Abstract
Purpose
Our aim was to compare pharmacological aspects of two switching strategies from morphine/oxycodone to methadone; the stop and go (SAG) strategy in which methadone is started directly after the initial opioid has been stopped, and the 3-days switch (3DS), in which morphine/oxycodone is gradually changed to methadone by cross-tapering over 3 days.
Methods
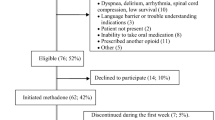
Forty-two cancer patients with pain and/or opioid side effects were assessed in this randomised trial. Trough serum concentrations of methadone, morphine, morphine-6-glucuronide (M6G), and oxycodone were measured on days 1, 2, 3, 4, 7, and 14. Primary outcome was number of patients with methadone concentrations in apparent CSS on day 4. Secondary outcomes were exposure to opioids during the first 3 days, interindividual variation of opioid concentrations, and correlation between methadone concentrations and pain intensity (PI) day 3.
Results
Thirty-five patients received methadone (16 in the SAG group, 19 in the 3DS group). The median preswitch morphine equivalent doses were 620 (range 350–2000) mg/day in the SAG group and 800 (range 90–3600) mg/day in the 3DS group (p = 0.43);42% reached CSS for methadone in the SAG group on day 4 compared with 22% in the 3DS group (p = 0.42). The SAG group was significantly less exposed to morphine/M6G/oxycodone and significantly more exposed to methadone in the first 3 days. Methadone showed a low correlation with PI. More patients dropped out after intervention in the SAG group than in the 3DS group (38% vs. 5%; p = 0.032). One SAG patient suffered from respiratory depression on day 5.
Conclusion
The SAG group was initially more exposed to methadone and less to the replaced opioids but without observed clinical benefit and with a higher dropout rate. Patients switched to methadone should be followed closely for the first 5 days, regardless of switching strategy.




Similar content being viewed by others
References
Hanks GW, de Conno F, Cherny N, Hanna M, Kalso E, McQuay HJ, Mercadante S, Meynadier J, Poulain P, Ripamonti C, Radbruch L, Casas JRI, Sawe J, Twycross RG, Ventafridda V (2001) Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer 84(5):587–593
Totah RA, Sheffels P, Roberts T, Whittington D, Thummel K, Kharasch ED (2008) Role of CYP2B6 in stereoselective human methadone metabolism. Anesthesiology 108(3):363–374. doi:10.1097/ALN.0b013e3181642938
Kharasch ED, Hoffer C, Whittington D, Walker A, Bedynek PS (2009) Methadone pharmacokinetics are independent of cytochrome P4503A (CYP3A) activity and gastrointestinal drug transport: insights from methadone interactions with ritonavir/indinavir. Anesthesiology 110(3):660–672. doi:10.1097/ALN.0b013e3181986a9a
Shinderman M, Maxwell S, Brawand-Amey M, Golay KP, Baumann P, Eap CB (2003) Cytochrome P4503A4 metabolic activity, methadone blood concentrations, and methadone doses. Drug Alcohol Depend 69(2):205–211
Gronlund J, Saari TI, Hagelberg NM, Neuvonen PJ, Olkkola KT, Laine K (2010) Exposure to oral oxycodone is increased by concomitant inhibition of CYP2D6 and 3A4 pathways, but not by inhibition of CYP2D6 alone. Br J Clin Pharmacol 70(1):78–87. doi:10.1111/j.1365-2125.2010.03653.x
Coffman BL, Rios GR, King CD, Tephly TR (1997) Human UGT2B7 catalyzes morphine glucuronidation. Drug Metab Dispos 25(1):1–4
Nicholson AB (2004) Methadone for cancer pain. Cochrane Database Syst Rev (2): CD003971 doi:10.1002/14651858.CD003971.pub2 [doi]
Mercadante S, Casuccio A, Calderone L (1999) Rapid switching from morphine to methadone in cancer patients with poor response to morphine. J Clin Oncol 17(10):3307–3312
Mercadante S, Bianchi M, Villari P, Ferrera P, Casuccio A, Fulfaro F, Gebbia V (2003) Opioid plasma concentration during switching from morphine to methadone: Preliminary data. Support Care Cancer 11(5):326–331
Benitez-Rosario MA, Salinas-Martin A, guirre-Jaime A, Perez-Mendez L, Feria M (2009) Morphine-methadone opioid rotation in cancer patients: analysis of dose ratio predicting factors. J Pain Symptom Manage 37(6):1061–1068
Ripamonti C, Groff L, Brunelli C, Polastri D, Stavrakis A, De Conno F (1998) Switching from morphine to oral methadone in treating cancer pain: what is the equianalgesic dose ratio? J Clin Oncol 16(10):3216–3221
Lawlor PG, Turner KS, Hanson J, Bruera ED (1998) Dose ratio between morphine and methadone in patients with cancer pain: a retrospective study. Cancer 82(6):1167–1173
Bruera E, Pereira J, Watanabe S, Belzile M, Kuehn N, Hanson J (1996) Opioid rotation in patients with cancer pain. A retrospective comparison of dose ratios between methadone, hydromorphone, and morphine. Cancer 78(4):852–857. doi:10.1002/(SICI)1097-0142(19960815)78:4<852::AID-CNCR23>3.0.CO;2-T
Fredheim OM, Kaasa S, Dale O, Klepstad P, Landro NI, Borchgrevink PC (2006) Opioid switching from oral slow release morphine to oral methadone may improve pain control in chronic non-malignant pain: a nine-month follow-up study. PalliatMed 20(1):35–41
Ripamonti C, De Conno F, Groff L, Belzile M, Pereira J, Hanson J, Bruera E (1998) Equianalgesic dose/ratio between methadone and other opioid agonists in cancer pain: comparison of two clinical experiences. Ann Oncol 9(1):79–83
Dale O, Moksnes K, Kaasa S (2011) European Palliative Care Research Collaborative pain guidelines: Opioid switching to improve analgesia or reduce side effects. A systematic review Palliat Med 25(5):494–503. doi:10.1177/0269216310384902
Fredheim OM, Borchgrevink PC, Klepstad P, Kaasa S, Dale O (2007) Long term methadone for chronic pain: a pilot study of pharmacokinetic aspects. Eur J Pain 11(6):599–604
Auret K, Roger Goucke C, Ilett KF, Page-Sharp M, Boyd F, Oh TE (2006) Pharmacokinetics and pharmacodynamics of methadone enantiomers in hospice patients with cancer pain. Ther Drug Monit 28(3):359–366
Sawe J, Hansen J, Ginman C, Hartvig P, Jakobsson PA, Nilsson MI, Rane A, Anggard E (1981) Patient-controlled dose regimen of methadone for chronic cancer pain. Br Med J (Clin Res Ed) 282(6266):771–773
Moksnes K, Dale O, Rosland JH, Paulsen O, Klepstad P, Kaasa S (2011) How to switch from morphine or oxycodone to methadone in cancer patients? A randomised clinical phase II trial Eur J Cancer. doi:10.1016/j.ejca.2011.06.047
Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E (2001) Equianalgesic dose ratios for opioids. a critical review and proposals for long-term dosing. J Pain Symptom Manage 22(2):672–687
Ayonrinde OT, Bridge DT (2000) The rediscovery of methadone for cancer pain management. Med J Aust 173(10):536–540
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 23(2):129–138
Klepstad P, Loge JH, Borchgrevink PC, Mendoza TR, Cleeland CS, Kaasa S (2002) The Norwegian brief pain inventory questionnaire: translation and validation in cancer pain patients. JPain SymptomManage 24(5):517–525
Dale O, Piribauer M, Kaasa S, Moksnes K, Knobel H, Klepstad P (2009) A double-blind, randomised, crossover comparison between single-dose and double-dose immediate-release oral morphine at bedtime in cancer patients. J Pain Symptom Manage 37(1):68–76. doi:10.1016/j.jpainsymman.2007.12.016
Shah VP, Midha KK, Dighe S, McGilveray IJ, Skelly JP, Yacobi A, Layloff T, Viswanathan CT, Cook CE, McDowall RD, Pittman KA, Spector S (1992) Analytical Methods Validation - Bioavailability, Bioequivalence, and Pharmacokinetic Studies. J Pharm Sci 81(3):309–312
Dadgar D, Burnett PE, Choc MG, Gallicano K, Hooper JW (1995) Application issues in bioanalytical method validation, sample analysis and data reporting. J Pharm Biomed Anal 13(2):89–97
Edwards SR, Smith MT (2007) Low-level quantitation of oxycodone and its oxidative metabolites, noroxycodone, and oxymorphone, in rat plasma by high-performance liquid chromatography-electrospray ionization-tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 848(2):264–270. doi:10.1016/j.jchromb.2006.10.039
Katz R, Kelly HW (1993) Pharmacokinetics of continuous infusions of fentanyl in critically ill children. Crit Care Med 21(7):995–1000
Andreassen TN, Klepstad P, Davies A, Bjordal K, Lundstrom S, Kaasa S, Dale O (2011) Influences on the pharmacokinetics of oxycodone: a multicentre cross-sectional study in 439 adult cancer patients. Eur J Clin Pharmacol 67(5):493–506. doi:10.1007/s00228-010-0948-5
Eap CB, Bertschy G, Baumann P, Finkbeiner T, Gastpar M, Scherbaum N (1998) High interindividual variability of methadone enantiomer blood levels to dose ratios. Arch Gen Psychiatry 55(1):89–90
Lotsch J, Geisslinger G, Tegeder I (2009) Genetic modulation of the pharmacological treatment of pain. Pharmacol Ther 124(2):168–184. doi:10.1016/j.pharmthera.2009.06.010
Quigley C, Joel S, Patel N, Baksh A, Slevin M (2003) Plasma concentrations of morphine, morphine-6-glucuronide and morphine-3-glucuronide and their relationship with analgesia and side effects in patients with cancer-related pain. Palliat Med 17(2):185–190
Wolff T, Samuelsson H, Hedner T (1995) Morphine and morphine metabolite concentrations in cerebrospinal fluid and plasma in cancer pain patients after slow-release oral morphine administration. Pain 62(2):147–154
Klepstad P, Borchgrevink PC, Dale O, Zahlsen K, Aamo T, Fayers P, Fougner B, Kaasa S (2003) Routine drug monitoring of serum concentrations of morphine, morphine-3-glucuronide and morphine-6-glucuronide do not predict clinical observations in cancer patients. Palliat Med 17(8):679–687
Kristensen K, Christensen CB, Christrup LL (1995) The mu1, mu2, delta, kappa opioid receptor binding profiles of methadone stereoisomers and morphine. Life Sci 56(2):PL45–PL50
Hunt G, Bruera E (1995) Respiratory depression in a patient receiving oral methadone for cancer pain. JPain SymptomManage 10(5):401–404
Ettinger DS, Vitale PJ, Trump DL (1979) Important clinical pharmacologic considerations in the use of methadone in cancer patients. Cancer Treat Rep 63(3):457–459
Bond Sutton L, Erlen JA, Glad JM, Siminoff LA (2003) Recruiting vulnerable populations for research: revisiting the ethical issues. J Prof Nurs 19(2):106–112. doi:10.1053/jpnu.2003.16
Acknowledgements
We are grateful for the assistance from Gunnhild Jacobsen, Turid Nilsen, Trine Andreassen, and Kjell Aarstad for blood analyses, from Karin Tulluan for the randomisation process, and for valuable advice from Olav M.S. Fredheim and Line Oldervoll. We also thank the staff at the participating units and the patients for their participation. This study was supported by grants from the Norwegian Research Council and Norwegian Cancer Society.
Conflict of interest
The authors declare that they have no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Additional information
ClinicalTrials.gov id: NCT0014496
Rights and permissions
About this article
Cite this article
Moksnes, K., Kaasa, S., Paulsen, Ø. et al. Serum concentrations of opioids when comparing two switching strategies to methadone for cancer pain. Eur J Clin Pharmacol 68, 1147–1156 (2012). https://doi.org/10.1007/s00228-012-1228-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1228-3