Abstract
Purpose
To describe the clinical profile of the patients that initiate statin therapy for the primary prevention of vascular diseases and to investigate the extent to which clinicians use intensive vs. standard regimens.
Methods
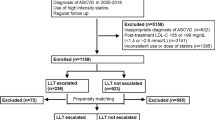
A cross-sectional analysis of nationwide individual data regarding individuals ≥11 years with a first prescription of statin, recorded between 1 January 2007 and 31 December 2011. Subjects were defined as intensive therapy initiators if a statin dose superior to simvastatin 40 mg (or equivalent dose if different statin) was first prescribed. Multivariable logistic regression models were built for dependent summary variables to evaluate the strength of the association between them and the use of intensive therapy.
Results
Overall, 69,737 patients receiving a first prescription of statin for the primary prevention of vascular diseases were identified. Predictors for intensive therapy initiation were male gender (adjusted OR: 1.28; 95%CI: 1.10–1.48), history of hypothyroidism (1.47; 1.17–1.85), current treatment of diabetes (1.18; 1.00–1.41), proteinuria (1.87; 1.12–3.12), age, and year of statin prescription. Modifiable risk factors associated with intensive therapy were elevated tryglicerides (1.63; 1.39–1.91), elevated LDL-C (1.96; 1.69–2.28), obesity (1.25; 1.07–1.47), smoking (1.32; 1.14–1.55), comedication with ezetimibe (3.76; 1.87–7.55), fibrates (1.96; 1.43–2.70) and calcium antagonists in women (1.42; 1.02–1.98).
Conclusions
The use of intensive therapy with statins in primary prevention was not very high in absolute terms, but is increasing considerably. The association between intensive therapy and previous hypothyroidism or its combination with fibrates may raise additional safety and tolerability concerns.

Similar content being viewed by others
References
Clark LT (2003) Treating dyslipidemia with statins: the risk-benefit profile. Am Heart J 145(3):387–396
Scandinavian Simvastatin Group (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344(8934):1383–1389
Naci H, Brugts JJ, Fleurence R, Tsoi B, Toor H, Ades A (2013) Comparative benefits of statins in the primary and secondary prevention of major coronary events and all-cause mortality: a network meta-analysis of placebo-controlled and active-comparator trials. Eur J Prev Cardiol 20(4):641–657
Cholesterol Treatment Trialists’ (CTT), Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380(9841):581–590
Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, Ward K, Ebrahim S (2013) Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 31:1
Lazar LD, Pletcher MJ, Coxson PG, Bibbins-Domingo K, Goldman L (2011) Cost-effectiveness of statin therapy for primary prevention in a low-cost statin era. Circulation 124(2):146–153
Catalá-López F, Sanfélix-Gimeno G, Ridao M, Peiró S (2013) When are statins cost-effective in cardiovascular prevention? A systematic review of sponsorship bias and conclusions in economic evaluations of statins. PLoS One 8(7):e69462. doi:10.1371/journal.pone.0069462
Agencia Española de Medicamentos y Productos Sanitarios. Proyecto BIFAP http://www.bifap.org/summary.php. Accessed July 2013
de Abajo FJ, Gil MJ, Bryant V, Timoner J, Oliva B, García-Rodríguez LA (2013) Upper gastrointestinal bleeding associated with NSAIDs, other drugs and interactions: a nested case–control study in a new general practice database. Eur J Clin Pharmacol 69(3):691–701
Hernández-Díaz S, García Rodríguez LA (2006) Cardioprotective aspirin users and their excess risk of upper gastrointestinal complications. BMC Med 4:22
National Institute for Health and Clinical Excellence. Lipid modification. Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. NICE Clinical guideline 67. London: NICE, May 2008. Available from: http://www.nice.org.uk/nicemedia/pdf/CG67NICEguideline.pdf Accessed July 2013
SIGN (Scottish Intercollegiate Guidelines Network). Risk estimation and the prevention of cardiovascular disease. Guideline No 97. ISBN 1899893997 Edinburgh: SIGN, 2007. Available on: http://www.sign.ac.uk/pdf/sign97.pdf. Accessed July 2013
Maiques Galán A, Brotons Cuixart C, Villar Álvarez F, Navarro Pérez J, Lobos-Bejarano JM, Ortega Sánchez-Pinilla R, Martín Rioboó R, Banegas Banegas JR, Orozco-Beltrán D, Gil Guillén V (2012) Preventive cardiovascular recommendations. Aten Primaria 44(Supl 1):3–15
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
Fifth Joint Task Force of the European Society of Cardiology; European Association of Echocardiography; European Association of Percutaneous Cardiovascular Interventions; European Heart Rhythm Association; Heart Failure Association; European Association for Cardiovascular Prevention & Rehabilitation; European Atherosclerosis Society; International Society of Behavioural Medicine; European Stroke Organisation; European Society of Hypertension; European Association for the Study of Diabetes; European Society of General Practice/Family Medicine; International Diabetes Federation Europe; European Heart Network (2012) European guidelines on cardiovascular disease prevention in clinical practice (version 2012): the fifth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Prev Cardiol 19(4):585–667
Miller M, Stone NJ, Ballantyne C, Bittner V, Criqui MH, Ginsberg HN, Goldberg AC, Howard WJ, Jacobson MS, Kris-Etherton PM, Lennie TA, Levi M, Mazzone T, Pennathur S (2011) Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association 123(20):2292–2333
Cholesterol Treatment Trialists’ (CTT), Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, Collins R (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376(9753):1670–1681
Martin K, Bégaud B, Latry P, Miremont-Salamé G, Fourrier A, Moore N (2004) Differences between clinical trials and postmarketing use. Br J Clin Pharmacol 57(1):86–92
Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, Hill KA, Pfeffer MA, Skene AM (2004) Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med 350(15):1495–1504
Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine (SEARCH), Armitage J, Bowman L, Wallendszus K, Bulbulia R, Rahimi K, Haynes R, Parish S, Peto R, Collins R (2010) Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: a double-blind randomised trial. Lancet 376(9753):1658–1669
De Lemos JA, Blazing MA, Wiviott SD, Lewis EF, Fox KA, White HD, Rouleau JL, Pedersen TR, Gardner LH, Mukherjee R, Ramsey KE, Palmisano J, Bilheimer DW, Pfeffer MA, Califf RM, Braunwald E (2004) Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA 292(11):1307–1316
Pedersen TR, Faergeman O, Kastelein JJ, Olsson AG, Tikkanen MJ, Holme I, Larsen ML, Bendiksen FS, Lindahl C, Szarek M, Tsai J (2005) High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 294(19):2437–2445
Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, Sillesen H, Simunovic L, Szarek M, Welch KM, Zivin JA (2006) High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 355:549–559
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ (2008) Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med 359(21):2195–2207
Crouse JR 3rd, Raichlen JS, Riley WA, Evans GW, Palmer MK, O’Leary DH, Grobbee DE, Bots ML, METEOR Study Group (2007) Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: the METEOR TRIAL. JAMA 297(12):1344–1353
Ito MK (2012) Dyslipidemia: management using optimal lipid-lowering therapy. Ann Pharmacother 46(10):1368–1381
Ridker PM, Genest J, Boekholdt SM, Libby P, Gotto AM, Nordestgaard BG, Mora S, MacFadyen JG, Glynn RJ, Kastelein JJ (2010) HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: an analysis from the JUPITER trial. Lancet 376(9738):333–339
Preiss D, Tikkanen MJ, Welsh P, Ford I, Lovato LC, Elam MB, LaRosa JC, DeMicco DA, Colhoun HM, Goldenberg I, Murphy MJ, MacDonald TM, Pedersen TR, Keech AC, Ridker PM, Kjekshus J, Sattar N, McMurray JJ (2012) Lipid-modifying therapies and risk of pancreatitis: a meta-analysis. JAMA 308(8):804–811
Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Thomason MJ, Mackness MI, Charlton-Menys V, Fuller JH (2004) Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study. Lancet 364:685–896
Duntas LH, Brenta G (2012) The effect of thyroid disorders on lipid levels and metabolism. Med Clin North Am 96(2):269–281
Bruckert E, Hayem G, Dejager S, Yau C, Bégaud B (2005) Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients-the PRIMO study. Cardiovasc Drugs Ther 19(6):403–414
Food and Drugs Administration (FDA). CRESTOR (AstraZeneca Pharmaceuticals LP) Label. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021366Orig1s024Lbl.pdf Accessed July 2013
Dormuth CR, Hemmelgarn BR, Paterson JM, James MT, Teare GF, Raymond CB, Lafrance JP, Levy A, Garg AX, Ernst P (2013) Use of high potency statins and rates of admission for acute kidney injury: multicenter, retrospective observational analysis of administrative databases. BMJ 346:f880. doi:10.1136/bmj.f880
Kostapanos MS, Milionis HJ, Elisaf MS (2010) Rosuvastatin-associated adverse effects and drug-drug interactions in the clinical setting of dyslipidemia. Am J Cardiovasc Drugs 10(1):11–28
Pearson TA, Laurora I, Chu H, Kafonek S (2000) The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med 160(4):459–467
Desai DA, Zakaria S, Ouyang P (2012) Initiation of statin therapy: are there age limits? Curr Atheroscler Rep 14(1):17–25
Savoie I, Kazanjian A (2002) Utilization of lipid-lowering drugs in men and women a reflection of the research evidence? J Clin Epidemiol 55(1):95–101
Food and Drugs Administration (FDA). VYTORIN® (Merck&Co Inc) Label. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021687s044lbl.pdf Accessed July 2013
Amend KL, Landon J, Thyagarajan V, Niemcryk S, McAfee A (2011) Incidence of hospitalized rhabdomyolysis with statin and fibrate use in an insured US population. Ann Pharmacother 45(10):1230–1239
Davidson MH, Armani A, McKenney JM, Jacobson TA (2007) Safety considerations with fibrate therapy. Am J Cardiol 99(6A):3C–18C
Acknowledgments
Authors would like to acknowledge the excellent collaboration of general practitioners taking part in BIFAP.
Funding
None.
Conflict of Interest Statement
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work and no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Contributions of Authors statement
All the authors have contributed substantially to the material and/or intellectual content, data analysis, if applicable, and the writing of the manuscript, sufficiently to accept public accountability for it.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Macías Saint-Gerons, D., de la Fuente Honrubia, C., Montero Corominas, D. et al. Standard and intensive lipid-lowering therapy with statins for the primary prevention of vascular diseases: a population-based study. Eur J Clin Pharmacol 70, 99–108 (2014). https://doi.org/10.1007/s00228-013-1586-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-013-1586-5