Abstract
Purpose
Ertapenem is used off-label to treat osteoarticular infections but there are few pharmacokinetic (PK) data to guide optimal dosing strategies in patients who may be obese with multiple co-morbidities including diabetes and peripheral vascular disease.
Methods
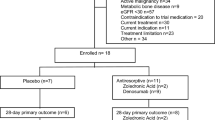
Participants undergoing lower limb amputation or elective joint arthroplasty received a dose of intravenous ertapenem prior to surgery. Eight plasma samples were collected over 24 h, together with at least one bone sample per patient. Ertapenem concentrations in plasma and bone were measured using liquid-chromatography/mass-spectroscopy and analysed using non-linear mixed effects PK modelling.
Results
Plasma and bone concentrations were obtained from 10 participants. The final population PK model showed that a fat free body mass was the most appropriate body size adjustment. Ertapenem diffused rapidly into bone but concentrations throughout the 24 h dosing period were on average 40-fold higher in plasma, corresponding to a bone to plasma ratio of 0.025, and highly variable between individuals. Simulations demonstrated a high probability of target attainment (PTA) for free plasma concentrations when the minimum inhibitory concentrations (MIC) were ≤ 0.25 mg/L. By contrast, at MICs of 0.5 mg/L and ≥ 1 mg/L, the fractions of patients attaining this target was ~ 80% and 40%, respectively. In bone, the PTA was ≤ 45% when the MIC was ≥ 0.25 mg/L.
Conclusion
Local bone and free plasma concentrations appear adequate for osteoarticular infections where Enterobacteriaceae are the main causative pathogens, but for Staphylococcus aureus and other bacteria, conventional dosing may lead to inadequate PTA.


Similar content being viewed by others
References
Perez F, Endimiani A, Hujer KM, Bonomo RA (2007) The continuing challenge of ESBLs. Curr Opin Pharmacol 7(5):459–469. https://doi.org/10.1016/j.coph.2007.08.003
Lipsky BA, Armstrong DG, Citron DM, Tice AD, Morgenstern DE, Abramson MA (2005) Ertapenem versus piperacillin/tazobactam for diabetic foot infections (SIDESTEP): prospective, randomised, controlled, double-blinded, multicentre trial. Lancet 366(9498):1695–1703. https://doi.org/10.1016/S0140-6736(05)67694-5
Goswami ND, Johnson MD, Chu VH (2011) Ertapenem for treatment of osteomyelitis: a case series. BMC Res Notes 4:478. https://doi.org/10.1186/1756-0500-4-478
Chen M, Nafziger AN, Drusano GL, Ma L, Bertino JS Jr (2006) Comparative pharmacokinetics and pharmacodynamic target attainment of ertapenem in normal-weight, obese, and extremely obese adults. Antimicrob Agents Chemother 50(4):1222–1227. https://doi.org/10.1128/AAC.50.4.1222-1227.2006
Nijland HM, Ruslami R, Stalenhoef JE, Nelwan EJ, Alisjahbana B, Nelwan RH, van der Ven AJ, Danusantoso H, Aarnoutse RE, van Crevel R (2006) Exposure to rifampicin is strongly reduced in patients with tuberculosis and type 2 diabetes. Clin Infect Dis 43(7):848–854. https://doi.org/10.1086/507543
Landersdorfer CB, Bulitta JB, Kinzig M, Holzgrabe U, Sorgel F (2009) Penetration of antibacterials into bone: pharmacokinetic, pharmacodynamic and bioanalytical considerations. Clin Pharmacokinet 48(2):89–124. https://doi.org/10.2165/0003088-200948020-00002
Boselli E, Breilh D, Djabarouti S, Bel JC, Saux MC, Allaouchiche B (2007) Diffusion of ertapenem into bone and synovial tissues. J Antimicrob Chemother 60(4):893–896. https://doi.org/10.1093/jac/dkm296
Majumdar AK, Musson DG, Birk KL, Kitchen CJ, Holland S, McCrea J, Mistry G, Hesney M, Xi L, Li SX, Haesen R, Blum RA, Lins RL, Greenberg H, Waldman S, Deutsch P, Rogers JD (2002) Pharmacokinetics of ertapenem in healthy young volunteers. Antimicrob Agents Chemother 46(11):3506–3511
European Committee on Antimicrobial Susceptibility Testing (EUCAST) (2016) MIC distributions and ECOFFs. In: EUCAST (Ed.) ed.
Green B, Duffull SB (2004) What is the best size descriptor to use for pharmacokinetic studies in the obese? Br J Clin Pharmacol 58(2):119–133. https://doi.org/10.1111/j.1365-2125.2004.02157.x
Anderson BJ, Holford NH (2008) Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol 48:303–332. https://doi.org/10.1146/annurev.pharmtox.48.113006.094708
Borracci T, Adembri C, Accetta G, Berti J, Cappellini I, Lucchese M, Biggeri A, De Gaudio AR, Novelli A (2014) Use of the parenteral antibiotic ertapenem as short term prophylaxis in bariatric surgery: a pharmaco-kinetic-pharmacodynamic study in class III obese female patients. Minerva Anestesiol 80(9):1005–1011
Wittau M, Paschke S, Kurlbaum M, Scheele J, Ly NS, Hemper E, Kornmann M, Henne-Bruns D, Bulitta JB (2017) Population pharmacokinetics and target attainment of ertapenem in plasma and tissue assessed via microdialysis in morbidly obese patients after laparoscopic visceral surgery. Antimicrob Agents Chemother 61 (1) https://doi.org/10.1128/AAC.00952-16
Raymakers JT, Houben AJ, van der Heyden JJ, Tordoir JH, Kitslaar PJ, Schaper NC (2001) The effect of diabetes and severe ischaemia on the penetration of ceftazidime into tissues of the limb. Diabet Med 18(3):229–234
Vuorisalo S, Pokela R, Satta J, Syrjala H (2000) Internal mammary artery harvesting and antibiotic concentrations in sternal bone during coronary artery bypass. Int J Angiol 9(2):78–81
Grimer RJ, Karpinski MR, Andrews JM, Wise R (1986) Penetration of amoxycillin and clavulanic acid into bone. Chemotherapy 32(3):185–191
Funding
This study was funded through a Fremantle Hospital Medical Research Foundation grant and NHMRC project grant 1047105. TMED is supported by an NHMRC Practitioner Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This prospective, single group, longitudinal PK study of single-dose intravenous ertapenem was approved by the Fremantle Hospital Human Research Ethics Committee (13/4) and all patients gave informed consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Figure 1
Extraction efficiency of ertapenem from bone according to time. (PNG 184 kb)
Supplementary Figure 2
Goodness-of-fit plots for ertapenem in plasma (A) and bone (B), including observed concentrations against population and individual predicted concentrations, and weighted residuals against time from dose and population predicted concentrations. (PNG 435 kb)
ESM 3
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Chambers, J., Page-Sharp, M., Salman, S. et al. Ertapenem for osteoarticular infections in obese patients: a pharmacokinetic study of plasma and bone concentrations. Eur J Clin Pharmacol 75, 511–517 (2019). https://doi.org/10.1007/s00228-018-2597-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-018-2597-z