Abstract
Purpose
To investigate associations between antidepressant use patterns and risk of fatal and non-fatal suicidal behaviours in older adults who initiated antidepressant therapy.
Method
A national population-based cohort study conducted among Swedish residents aged ≥ 75 years who initiated antidepressant treatment. Patients who filled antidepressant prescriptions between January 1, 2007 and December 31, 2013 (N = 185,225) were followed until December 31, 2014. Sub-hazard ratios of suicides and suicide attempts associated with use patterns of antidepressants, adjusting for potential confounders such as serious depression were calculated using the Fine and Gray regression models.
Results
During follow-up, 295 suicides and 654 suicide attempts occurred. Adjusted sub-hazard ratios (aSHRs) were increased for both outcomes in those who switched to another antidepressant (aSHR for suicide 2.42, 95% confidence interval 1.65 to 3.55, and for attempt 1.76, 1.32 to 2.34). Elevated suicide risks were also observed in those who concomitantly filled anxiolytics (1.54, 1.20 to 1.96) and hypnotics (2.20, 1.69 to 2.85). Similar patterns were observed for the outcome suicide attempt. Decreased risk of attempt was observed among those with concomitant use of anti-dementia drugs (0.40, 0.27 to 0.59).
Conclusion
Switching antidepressants, as well as concomitant use of anxiolytics or hypnotics, may constitute markers of increased risk of suicidal behaviours in those who initiate antidepressant treatment in very late life. Future research should consider indication biases and the clinical characteristics of patients initiating antidepressant therapy.
Similar content being viewed by others
Background
Older populations, in particular older men, tend to have the highest rates of suicide in many countries worldwide [1, 2]. Depression is common in older adults who die by suicide, and it has been estimated that three quarters of all late-life suicides could be prevented, if depression could be successfully treated [3].
There is some evidence that antidepressant therapy is associated with decreased risk of suicide in late life [4, 5]. However, there is a need for studies that focus specifically on the oldest segment of the population. Clinical trials tend to exclude older persons often due to physical frailty [6]. This is problematic as medication use patterns, treatment response and side effects may all differ between younger and older users of antidepressants, due to higher levels of psychiatric and somatic comorbidities in the older group, as well as age-related physiological changes [7, 8].
Given the fact that the identification and subsequent treatment of late life depression is a major suicide prevention strategy [9, 10], it is surprising that only a few pharmacoepidemiological studies investigate how different use patterns of antidepressants may impact on the risk of suicide in older adults [11, 12]. We could find no population-based studies providing risk estimates for concomitant use of psychoactive drugs in this high-risk age group. The latter is important as sedatives and hypnotics are widely prescribed for older patients with depression, and these medications may be related to increased risk of suicide [13, 14]. We have previously presented data demonstrating that anxiolytics and hypnotics, but not antidepressants, were associated with increased suicide risk in older adults after adjustment for confounding by indication [15]. That study was small and based on retrospective information, and potential associations with suicidal behaviour need to be examined using large, prospective data sets.
The aim of the present study was to investigate the association between antidepressant use patterns and the risk of suicide and suicide attempt in a national population-based cohort of older Swedish adults who initiated antidepressant therapy. Considering the fact that suicide rates are particularly high in the oldest age group, we chose to focus on those aged 75 years and above.
Methods
Study design
We conducted a prospective cohort study employing data from several national registers, linked by the unique personal identity number [16].
Study population and study period
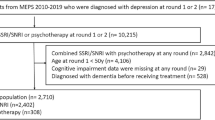
The study population comprised all Swedish residents aged ≥ 75 years who initiated antidepressant treatment between January 1, 2007 and December 31, 2013. Those who filled a prescription for an antidepressant during this period with no such fills during the preceding year were considered treatment initiators. The new-user design minimised confounding [17]. The cohort (N = 185,225) was followed from the date of first filled prescription, denoted the index date, until December 31, 2014 or until migration or death. The study flow diagram is presented in Online Resource 1.
Data sources
The Swedish Prescribed Drug Register (SPDR) was used to identify antidepressant initiators and patterns of drug use. The SPDR has full coverage of filled prescriptions in outpatient care [18]. It includes information on dispensed medications, dispensed quantity, number of defined daily doses and prescribed daily doses in free text. The National Patient Register [19] was used to identify individuals with diagnosis of suicide attempt. This register includes up to 30 diagnoses for specialised in- and outpatient care based on the International Classification of Diseases, 10th version (ICD-10). Thus, the National Patient Register captures cases of depression requiring specialist services. For the purpose of this study, individuals with a depression diagnosis, as identified by the National Patient Register, are considered to have serious depression. Data on cause of death, including suicide, were collected from the Cause of Death Register. Persons residing in nursing homes were identified by social service data from the National Board of Health and Welfare. Statistics Sweden provided information on migration during the follow-up period.
Exposure measures: medication use patterns
Antidepressants were defined as substances included in the Anatomical Therapeutic Chemical group (ATC-group) N06A [20]. We grouped antidepressants into major classes: tricyclic antidepressants (TCAs) (N06AA), selective serotonin reuptake inhibitors (SSRIs) (N06AB), serotonin-norepinephrine reuptake inhibitors and norepinephrine reuptake inhibitors (SNRIs/NRIs) (N06AX21, N06AX16, N06AX18), and other antidepressant medications.
We defined early discontinuation as not refilling any antidepressant medication within 180 days after the index date. Combination use was defined as the fill of two or more different antidepressants within 180 days following the index date, with the first antidepressant refilled after the purchase of the second antidepressant. Switching was defined as filling two or more different antidepressant substances within 180 days following the index date without a new refill of the index antidepressant after the fill of the new antidepressant. In Sweden, patients can purchase 3 months’ supply at each fill within the Pharmaceutical Benefits Scheme; in practice, packages of approximately 100 units are often dispensed. In addition, start packages covering up to 1 month’s supply of medication are sometimes dispensed when initiating a new treatment. To avoid misclassifying new users who did not have a start package when initiating their therapy, or with late refill of their medications, we applied the conservative period of 180 days after initiating the therapy to define different use patterns of antidepressants.
We estimated the patients’ adherence to their antidepressant therapy by the medication possession ratio (MPR), which measures the proportion of days’ supply during the observation period. The number of days’ supply was calculated by dividing the total number of filled prescribed doses by the number of estimated prescribed daily doses (PDDs). We estimated a theoretical substance-specific PDD based on a review of drug strength and dosage instructions among a sample of the study population, and a PDD/defined daily dose (DDD) was calculated for each substance. We assumed that the theoretical PDD was similar for multidose users [21]. For substances with few users and for those lacking dosage instructions, a theoretical PDD was set at 0.5 DDD. Non-adherence was defined as MPR < 80% [22].
Concurrent use of other psychotropic medications was defined as filling a prescription for another psychotropic within the 90 days following the refill of an antidepressant. Psychotropic medications were classified as follows: antipsychotics (N05A), anxiolytics (N05B), sedatives (N05C), mood stabilisers (N03AF01, N03AG01, N03AX09, N05AN01), and anti-dementia drugs (N06D).
Outcome measures
The study outcomes were identified using the following ICD-10 codes: intentional self-harm (X60-X84), harm of undetermined intent (Y10-Y34), and sequelae of intentional self-harm and of events of undetermined intent (Y87.0 and Y87.2) from the Cause of Death Register (suicide) and from the National Patient Register (attempted suicide).
Covariates
Potential confounders included age at index date, sex, suicide attempt during the year preceding the index date, index antidepressant medication, and serious depression in the 3 months preceding or following the index date. Use of statins was used as a proxy of cardiovascular comorbidity since previous studies have shown associations between cardiovascular comorbidity, including cerebrovascular disease, and both depression [23] and suicide [24]. Nursing home residence during the year preceding the index date was used as a general marker of frailty, which may be associated with both depression [25] and suicide [26].
Statistical analysis
We used the Fine and Gray proportional hazard models [27] to estimate the sub-hazard ratios (SHRs) with 95% confidence intervals for the association between use patterns and suicide or suicide attempts. The Fine and Gray model is a time-to-event model, similar to the Cox proportional hazard model. However, unlike Cox’s regression, the Fine and Gray model is developed for competing data and takes into account that participants may die of other causes than that of interest. Use patterns were included in the model as time-varying covariates and the models were adjusted for the potential confounders mentioned above. In addition, we conducted gender-stratified analyses. Due to partially missing data, 210 individuals were excluded from the regression analyses.
We also described the crude associations between the use patterns of antidepressants and baseline characteristics including index medication (Online Resource 2). In order to assess the robustness of our findings, we used the Cox proportional hazards models to estimate the hazard ratios for cause-specific risk. A 0.05 significance level was used. Data management and statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
The study was approved by the Regional Ethical Review Board in Gothenburg (no: 111-15) as well as security clearance by the register holders in accordance with national regulations.
Results
Table 1 describes the baseline characteristics of the study population. Almost two thirds of the new antidepressant users were women. The mean age was 83.4 years, and almost one fifth lived in nursing homes. Four out of one thousand new users had attempted suicide during the year preceding the initiation of the antidepressant therapy, and 4% had a serious depression according to the National Patient Register. Selective serotonin reuptake inhibitors were filled by almost two thirds of the new users. Concomitant treatment with at least one other psychotropic medication was present for over half of the study population. The median length of follow-up was 2.6 (interquartile range 1.2–4.6) years.
Overall, 90,681 persons (48.7%) died during follow-up. Suicide was the cause of death for 295 individuals (199 men and 96 women), corresponding to an incidence rate of 50 per 100,000 person-years for the total study population (106 per 100,000 person-years in men, and 25 per 100,000 person-years in women). Suicide methods are presented for men and women in Online Resource 3.
Table 2 shows that the adjusted SHR (aSHR) for suicide was doubled among individuals who switched to another antidepressant medication (aSHR 2.42, 95% confidence interval 1.65 to 3.55) compared to those who did not. Elevated aSHRs were observed in those who filled a concomitant prescription for anxiolytics (1.54, 1.20 to 1.96), hypnotics (2.20, 1.69 to 2.85), and antipsychotics (1.73, 1.19 to 2.51) compared to those with no fill for each group.
There were 654 suicide attempts during the follow-up period (300 men and 354 women), yielding an incidence rate of 117 per 100,000 person-years for the total study population (167 per 100,000 person-years in men and 94 per 100,000 person-years in women).
Table 3 shows that the risk of suicide attempt was almost doubled among those who switched to another antidepressant (1.76, 1.32 to 2.34). Elevated aSHRs were observed for those who concomitantly filled a prescription for anxiolytics (2.04, 1.73 to 2.40) and hypnotics (2.86, 2.38 to 3.43). The aSHR for suicide attempt was significantly lower among individuals who were prescribed anti-dementia drugs (0.40, 0.27 to 0.59) compared to those without such drugs. There was no significant association between refill adherence (MPR ≥ 80%) and suicidal behaviours in both adjusted and unadjusted analyses.
Similar results were obtained for the associations between the use patterns of antidepressants and suicide in the gender-stratified analyses (Online Resource 4). However, a decreased risk of suicide in those using anti-dementia drugs was observed in men only. For the outcome suicide attempt, an increased risk was found among women using mood stabilisers but not in men. Several associations were no longer significant, which could be related to the relatively small number of cases in the stratified analyses.
The results from the Cox regression were in accordance with the Fine and Gray regression and are presented in the Online Resource 5.
Discussion
In this national population-based cohort study of all new users of antidepressants aged 75 years and older, we found increased risk of both fatal and non-fatal suicidal behaviour among those who concomitantly used anxiolytics and hypnotics and among those who switched antidepressant medication within the first 6 months of treatment.
The study is based on national data with no exclusion criteria, minimising the risk of selection bias. Moreover, there is no recall bias as use patterns and potential confounders were register-based. While we adjusted our regression models for several known confounders, our study design did not allow investigating other factors, such as substance misuse and family history of psychiatric disorder or suicidal behaviour. Nor did we have details about the psychopathology that may have alerted physicians to the need for treatment at index. Therefore, indication biases are to be considered [28]. The decision to prescribe a particular antidepressant or other psychotropic medication, and at a certain dose to a specific patient, depends upon the clinical diagnosis, or the severity of depression and concomitant medical conditions, which may be itself associated with the occurrence of the suicidal behaviours.
We used the term serious depression to describe the cases identified through the National Patient Register since the common practice in Sweden is that milder forms of depression are treated within primary care and more serious cases are referred [29]. However, some serious depressions may be managed in primary care only and are therefore missed in the National Patient Register. Also, milder forms of depression are associated with suicidal behaviour in older adults [30, 31], and these cannot be captured with our study design as diagnostic data from primary care were lacking in national registers, nor can we distinguish between new users who initiated antidepressant treatment for the very first time and previous users who were off antidepressants during the year prior to index. Another consideration is that we could not account for variation in depression severity during follow-up. We must therefore consider the possibility of residual confounding. The absence of association between refill adherence and suicidal behaviour should be interpreted with caution. Non-users of antidepressants may have been classified as users if they filled a prescription but failed to ingest the medication. We should highlight that half of the study population used multidose dispensed medications (automatic refill) which creates an artificially regular drug-dispensing pattern and thereby a high refill adherence. The small number of suicides and suicide attempts made it unfeasible to analyse results for individual substances. We did not also account for the period of increased risks to suicidal behaviours following the switch to another antidepressant, or for possible time trends in the associations between use pattern and suicidal behaviours. Further, we could not conduct stratified analyses by age groups, which is a limitation as factors related to suicidal behaviour in extreme old age may differ from those for persons in their mid-70s and 80s [32]. Our gender-stratified analyses should also be interpreted with caution due to the low number of suicides in women and therefore low power. By restricting the study to new users, in line with guidelines such as the GRACE guidelines [33], confounding can be limited yet it may limit the generalisability of our findings to all users of antidepressants. Excluding prevalent users may not allow evaluation of risks related to chronic exposure to antidepressants. However, the relatively long follow-up period means that some persons can be considered long-term users.
Results from this large prospective study expand on our previous findings pointing to increased risk of suicidal behaviour in older adults who used sedatives and hypnotics [15]. One possible explanation for the observed risk increase may be that these drugs trigger an aggressive behaviour [34]. It is also possible that concomitant use of anxiolytics and hypnotics is merely a marker for some other factors related to suicide risk or self-harm, for example, more complex psychopathology [35, 36]. In previous population-based studies in which older adults took part in psychiatric examinations, we have shown that anxiety symptoms [37], as well as sleep problems [32], may be independent predictors of suicidality. Furthermore, as older adults of today are less likely to abstain from alcohol compared to earlier born cohorts [38], possible interactions between these medications and alcohol cannot be outruled. Alcohol use may intensify impulsive tendencies, thereby increasing risk of suicidal behaviour.
Our finding of elevated SHRs of suicide and suicide attempt associated with switching antidepressants may in part be explained by the fact that drug cessation can in some cases result in withdrawal symptoms and relapse or exacerbation of the depression [39]. We cannot rule out confounding by indication, and switching may in many cases be perceived as a marker of treatment-resistant depression [40]. Moreover, patients with severe depression may transiently become agitated and restless and harm themselves (with or without fatal outcome), before the new antidepressant starts to relieve depression.
Confounding by indication may also help to explain the higher risk of suicide among those taking antipsychotics, as older adults with psychotic depression may be at particular risk of suicidal behaviour. Another factor to be taken into account is that the elevated risk could be in part related to akathisia [41, 42]. Older patients are more prone to drug-induced movement disorders, but they may lack the vocabulary to describe this adverse event. The lower rates of suicide attempts among new users of antidepressants concomitantly taking anti-dementia drugs is also likely to be explained, at least in part, by confounding by indication. Antidepressants are often prescribed well into the course of dementia also for other conditions such as psychomotor agitation. Clinical studies indicate that cognition may be compromised in non-demented older adults with suicidal behaviour [43], and it is possible that anti-dementia treatment might have a preventive effect for suicidal behaviour for some individuals facing issues of milder cognitive impairment. One Danish cohort study that included also younger patients demonstrated increased risk for suicide when a first diagnosis of dementia was made in hospital [44]. However, the patients in that study most likely represented a high-risk subgroup. A previous population register-based study reported a lower risk of suicide among women who discontinued their antidepressant treatment, but the age range of the study population was broad, including persons aged 50 and above [45]. As prescribing patterns are different among older age groups with lower life expectancy [46], it may not be relevant to compare the findings of our study with those conducted among younger adult populations.
The rate of suicide in our population is more than twofold that observed in the general population aged 75 years and above [47]. Our findings may help to inform the prescribers who initiate antidepressant treatment in their older adult patients. Inconsistent results regarding the associations between the use of antipsychotics and fatal and non-fatal suicidal behaviours indicate a need for further research to draw more definite conclusions about these associations. The same applies to the findings regarding anti-dementia drugs. Future research should consider indication biases and the clinical characteristics of patients initiating antidepressant therapy. The latter includes severity of depression symptoms as well as anxiety, cognitive dysfunction, and overall frailty. Studies need to be carried out in other settings as availability of healthcare, prescription patterns, and rates of both fatal and non-fatal suicidal behaviour vary widely in a global perspective.
Contribution of authors
KH conceived and designed the study, helped acquire the data, helped with data analysis and interpretation of results, drafted the article, and had the final approval. KAS conceived and designed the study, helped acquire the data, helped with data analysis, revised the article for content, and gave the final approval for publication. AH helped with data analysis and gave the final approval for publication. IS helped with interpretation of results, revised the manuscript, and gave the final approval for publication. SG performed data analysis, helped with interpretation of results, and gave the final approval for publication. MW is the primary investigator of the project. She conceived and designed the study, helped acquire the data, helped with interpretation of results, revised the article for content, and gave the final approval for publication. All authors had full access to all of the data (including statistical reports and tables) and can take responsibility for the integrity of the data and the accuracy of the data analysis. KH is the guarantor.
References
Statistics Sweden (2016) Statistics on Causes of Death 2015 [In Swedish]. http://www.socialstyrelsen.se/publikationer2016/2016-8-4. Accessed 17 Aug 2017
Bertolote JM, De Leo D (2012) Global suicide mortality rates—a light at the end of the tunnel? Crisis 33(5):249–253
Beautrais AL (2002) A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav 32(1):1–9
Barbui C, Esposito E, Cipriani A (2009) Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. Can Med Assoc J 180(3):291–297
Gibbons RD, Hur K, Bhaumik DK, Mann JJ (2005) The relationship between antidepressant medication use and rate of suicide. Arch Gen Psychiatry 62(2):165–172
Parikh C (2000) Antidepressants in the elderly: challenges for study design and their interpretation. Br J Clin Pharmacol 49(6):539–547
Cadieux RJ (1999) Antidepressant drug interactions in the elderly: understanding the P-450 system is half the battle in reducing risks. Postgrad Med 106(6):231–249
Reynolds CF III, Frank E, Kupfer DJ, Thase ME (1996) Treatment outcome in recurrent major depression: a post hoc comparison of elderly (“young old”) and midlife patients. Am J Psychiatry 153(10):1288
Lapierre S, Erlangsen A, Waern M, De Leo D, Oyama H, Scocco P, Gallo J, Szanto K, Conwell Y, Draper B (2011) A systematic review of elderly suicide prevention programs. Crisis 32(2):88–98
Conwell Y, Duberstein PR, Caine ED (2002) Risk factors for suicide in later life. Biol Psychiatry 52(3):193–204
Erlangsen A, Canudas-Romo V, Conwell Y (2008) Increased use of antidepressants and decreasing suicide rates: a population-based study using Danish register data. J Epidemiol Community Health 62(5):448–454
Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J (2011) Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 343:d4551
Vaughn McCall W, Benca RM, Rosenquist PB, Riley MA, McCloud L, Newman JC, Case D, Rumble M, Krystal AD (2017) Hypnotic medications and suicide: risk, mechanisms, mitigation, and the FDA. Am J Psychiatry 174(1):18–25
Lodhi LM, Shah A (2004) Psychotropic prescriptions and elderly suicide rates. Med Sci Law 44(3):236–244
Carlsten A, Waern M (2009) Are sedatives and hypnotics associated with increased suicide risk of suicide in the elderly? BMC Geriatr 9:20
Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A (2009) The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 24(11):659–667
Ray WA (2003) Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol 158(9):915–920
Wettermark B, Hammar N, Michael Fored C, Leimanis A, Otterblad Olausson P, Bergman U, Persson I, Sundström A, Westerholm B, Rosén M (2007) The new Swedish Prescribed Drug Register—opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16(7):726–735
Swedish National Board of Health and Welfare (2016) The National Patient Register. http://www.socialstyrelsen.se/register/halsodataregister/patientregistret/inenglish. Accessed 17 Aug 2017
WHO Collaborating Centre for Drug Statistics Methodology (2012) Guidelines for ATC classification and DDD assignment 2013. Oslo
Lesén E, Petzold M, Andersson K, Carlsten A (2009) To what extent does the indicator “concurrent use of three or more psychotropic drugs” capture use of potentially inappropriate psychotropics among the elderly? Eur J Clin Pharmacol 65(6):635–642
Choudhry NK, Shrank WH, Levin RL, Lee JL, Jan SA, Brookhart MA, Solomon DH (2009) Measuring concurrent adherence to multiple related medications. Am J Manag Care 15(7):457–464
Nemeroff CB, Goldschmidt-Clermont PJ (2012) Heartache and heartbreak—the link between depression and cardiovascular disease. Nat Rev Cardiol 9(9):526–539
Erlangsen A, Stenager E, Conwell Y (2015) Physical diseases as predictors of suicide in older adults: a nationwide, register-based cohort study. Soc Psychiatry Psychiatr Epidemiol 50(9):1427–1439
Brown PJ, Roose SP, Fieo R, Liu X, Rantanen T, Sneed JR, Rutherford BR, Devanand D, Avlund K (2014) Frailty and depression in older adults: a high-risk clinical population. Am J Geriatr Psychiatry 22(11):1083–1095
Fässberg MM, Cheung G, Canetto SS, Erlangsen A, Lapierre S, Lindner R, Draper B, Gallo JJ, Wong C, Wu J (2016) A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment Health 20(2):166–194
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
Grimes DA, Schulz KF (2002) Bias and causal associations in observational research. Lancet 359(9302):248–252
National Board of Health and Welfare (2016). National guidelines for care of depression and anxiety disorders: support for control and management [In Swedish]. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/20405/2016-12-6.pdf. Accessed 22 Aug 2017
Waern M, Runeson BS, Allebeck P, Beskow J, Rubenowitz E, Skoog I, Wilhelmsson K (2002) Mental disorder in elderly suicides: a case-control study. Am J Psychiatry 159(3):450–455
Wiktorsson S, Runeson B, Skoog I, Östling S, Waern M (2010) Attempted suicide in the elderly: characteristics of suicide attempters 70 years and older and a general population comparison group. Am J Geriatr Psychiatry 18(1):57–67
Fässberg MM, Östling S, Börjesson-Hanson A, Skoog I, Wærn M (2013) Suicidal feelings in the twilight of life: a cross-sectional population-based study of 97-year-olds. BMJ Open 3(2):e002260
Cox E, Martin BC, Van Staa T, Garbe E, Siebert U, Johnson ML (2009) Good research practices for comparative effectiveness research: approaches to mitigate bias and confounding in the design of nonrandomized studies of treatment effects using secondary data sources: the International Society for Pharmacoeconomics and Outcomes Research Good Research Practices for Retrospective Database Analysis Task Force Report—Part II. Value Health 12(8):1053–1061
Waern M (2003) Alcohol dependence and misuse in elderly suicides. Alcohol Alcohol 38(3):249–254
Gorman JM (1996) Comorbid depression and anxiety spectrum disorders. Depress Anxiety 4(4):160–168
Sherbourne CD, Wells KB (1997) Course of depression in patients with comorbid anxiety disorders. J Affect Disord 43(3):245–250
Jonson M, Skoog I, Marlow T, Fässberg MM, Waern M (2012) Anxiety symptoms and suicidal feelings in a population sample of 70-year-olds without dementia. Int Psychogeriatr 24(11):1865–1871
Waern M, Marlow T, Morin J, Östling S, Skoog I (2013) Secular changes in at-risk drinking in Sweden: birth cohort comparisons in 75-year-old men and women 1976–2006. Age Ageing 43(2):228–234
Keks N, Hope J, Keogh S (2016) Switching and stopping antidepressants. Aust Prescr 39(3):76–83
Philip NS, Carpenter LL, Tyrka AR, Price LH (2010) Pharmacologic approaches to treatment resistant depression: a re-examination for the modern era. Expert Opin Pharmacother 11(5):709–722
Miller CH, Fleischhacker WW (2000) Managing antipsychotic-induced acute and chronic akathisia. Drug Saf 22(1):73–81
Poyurovsky M (2010) Acute antipsychotic-induced akathisia revisited. Br J Psychiatry 196(2):89–91
Olsson P, Wiktorsson S, Sacuiu S, Marlow T, Östling S, Fässberg MM, Skoog I, Waern M (2016) Cognitive function in older suicide attempters and a population-based comparison group. J Geriatr Psychiatry 29(3):133–141
Erlangsen A, Zarit SH, Conwell Y (2008) Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am J Geriatr Psychiatry 16(3):220–228
Erlangsen A, Agerbo E, Hawton K, Conwell Y (2009) Early discontinuation of antidepressant treatment and suicide risk among persons aged 50 and over: a population-based register study. J Affect Disord 119(1):194–199
Hansen DG, Rosholm J-U, Gichangi A, Vach W (2007) Increased use of antidepressants at the end of life: population-based study among people aged 65 years and above. Age Ageing 36(4):449–454
National Board of Health and Welfare (2016). Statistical database for causes of death [In Swedish]. http://www.socialstyrelsen.se/statistik/statistikdatabas/dodsorsaker. Accessed 17 Oct 2017
Funding
MW received grants from the Swedish Research Council (VR) 2016-01590, the Swedish Research Council for Health, Working Life and Welfare (Forte) 2016-07097, Konung Gustaf V:s och Drottning Victorias Frimurarstiftelse, and ALFGBG-433511. KAS received a grant from the Söderström-König Foundation SLS-483251. IS received a grant from Forte 2013-2300.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare financial support from the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, Konung Gustaf V:s och Drottning Victorias Frimurarstiftelse, ALF, and the Söderström-König Foundation for the submitted work; there are no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years; there are no other relationships or activities that could appear to have influenced the submitted work. Karolina Andersson Sundell is employed by AstraZeneca. However, the views expressed in this study are her own and not those of AstraZeneca.
Ethical approval
This study was approved by the Regional Ethical Review Board in Gothenburg (no: 111-15).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hedna, K., Andersson Sundell, K., Hamidi, A. et al. Antidepressants and suicidal behaviour in late life: a prospective population-based study of use patterns in new users aged 75 and above. Eur J Clin Pharmacol 74, 201–208 (2018). https://doi.org/10.1007/s00228-017-2360-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2360-x