Abstract
Introduction Discontinuation of medical drug treatment is a serious problem in primary care. The need for a better understanding of the processes, including physician-specific mechanisms, is apparent. The aim of this study was to analyse the association between general practitioners’ prescribing prevalence and rate of early discontinuation of different drugs consisting of, in this study, lipid-lowering drugs, antihypertensive drugs, antidepressants, antidiabetics and drugs against osteoporosis.
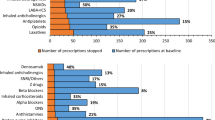
Material and methods This was a register study based on prescription data covering a 4-year period and consisting of 470,000 citizens. For each practice and group of drug, a 1-year prevalence for 2002 and the rate of early discontinuation among new users in 2002–2003 were estimated. Early discontinuation was defined as no prescriptions during the second half-year following the first prescription, with the exception of new users of antidepressants for whom it was the first half-year. Correlations were analysed using the SAS ver. 9.1PROC MIXED procedure. The association with the total prescribing prevalence (all drugs) was also analysed.
Results A total of 141 general practices were included in the study. There was a positive association between the prevalence of prescribing for the specific drugs studied (antidepressants, antidiabetics, drugs against osteoporosis and lipid-lowering drugs) and early discontinuation (r = 0.29 –0.44), but not for anti-hypertensive drugs. The analysis of the association between prevalence of all drugs and drug-specific early discontinuation showed some degree of positive association – strongest for anti-hypertensive drugs (r = 0.62) and antidepressants (r = 0.43).
Conclusion This study confirmed our hypothesis that general practitioners with high levels of prescribing attain higher rates of early discontinuation compared with colleagues with low levels of prescribing, not only with respect to antidepressants but also for various groups of drugs. A common underlying mechanism is suggested but has to be verified in future studies.
Similar content being viewed by others
Notes
Anatomical Therapeutic Chemical classification
References
Di Martino M, Degli EL, Ruffo P, Bustacchini S, Catte A, Sturani A et al (2005) Underuse of lipid-lowering drugs and factors associated with poor adherence: a real practice analysis in Italy. Eur J Clin Pharmacol 61:225–330
Foley KA, Denke MA, Kamal-Bahl S, Simpson R Jr, Berra K, Sajjan S et al (2006) The impact of physician attitudes and beliefs on treatment decisions: lipid therapy in high-risk patients. Med Care 44:421–428
Larsen J, Andersen M, Kragstrup J, Gram LF (2002) High persistence of statin use in a Danish population: compliance study 1993–1998. Br J Clin Pharmacol 53:375–378
Rasmussen JN, Chong A, Alter DA (2007) Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 297:177–186
Urquhart J (1996) Patient non-compliance with drug regimens: measurement, clinical correlates, economic impact. Eur Heart J 17[Suppl A]:8–15
World Health Organisation (WHO) (2003) Adherence to long-term therapies. Evidence for action. WHO, Geneva
Haynes RB (2002) Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev (2):CD000011
Haynes RB, Yao X, Degani A, Kripalani S, Garg A, McDonald HP (2005) Interventions to enhance medication adherence. Cochrane Database Syst Rev (4) CD000011
Hansen DG, Vach W, Rosholm JU, Søndergaard J, Gram LF, Kragstrup J (2004) Early discontinuation of antidepressants in general practice: association with patient and prescriber characteristics. Fam Pract 21:623–629
Bland JM, Altman DG (1996) Measurement error and correlation coefficients. Br Med J 313:41–42
van Houwelingen HC, Arends LR, Stijnen T (2002) Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med 21:589–624
Cohen J, West SG, Cohen P, Aiken L (2003) Applied multiple regression/correlation analysis for the behavioural sciences. Lawrence Erlbaum Assoc, Mahwah, N.J.
Gaist D, Sorensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44:445–448
Medicinal Product Statistics 1999–2003 (2004) Denmark. The primary health care sector. The hospital sector. Copenhagen, Danish Medicines Agency
Moore AT, Roland MO (1989) How much variation in referral rates among general practitioners is due to chance? Br Med J 298:500–502
Hallas J (2001) Conducting pharmacoepidemiologic research in Denmark. Pharmacoepidemiol Drug Saf 10:619–623
Morris LS, Schulz RM (1992) Patient compliance-an overview. J Clin Pharm Ther 17:283–295
Vermeire E, Hearnshaw H, Van Royen P, Denekens J (2001) Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther 26:331–342
DiMatteo MR (2004) Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care 42:200–209
Jaye C, Tilyard M (2002) A qualitative comparative investigation of variation in general practitioners’ prescribing patterns. Br J Gen Pract 52:381–386
Bradley CP (1991) Decision making and prescribing patterns–a literature review. Fam Pract 8:276–287
Acknowledgements
The Novo Foundation supported DGH and JL. We also thank Secretary Lise Stark for proof-reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hansen, D.G., Gichangi, A., Vach, W. et al. Early discontinuation: more frequent among general practitioners with high levels of prescribing. Eur J Clin Pharmacol 63, 861–865 (2007). https://doi.org/10.1007/s00228-007-0330-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0330-4