Abstract
Objective
To analyze prescriptions in a general-practitioner database over 1 year to determine the frequency, the characteristics, and the monitoring of the severe potential drug-drug interactions (DDIs).
Methods
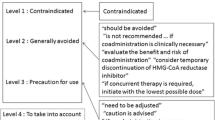
We retrospectively analyzed the clinical records from 16 general practitioners in the Veneto region, an area in northern Italy. The study covered the period from January 1 to December 31, 2004. We selected all severe and well-documented interactions according to the book Drug Interaction Facts by David S. Tatro (Facts and Comparisons, St. Louis, MO, 2006). We grouped severe potential DDIs according to their specific potential risk, and for the most frequently interacting drug pairs, we investigated whether some specific tests had been prescribed by physicians for safety monitoring.
Results
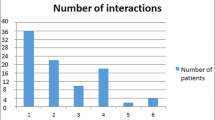
During the study period, 16,037 patients (55% female) with at least one drug prescription were recorded, and a total of 185,704 prescriptions relating to 1,020 different drugs were analyzed. Ramipril was the most frequently prescribed drug followed by acetylsalicylic acid and atorvastatin. The final number of different types of severe potential DDIs was 119, which occurred 1,037 times in 758 patients (4.7% of the total number of patients). More than 80% of drugs involved in severe potential DDIs were cardiovascular drugs. Digoxin was the most frequently involved drug. Electrolyte disturbances, increase in serum digoxin levels, risk of hemorrhage, severe myopathy or rhabdomyolysis, and cardiac arrhythmias were the most commonly implicated potential risks. When considering patients using digoxin with loop or thiazide diuretics for more than 5 months, 72% had at least one test to monitor potential digoxin toxicity, whereas 28% had no tests. Sixty-four percent of patients using digoxin with amiodarone, verapamil, or propafenone had an ECG and/or digoxin monitoring, and 36% of them did not have any tests.
Conclusions
The present study revealed that, in a group of Italian general practitioners, the risks of severe potential drug interactions are relatively low and the drugs concerned are few. Analyses of specific tests showed that physicians are generally aware of the potential risks caused by digoxin drug associations. However not all patients were closely monitored and this should be improved.


Similar content being viewed by others
References
Tatro DS (ed) (2006) Drug interaction facts™—the authority on drug interactions. Facts and Comparisons, St. Louis, MO
Grönroos PE, Irjala KM, Huupponen RK, Scheinin H, Forsström J, Forsström JJ (1997) A medication database-a tool for detecting drug interactions in hospital. Eur J Clin Pharmacol 53(1):13–17
Glintborg B, Andersen SE, Dalhoff K (2005) Drug-drug interactions among recently hospitalized patients-frequent but mostly clinically insignificant. Eur J Clin Pharmacol 61(9):675–681
Cruciol-Souza JM, Thomson JC (2006) Prevalence of potential drug-drug interactions and its associated factors in a Brazilian teaching hospital. J Pharm Pharm Sci 9(3):427–433
Bjerrum L, Andersen M, Petersen G, Kragstrup J (2003) Exposure to potential drug interactions in primary health care. Scand J Prim Health Care 21(3):153–158
Jankel CA, Speedie SM (1990) Detecting drug interactions: a review of the literature. DICP 24(10):982–989
Björkman IK, Fastbom J, Schmidt IK, Bernsten CB, Pharmaceutical Care of the Elderly in Europe Research (PEER) Group (2002) Drug-drug interactions in the elderly. Ann Pharmacother 36(11):1675–1681
Bergendal L, Friberg A, Schaffrath A (1995) Potential drug-drug interactions in 5,125 mostly elderly out-patients in Gothenburg, Sweden. Pharm World Sci 17(5):152–157
Costa AJ (1991) Potential drug interactions in an ambulatory geriatric population. Fam Pract 8(3):234–236
Rosholm JU, Bjerrum L, Hallas J, Worm J, Gram LF (1998) Polypharmacy and the risk of drug-drug interactions among Danish elderly. A prescription database study. Dan Med Bull 45(2):210–213
Guèdon-Moreau L, Ducrocq D, Duc MF, Quieureux Y, L’Hôte C, Deligne J, Caron J (2004) Absolute contraindications in relation to potential drug interactions in outpatient prescriptions: analysis of the first five million prescriptions in 1999. Eur J Clin Pharmacol 59(12):899–904
Astrand B, Astrand E, Antonov K, Petersson G (2006) Detections of potential drug interactions-a model for a national pharmacy register. Eur J Clin Pharmacol 62(9):749–756
Steiness E, Olesen KH (1976) Cardiac arrhythmias induced by hypokalaemia and potassium loss during maintenance digoxin therapy. Br Heart J 38(2):167–172
Schepkens H, Vanholder R, Billiouw JM, Lameire N (2001) Life-threatening hyperkalemia during combined therapy with angiotensin-converting enzyme inhibitors and spironolactone: an analysis of 25 cases. Am J Med 110(6):438–441
Janchawee B, Owatranporn T, Mahatthanatrakul W, Chongsuvivatwong V (2005) Clinical drug interactions in outpatients of a university hospital in Thailand. J Clin Pharm Ther 30(6):583–590
Egger SS, Drewe J, Schlienger RG (2003) Potential drug-drug interactions in the medication of medical patients at hospital discharge. Eur J Clin Pharmacol 58(11):773–778
Becker ML, Kallewaard M, Caspers PW, Visser LE, Leufkens HG, Stricker BH (2006) Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf 16(6):641–651
Doucet J, Chassagne P, Trivalle C, Landrin I, Pauty MD, Kadri N, Mènard JF, Bercoff E (1996) Drug-drug interactions related to hospital admissions in older adults: a prospective study of 1000 patients. J Am Geriatr Soc 44(8):944–948
McDonnell PJ, Jacobs MR (2002) Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 36(9):1331–1336
Vitry AI (2006) Comparative assessment of four drug interaction compendia. Br J Clin Pharmacol 63(6):709–714
Il Pensiero Scientifico (Ed) (2005) L’uso dei Farmaci in Italia-Rapporto Nazionale anno 2004. OsMed (Osservatorio Nazionale sull’Impiego dei Medicinali), Rome
Fux R, Greiner D, Geldmacher M, Mörike K, Gleiter CH (2006) Multiple drug prescribing by general practitioners in a German region: implications for drug interactions and patient safety. Int J Clin Pharmacol Ther 44(11):539–547
The Digitalis Investigation Group (1997) The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 336(8):525–533
Ahmed A, Rich MW, Love TE, Lloyd-Jones DM, Aban IB, Colucci WS, Adams KF, Gheorghiade M (2006) Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J 27(2):178–186
Hunt SA, American College of Cardiology, American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) (2005) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 46(6):e1–e82
Adams KF, Gheorghiade M, Uretsky BF, Patterson JH, Schwartz TA, Young JB (2002) Clinical benefits of low serum digoxin concentrations in heart failure. J Am Coll Cardiol 39(6):946–953
Whang R, Oei TO, Watanabe A (1985) Frequency of hypomagnesaemia in hospitalized patients receiving digitalis. Arch Inter Med 145(4):655–656
Belz GG, Doering W, Munkes R, Matthews J (1983) Interaction between digoxin and calcium antagonists and antiarrhythmic drugs. Clin Pharmacol Ther 33(4):410–417
Lehmann HU, Witt E, Temmen L, Hochrein H (1978) Life-threatening digitalis intoxication with and without additional diuretic treatment. Dtsch Med Wochenschr 103(40):1566–1571
Eichhorn EJ, Gheorghiade M (2002) Digoxin. Prog Cardiovasc Dis 44(4):251–266
Smith TW, Antman EM, Friedman PL, Blatt CM, Marsh JD (1984) Digitalis glycosides: mechanism and manifestations of toxicity. Parts I and II. Prog Cardiovasc Dis 26(5):413–458; 26 (6):495–540
Oetgen WJ, Sobol SM, Tri TB, Heydon WH, Rakita L (1984) Amiodarone-digoxin interaction. Clinical and experimental observations. Chest 86(1):75–79
Nademanee K, Kannan R, Hendrickson J, Ookhtens M, Kay I, Singh BN (1984) Amiodarone-digoxin interaction: clinical significance, time course of development, potential pharmacokinetic mechanisms and therapeutic implications. J Am Coll Cardiol 4(1):111–116
Pedersen KE, Christiansen BD, Kjaer K, Klitgaard NA, Nielsen-Kudsk F (1983) Verapamil-induced changes in digoxin kinetics and intraerythrocytic sodium concentration. Clin Pharmacol Ther 34(1):8–13
Schwartz JB, Keefe D, Kates RE, Kirsten E, Harrison DC (1982) Acute and chronic pharmacodynamic interaction of verapamil and digoxin in atrial fibrillation. Circulation 65(6):1163–1170
Klein HO, Lang R, Weiss E, Di Segni E, Libhaber C, Guerriero J, Kaplinsky E (1982) The influence of verapamil on serum digoxin concentration. Circulation 65(5):998–1003
Magnani B, Malini PL (1995) Cardiac glycosides. Drug interactions of clinical significance. Drug Saf 12(2):97–109
Wrenger E, Müller R, Moesenthin M, Welte T, Frölich JC, Neumann KH (2003) Interaction of spironolactone with ACE-inhibitors or angiotensin receptor blockers: analysis of 44 cases. BMJ 327(7407):147–149
Simborg DW (1976) Medication prescribing on a university medical service-the incidence of drug combinations with potential adverse interactions. Johns Hopkins Med J 139(1):23–26
Johnston RT, de Bono DP, Nyman CR (1992) Preventable sudden death in patients receiving angiotensin converting enzyme inhibitors and loop/potassium sparing diuretic combinations. Int J Cardiol 34(2):213–215
Reardon LC, Macpherson DS (1998) Hyperkalemia in outpatients using angiotensin-converting enzyme inhibitors. Arch Intern Med 158(1):26–32
Kurnik D, Loebstein R, Farfel Z, Ezra D, Halkin H, Olchovsky D (2004) Complex drug-drug-disease interactions between amiodarone, warfarin, and the thyroid gland. Medicine (Baltimore) 83(2):107–113
Farmer JA, Torre-Amione G (2000) Comparative tolerability of the HMG-CoA reductase inhibitors. Drug Saf 23(3):197–213
Westphal JF (2000) Macrolide-induced clinically relevant drug interactions with cytochrome P-450A (CYP) 3A4: an update focused on clarithromycin, azithromycin and dirithromycin. Br J Clin Pharmacol 50(4):285–295
Amacher DE, Schomaker SJ, Retsema JA (1991) Comparison of the effects of the new azalide antibiotic, azithromycin, and erythromycin estolate on rat liver cytochrome P-450. Antimicrob Agents Chemother 35(6):1186–1190
Nahata M (1996) Drug interactions with azithromycin and the macrolides; an overview. J Antimicrobic Chemother 37(Suppl):133–142
Piacentini N, Trifirò G, Tari M, Moretti S, Arcoraci V, UVEC Group (2005) Statin-macrolide interaction risk: a population-based study throughout a general practice database. Eu J Clin Pharmacol 61(8):615–620
Stang P, Morris L, Kempf J, Henderson S, Yood MU, Oliveria S (2007) The coprescription of contraindicated drugs with statins: continuing potential for increased risk of adverse events. Am J Ther 14(1):30–40
Glassman PA, Simon B, Belperio P, Lanto A (2002) Improving recognition of drug interactions: benefits and barriers to using automated drug alerts. Med Care 40(12):1161–1171
Hansten PD (2003) Drug interaction management. Pharm World Sci 25(3):94–97
Acknowledgements
We thank all general practitioners involved in this study for collecting the clinical records. The authors have no conflicts of interest directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magro, L., Conforti, A., Del Zotti, F. et al. Identification of severe potential drug-drug interactions using an Italian general-practitioner database. Eur J Clin Pharmacol 64, 303–309 (2008). https://doi.org/10.1007/s00228-007-0394-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0394-1