concentrations were also determined.
Results
The study included 157 LTRs. ACR ≥ A1 grade was present in 46.5% of patients, and ACR ≥ A2 grade was present in 17.2%. There was no difference between tacrolimus TTR in patients with ACR ≥ A1 compared with those without ACR (47.4 ± 16.1 versus 46.2 ± 18.9%, p = 0.67) or in patients with ACR ≥ A2 grade compared with those with A0 or A1 ACR (46.0 ± 16.3 versus 47.0 ± 17.9%, p = 0.81). When comparing patients with any ACR grade A1 or higher with those without ACR, there was no difference in tacrolimus CoV (42.7 ± 11.0 versus 44.6 ± 12.4, p = 0.30), median tacrolimus trough concentration (9.9 ± 1.3 versus 9.8 ± 1.4 ng/mL, p = 0.66), or days to therapeutic level (9 versus 12 days, p = 0.057).
Conclusions
The results suggest that tacrolimus TTR, time in therapeutic range, and variability are not related to the presence of ACR in LTRs.
Similar content being viewed by others
Data availability
Not applicable
References
Chambers DC, Cherikh WS, Harhay MO, Hayes D Jr, Hsich E, Khush KK, Meiser B, Potena L, Rossano JW, Toll AE, Singh TP, Sadavarte A, Zuckermann A, Stehlik J, H. International Society for and T. Lung (2019) The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-sixth adult lung and heart-lung transplantation report-2019; Focus theme: Donor and recipient size match. J Heart Lung Transplant 38(10):1042–1055
Treede H, Klepetko W, Reichenspurner H, Zuckermann A, Meiser B, Birsan T, Wisser W, Reichert B, Munich and G. Vienna Lung Transplant (2001) Tacrolimus versus cyclosporine after lung transplantation: a prospective, open, randomized two-center trial comparing two different immunosuppressive protocols. J Heart Lung Transplant 20(5):511–517
Hachem RR, Yusen RD, Chakinala MM, Meyers BF, Lynch JP, Aloush AA, Patterson GA, Trulock EP (2007) A randomized controlled trial of tacrolimus versus cyclosporine after lung transplantation. J Heart Lung Transplant 26(10):1012–1018
Stewart S, Fishbein MC, Snell GI, Berry GJ, Boehler A, Burke MM, Glanville A, Gould FK, Magro C, Marboe CC, McNeil KD, Reed EF, Reinsmoen NL, Scott JP, Studer SM, Tazelaar HD, Wallwork JL, Westall G, Zamora MR, Zeevi A, Yousem SA (2007) Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection. J Heart Lung Transplant 26(12):1229–1242
Hachem RR (2017) Acute rejection and antibody-mediated rejection in lung transplantation. Clin Chest Med 38(4):667–675
Parulekar AD, Kao CC (2019) Detection, classification, and management of rejection after lung transplantation. J Thorac Dis 11(Suppl 14):S1732–S1739
Martinu T, Pavlisko EN, Chen DF, Palmer SM (2011) Acute allograft rejection: cellular and humoral processes. Clin Chest Med 32(2):295–310
Sikma MA, van Maarseveen EM, van de Graaf EA, Kirkels JH, Verhaar MC, Donker DW, Kesecioglu J, Meulenbelt J (2015) Pharmacokinetics and toxicity of tacrolimus early after heart and lung transplantation. Am J Transplant 15(9):2301–2313
Ivulich S, Dooley M, Kirkpatrick C, Snell G (2017) Clinical challenges of tacrolimus for maintenance immunosuppression post-lung transplantation. Transplant Proc 49(9):2153–2160
Ryu JH, Choi S, Lee HJ, Kim YT, Kim YW, Yang J (2019) Low early posttransplant serum tacrolimus levels are associated with poor patient survival in lung transplant patients. Ann Thorac Med 14(3):186–191
Chiang CY, Schneider HG, Levvey B, Mitchell L, Snell GI (2013) Tacrolimus level variability is a novel measure associated with increased acute rejection in lung transplant (LTX) recipients. Journal of Heart and Lung Transplantation 32(4):S170
Ensor CR, Iasella CJ, Harrigan KM, Morrell MR, Moore CA, Shigemura N, Zeevi A, McDyer JF, Venkataramanan R (2018) Increasing tacrolimus time-in-therapeutic range is associated with superior one-year outcomes in lung transplant recipients. Am J Transplant 18(6):1527–1533
Gallagher HM, Sarwar G, Tse T, Sladden TM, Hii E, Yerkovich ST, Hopkins PM, Chambers DC (2015) Erratic tacrolimus exposure, assessed using the standard deviation of trough blood levels, predicts chronic lung allograft dysfunction and survival. J Heart Lung Transplant 34(11):1442–1448
Wallemacq P, Goffinet JS, O’Morchoe S, Rosiere T, Maine GT, Labalette M, Aimo G, Dickson D, Schmidt E, Schwinzer R, Schmid RW (2009) Multi-site analytical evaluation of the Abbott ARCHITECT tacrolimus assay. Ther Drug Monit 31(2):198–204
Rosendaal FR, Cannegieter SC, van der Meer FJ, Briet E (1993) A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 69(3):236–239
Diannelidou-Stamelou L, Spurr L, Leaver N, Smith J, Simon A, Carby M, Reed A, Wei L, Lyster H (2017) Intra-patient variability of tacrolimus levels and lung allograft outcomes: a single centre experience. Journal of Heart and Lung Transplantation 36(4):S367–S368
Miano TA, Flesch JD, Feng R, Forker CM, Brown M, Oyster M, Kalman L, Rushefski M, Cantu E 3rd, Porteus M, Yang W, Localio AR, Diamond JM, Christie JD, Shashaty MGS (2020) Early tacrolimus concentrations after lung transplant are predicted by combined clinical and genetic factors and associated with acute kidney injury. Clin Pharmacol Ther 107(2):462–470
Benazzo A, Schwarz S, Muckenhuber M, Schweiger T, Murakozy G, Moser B, Siguenza JM, Lang G, Taghavi S, Klepetko W, Hoetzenecker K, Jaksch P, Lambers C (2019) Alemtuzumab induction combined with reduced maintenance immunosuppression is associated with improved outcomes after lung transplantation: a single centre experience. PLoS One 14(1):e0210443
Garrity ER Jr, Villanueva J, Bhorade SM, Husain AN, Vigneswaran WT (2001) Low rate of acute lung allograft rejection after the use of daclizumab, an interleukin 2 receptor antibody. Transplantation 71(6):773–777
Penninga L, Moller CH, Penninga EI, Iversen M, Gluud C, Steinbruchel DA (2013) Antibody induction therapy for lung transplant recipients. Cochrane Database Syst Rev 11:CD008927
Husain S, Zaldonis D, Kusne S, Kwak EJ, Paterson DL, McCurry KR (2006) Variation in antifungal prophylaxis strategies in lung transplantation. Transpl Infect Dis 8(4):213–218
Baughman RP, Meyer KC, Nathanson I, Angel L, Bhorade SM, Chan KM, Culver D, Harrod CG, Hayney MS, Highland KB, Limper AH, Patrick H, Strange C, Whelan T (2012) Monitoring of nonsteroidal immunosuppressive drugs in patients with lung disease and lung transplant recipients: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 142(5):e1S–e111S
Pawelec G, Ehninger G, Rehbein A, Schaudt K, Jaschonek K (1991) Comparison of the immunosuppressive activities of the antimycotic agents itraconazole, fluconazole, ketoconazole and miconazole on human T-cells. Int J Immunopharmacol 13(2–3):299–304
Saint-Marcoux F, Knoop C, Debord J, Thiry P, Rousseau A, Estenne M, Marquet P (2005) Pharmacokinetic study of tacrolimus in cystic fibrosis and non-cystic fibrosis lung transplant patients and design of Bayesian estimators using limited sampling strategies. Clin Pharmacokinet 44(12):1317–1328
Author information
Authors and Affiliations
Contributions
All authors contributed to study conception and design. Data collection was performed by Christina Kao and Justin Segraves. The first draft of the manuscript was prepared by Christina Kao and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the Institutional Review Board of Baylor College of Medicine with waiver of consent.
Consent to participate
Not applicable
Consent for publication
Not applicable
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kao, C.C., Segraves, J. & Parulekar, A.D. Tacrolimus monitoring parameters are not associated with acute cellular rejection following lung transplantation. Eur J Clin Pharmacol 77, 63–69 (2021). https://doi.org/10.1007/s00228-020-02976-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-02976-z