Abstract
Objective
The objective of this study was to perform a comparative assessment of tolerability of all licensed new antiepileptic drugs (AEDs) through a network meta-analysis (NMA) including all placebo-controlled double-blind clinical trials (RCTs) in all conditions in which these drugs have been tested.
Methods
NMA with a frequentist approach was used to compare proportions of patients withdrawing because of adverse events (AEs). Analyses were conducted for all therapeutic doses pooled and specifically for high therapeutic doses. Patients treated with non-therapeutic doses of each drug were excluded.
Results
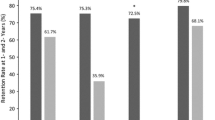
A total of 195 RCTs were included in the current analysis, comprising a total of 28,013 patients treated with AEDs and 17,908 patients treated with placebo. RCTs included in the analysis were 8 for brivaracetam; 5 for eslicarbazepine; 22 for gabapentin; 7 for lacosamide; 14 for levetiracetam; 14 for lamotrigine; 6 for oxcarbazepine; 9 for perampanel; 50 for pregabalin; 5 for tiagabine; 36 for topiramate; 7 for zonisamide; 4 for gabapentin-extended formulation (ER); 2 each for levetiracetam-ER, lamotrigine-ER, and topiramate-ER; and 1 each for oxcarbazepine-ER and pregabalin-ER. Brivaracetam, gabapentin, gabapentin-ER, and levetiracetam had a significantly lower withdrawal rate compared to several other AEDs, while eslicarbazepine, lacosamide, oxcarbazepine, and topiramate had a higher withdrawal rate. Perampanel, lamotrigine, pregabalin, tiagabine, and zonisamide showed an intermediate pattern of tolerability. Additional analysis has been conducted through selection of highly recommended doses for each drug. This analysis has roughly confirmed results of head to head comparisons of the all-dose analysis, with some exceptions. A further analysis has been conducted after exclusion of RCTs in which patients were allocated to the therapeutic dose of the experimental drug without titration, and it failed to show clinically important differences.
Significance
Relevant differences in short-term tolerability of AEDs have been observed between AEDs. Brivaracetam, gabapentin, and levetiracetam show the best tolerability profile while other AEDs are at higher risk for intolerable adverse effects.



Similar content being viewed by others
References
Perucca E, Tomson T (2011) The pharmacological treatment of epilepsy in adults. Lancet Neurol 10:446–456
Santulli L, Coppola A, Balestrini S et al (2016) The challenges of treating epilepsy with 25 antiepileptic drugs. Pharmacol Res 107:211–219
Zaccara G (2009) Neurological comorbidity and epilepsy: implications for treatment. Acta Neurol Scand 120:1–15
Lu G, Ades AE (2004) Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 23:3105–3124
Salanti G, Higgins JP, Ades AE et al (2008) Evaluation of networks of randomized trials. Stat Methods Med Res 17:279–301
Costa J, Fareleira F, Ascenção R et al (2011) Clinical comparability of the new antiepileptic drugs in refractory partial epilepsy: a systematic review and meta-analysis. Epilepsia 52:1280–1291
Bodalia PN, Grosso AM, Sofat R et al (2013) Comparative efficacy and tolerability of antiepileptic drugs for refractory focal epilepsy systematic review and network meta-analysis reveals the need for long-term comparator trials. Br J Clin Pharmacol 76:649–667
Rheims S, Perucca E, Ryvlin P (2011) Clinical comparability of the new antiepileptic drugs in refractory partial epilepsy: reply to Costa et al. Epilepsia 52:2139–2141
Zaccara G, Sisodiya SM, Giovannelli F et al (2013) Network meta-analysis and the comparison of efficacy and tolerability of anti-epileptic drugs for treatment of refractory focal epilepsy. Br J Clin Pharmacol 76:827–828
Zaccara G, Giovannelli F, Bell GS et al (2014) Network meta-analyses of antiepileptic drug efficacy and tolerability in drug-resistant focal epilepsies: a clinical perspective. Eur J Clin Pharmacol 70:647–654
Rheims S, Perucca E, Cucherat M et al (2011) Factors determining response to antiepileptic drugs in randomized controlled trials. A systematic review and meta-analysis. Epilepsia 52:219–233
Zaccara G, Giovannelli F, Cincotta M et al (2015) Adverse events of placebo-treated, drug-resistant, focal epileptic patients in randomized controlled trials: a systematic review. J Neurol 262:501–515
Higgins JPT, Altman DG. (2008) Chapter 8: assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions version 5.0.1 [updatedSeptember 2008]. Available atwebsite: http://www.cochrane-handbook.org/. Accessed October 2015
Cope S, Zhang J, Saletan S et al (2014) A process for assessing the feasibility of a network meta-analysis: a case study of everolimus in combination with hormonal therapy versus chemotherapy for advanced breast cancer. BMC Med 12:93
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:]
Biondi-Zoccai G (ed) (2014) Network meta-analysis: evidence synthesis with mixed treatment comparison. Nova Science Publishers, Hauppauge, NY
Rücker G (2012) Network meta-analysis, electrical networks and graph theory. Res Synth Methods 3:312–324
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
http://www.ema.europa.eu/docs/en_GB/document_library/Presentation/2012/05/WC500127919.pdf
Guekht AB, Korczyn AD, Bondareva IB et al (2010) Placebo responses in randomized trials of antiepileptic drugs. Epilepsy Behav 17:64–69
Zaccara G, Gangemi P, Perucca P et al (2011) The adverse event profile of pregabalin: a systematic review and meta-analysis of randomized controlled trials. Epilepsia 52:826–836
Zaccara G, Perucca P, Loiacono G et al (2013) The adverse event profile of lacosamide: a systematic review and meta-analysis of randomized controlled trials. Epilepsia 54:66–74
Zaccara G, Cincotta M, Borgheresi A et al (2004) Adverse motor effects induced by antiepileptic drugs. Epileptic Disord 6:153–168
Perucca P, Gilliam FG (2012) Adverse effects of antiepileptic drugs. Lancet Neurol 11:792–802
Verrotti A, Prezioso G, Di Sabatino F et al (2015) The adverse event profile of levetiracetam: a meta-analysis on children and adults. Seizure 31:49–55
Biton V, Gil-Nagel A, Brodie MJ et al (2013) Safety and tolerability of different titration rates of retigabine (ezogabine) in patients with partial-onset seizures. Epilepsy Res 107:138–145
Mula M, Hesdorffer DC, Trimble M et al (2009) The role of titration schedule of topiramate for the development of depression in patients with epilepsy. Epilepsia 50:1072–1076
Perucca E, Kwan P (2005) Overtreatment in epilepsy: how it occurs and how it can be avoided. CNS Drugs 19:897–908
Zaccara G, Giovannelli F, Giorgi FS et al (2016) Analysis of nocebo effects of antiepileptic drugs across different conditions. J Neurol 263:1274–1279
Zaccara G, Perucca P, Gangemi PF (2012) The adverse event profile of pregabalin across different disorders: a meta-analysis. Eur J Clin Pharmacol 68:903–912
Sake JK, Hebert D, Isojärvi J et al (2010) A pooled analysis of lacosamide clinical trial data grouped by mechanism of action of concomitant antiepileptic drugs. CNS Drugs 24:1055–1068
Contributions of authors
GZ proposed the project, wrote the protocol, carried out the review, and wrote the article. FG and UB made all analyses. VF performed literature search. GZ, FG, FSG, VF, and SG extracted data for a subset of included articles, cross-checked the results, and assessed eligibility and risk of bias. All authors commented on or edited sections of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Disclosure
GZ has received speaker’s or consultancy fees from EISAI, Jansen-Cilag, Sanofi-Aventis, and UCB Pharma. FG, FSG, and SG report no disclosures. VF is a former employee of Eisai s.r.l., Italy.
Funding
The authors received no funding for this study.
Electronic supplementary material
Additional Supporting Information may be found in the online version of this article:
ESM 1
PRISMA checklist (DOCX 19 kb)
ESM 2
Inclusion and exclusion criteria and therapeutic doses included in the analysis for each AED (DOCX 21 kb)
ESM 3
Flow charts and references of the identified studies (DOC 195 kb)
ESM 4
Main features of the 196 RCTs included in the analysis (XLS 75 kb)
ESM 5
Diseases explored and main conditions in which they were grouped (DOC 30 kb)
ESM 6
Risk of bias of the included studies (DOCX 23 kb)
ESM 7
Results of main findings (PPTX 133 kb)
ESM 8
Results of secondary analyses (PPTX 390 kb)
Rights and permissions
About this article
Cite this article
Zaccara, G., Giovannelli, F., Giorgi, F.S. et al. Tolerability of new antiepileptic drugs: a network meta-analysis. Eur J Clin Pharmacol 73, 811–817 (2017). https://doi.org/10.1007/s00228-017-2245-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2245-z