Abstract
Purpose
Outpatient subcutaneous therapies are becoming increasingly common. A literature search failed to find produced any studies on application problems pertaining to the self-injection of low-molecular-weight heparins (LMWH) in a heterogeneous outpatient population under daily-life conditions. We therefore designed a study with the aim of recording drug use problems, patient satisfaction, compliance, problems arising from the injection site (abdomen vs. thigh), and residual drug volumes in pre-filled syringes used in self-injection therapy.
Methods
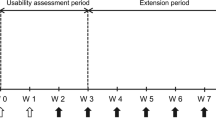
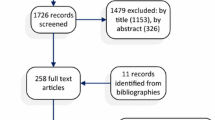
Patients were recruited in community pharmacies by 95 trained Master's students in pharmacy. Data were collected during recruitment and by means of structured questionnaire-based telephone interviews that were carried out at the beginning and the end of the LMWH treatment.
Results
The median age of the 213 patients enrolled in the study was 54 years [interquartile range (IQR) 39–70 years]; of these, 15.5% had their injections administered by a third person. The rate of self-reported non-compliance was 17.1%. At least one relevant problem was recorded in 85.0% of the cases. At the end of the treatment, 38.9% of the patients stated self-administration of the injections required some effort. The preferred injection site was the thigh (68.5%). An overall mean residual drug volume ≥10.0% was detected for 3.9% of the patients. If residual drug was present, a median of 11.2% (IQR 8.6–17.6%) of the total drug volume had not been injected. Patients injecting into the thigh showed a higher risk of leaving residual medication (odds ratio 2.16, 95% confidence interval 1.04–4.51).
Conclusions
Most patients had drug use problems, whereas no clear factors were associated with non-compliance, the injection site (apart from residual drug), and discomfort or effort required (apart from prior injection use).



Similar content being viewed by others
References
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW (2008) Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 133[Suppl]:381S–453S
Bates SM, Greer IA, Pabinger I, Sofaer S, Hirsh J (2008) Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 133[Suppl]:844S–886S
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G (2008) Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 133[Suppl 6]:160S–198S
Othieno R, Abu Affan M, Okpo E (2007) Home versus in-patient treatment for deep vein thrombosis. Cochrane Database Syst Rev (3):CD003076
Matsagas MI (2004) Outpatient treatment of venous thromboembolism using low molecular weight heparins. An overview. Int Angiol 23:305–316
Fahs PS, Kinney MR (1991) The abdomen, thigh, and arm as sites for subcutaneous sodium heparin injections. Nurs Res 40:204–207
Stäubli M, Suter J (2004) Die Komplikationenliste der Schweizerischen Gesellschaft für Innere Medizin. Schweiz Aerztezeitung 85:1109–1116
Huber AR (2005) Fragen aus der Praxis zum Thema Antikoagulation. Prim Care 5:773
Lemke H, Imhoff M, Lohlein D (1994) Increased wound healing disorders in patients with inguinal hernia caused by administration of antithrombotic agents in the abdominal wall. Chirurg 65:714–716
Donaldson J, Knowles CH, Clark SK, Renfrew I, Lobo MD (2007) Rectus sheath haematoma associated with low molecular weight heparin: a case series. Ann R Coll Surg Engl 89:309–312
Cuculi F, Gurzeler J (2006) What is your diagnosis? Rectus sheath hematoma. Praxis 95:11–12
Andereya S, Kalicke T, Hopf KF, Buschmeier M, Muhr G (2003) Serious complication after subcutaneous injection of heparin for prophylaxis of thromboembolism. Case report. Unfallchirurg 106:182–183
Pessina I, Bocchia M, Giansante P, Vaghi A (2003) Hematoma of the rectus muscle of abdomen in a patient treated with nadroparin. Recenti Prog Med 94:321–322
Luyx C, Vanpee D, Douala C, Gillet JB (2001) Acute dyspnea in a woman with swelling of the left leg treated with low molecular weight heparin. Am J Emerg Med 19:223–224
Morau D, Barthelet Y, Spilmann E, d'Athis F (2000) Hematoma of the right rectus abdominis in relation to treatment with low-molecular-weight heparin. Ann Fr Anesth Rèanim 19:69–70
Berna JD, Zuazu I, Madrigal M, Garcia-Medina V, Fernandez C, Guirado F (2000) Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging 25:230–234
Tsapatsaris NP (1991) Low-dose heparin. A cause of hematoma of rectus abdominis. Arch Intern Med 151:597–599
Webb KB, Hadzima S (1987) Hematoma of the rectus abdominis muscle: a complication of subcutaneous heparin therapy. South Med J 80:911–912
Zaybak A, Khorshid L (2008) A study on the effect of the duration of subcutaneous heparin injection on bruising and pain. J Clin Nurs 17:378–385
Chan H (2001) Effects of injection duration on site-pain intensity and bruising associated with subcutaneous heparin. J Adv Nurs 35:882–892
Spahn G (2002) Compliance with self-administration of heparin injections in outpatients. Eur J Trauma 28:104–109
Colwell CW, Pullido P, Hardwick ME, Morris BA (2005) Patient compliance with outpatient prophylaxis: an observational study. Orthopedics 28:143–147
Watts AC, Howie CR, Simpson AH (2006) Assessment of a self-administration protocol for extended subcutaneous thromboprophylaxis in lower limb arthroplasty. J Bone Joint Surg Br 88:107–110
Le Gall C, Jacques E, Medjebeur C, Darques L, Briand F, Haddad J, Bleichner G (2006) Low molecular weight heparin self-injection training: assessment of feasibility, tolerance and economic analysis in emergency departments. Eur J Emerg Med 13:264–269
Mengiardi S, Goepfert B, Tsakiris DA, Hersberger KE (2009) Pitfalls in patient self-management of subcutaneous drug application: removal of rubber protection caps from ready-to-use syringes. Eur J Clin Pharmacol 65:1061–1062
Jorgensen JT, Romsing J, Rasmussen M, Moller-Sonnergaard J, Vang L, Musaeus L (1996) Pain assessment of subcutaneous injections. Ann Pharmacother 30:729–732
da Silva AA, Cassiani SH, Optiz SP (2002) Evaluation of the technique of subcutaneous administration of heparin in the development of hematomas. Rev Bras Enferm 55:128–133
Lalezari JP, Patel IH, Zhang X, Dorr A, Hawker N, Siddique Z, Kolis SJ, Kinchelow T (2003) Influence of subcutaneous injection site on the steady-state pharmacokinetics of enfuvirtide (T-20) in HIV-1-infected patients. J Clin Virol 28:217–222
Frid A, Hardebo JE (1997) The thigh may not be suitable as an injection site for patients self-injecting sumatriptan. Neurology 49:559–561
Acknowledgments
We would like to thank the participating community pharmacies for their cooperation. We also thank the Master’s students for data collection, the patients for participating in the study, Michael Mittag for his support in the statistical analysis, and Irene Vogel Kahmann, Raphaela von Grünigen, Joëlle Bader, and Paul Lavender for their valuable contributions.
Conflict of interest
This study was supported by Pfizer AG through an unrestricted Investigator-Initiated Research Grant (IIRG).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mengiardi, S., Tsakiris, D.A., Lampert, M.L. et al. Drug use problems with self-injected low-molecular-weight heparins in primary care. Eur J Clin Pharmacol 67, 109–120 (2011). https://doi.org/10.1007/s00228-010-0956-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-010-0956-5